Translate this page into:
Survey of Psychosocial Issues of Nasogastric Tube Feeding in Head-and-Neck Cancer Patients
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Because of some psychosocial reasons and misbelieves regarding nasogastric(NG) tube feeding, many patients refuse for NG tube insertion.
Aim:
Primary aim was to do survey of psychological reasons for refusal of NG tube insertion and feeding in head and neck cancer patients. Secondary aim was to assess impact of psychological counseling of patient who did not accept NG tube feeding.
Method:
This cross sectional study was conducted on patients referred to palliative medicine department and needed NG tube feeding but refused for the same. We prepared our own questionnaire which includes the most common cause for enteral feeding refusal which we found during our routine OPD since last five years response to those questions were recorded. Then we did psychological counseling of patients and again we assessed patient's acceptability for NG tube feeding by Likert scale and record their response.
Results:
Most common psychological reasons for patient's refusal were “it will disrupt my body image”(88.33%), “unable to go outside/mix with people”(80%) and “dependency on others for activities”(66.66%). Post psychological counseling out of 60 patients 47 patients were agreed while 13 patients did not agree with NG tube feeding (P value 0.000062<0.5).
Conclusion:
We conclude that though NG tube feeding is necessary for some head and neck cancer, there are lots of psychosocial problem regarding its acceptance for patients. For that adequate psychological assessment and counseling is necessary for patients' acceptance, compliance and good quality of life.
Keywords
Enteral nutrition
nasogastric tube
palliative medicine
psychosocial issue
INTRODUCTION
Head-and-neck cancer (HNC) includes malignant tumor of oral and nasal cavity, lip, buccal mucosa, sinuses, pharynx, larynx, salivary gland, upper part of the esophagus, and ear.[1] The treatment options include surgery, radiotherapy (RT), and chemotherapy (CT), in combination or alone. Both RT and CT cause severe mucositis in many patients causing decrease oral intake.[2] Inadequate oral intake leads to rapid weight loss and negative impact on disease trajectory. It may decrease the response to CT and tolerance to CT and RT which leads to increase morbidity and mortality in patients.[1]
Enteral feeding through nasogastric (NG) tube for nutrition plays an important role in HNC patients with poor voluntary oral intake due to various reasons.[3] Enteral feeding is considered superior to total parenteral nutrition in patients with functional digestive tract as it has lower risk of complications and is less expensive.[456] NG tube is introduced as medical treatment, but it excludes sensory (taste of food), social, cultural pleasure, and regional traditions associated with eating food which leads to psychosocial impact on patient's life.[7] Because of these psychosocial reasons and other misbelieves regarding NG tube feeding, many patients refuse for NG tube insertion.
Hence, in this study, our primary aim was to do survey of psychological reasons for refusal of NG tube insertion and feeding in HNC patients. The secondary aim was to assess the impact of psychological counseling of patient who did not accept NG tube feeding.
METHODS
Study design and procedure
This cross-sectional study was conducted at the department of palliative medicine, state cancer institute during September 2019 to March 2020. This study was granted approval by the Institution Review and Ethical Committee.
Participants
Patients diagnosed with HNC undergoing CT, RT or both were referred to palliative medicine department at state cancer institute (during September 2019 to March 2020). Out of them, who had difficulties in taking orally or had involuntary less oral intake due to various factors such as trismus, mucositis, oro-cutaneous fistula, or mass effect needed NG tube feeding. Patients who refused for NG tube feeding were included in the study.
Exclusion
Patients <18 years and with language barrier were excluded from the study.
After obtaining inform consent, psychological assessment of 60 patients who were not agreed for NG tube feeding, was done by asking simple questionnaires (nine Questions) [Annexure 1] to identify the various reasons for refusal of NG tube feeding and recorded. There is no any standard questionnaire available for the assessment of psychosocial reasons for refusal of NG tube feeding. After reviewing the questionnaire developed by Maria Cristina and Antonio Apezetxea[8] to assess health-related quality of life in patients with home enteral nutrition, we prepared our own questionnaire which include the most common cause for enteral feeding refusal which we found during our routine outpatient department for last 5 years. The answers include multiple responses for single participant.
Then, we did psychological counseling regarding the importance of NG tube feeding, expected benefit of it and complications. We explained the practical aspects of NG tube insertion, feeding method, and long-term care of tube. We also addressed reasons for refusal. All these have been discussed sensitively without frightening the patient.
Again after counseling, we assessed patient's acceptability for NG tube feeding by Likert scale and record their response.[9]
Likert scale is fixed choice response formats designed to measure attitudes or opinions. This scale measures the levels of agreement or disagreement. It is a five point or seven point scale which is used to allow the individual to express how much they agree or disagree with a particular statement, for example, strongly agree/agree/undecided/disagree/strongly disagree.
Statistical analysis
Descriptive statistics were used for demographic data, mean, and standard deviation for continuous data and percentage for categorical variable. To analyze the impact of psychological counseling, we used percentage measurement and Chi-square test by using grapgpad.com
RESULTS
In our study, mean age of total 60 patients was 43.81 years with standard deviation ± 10.72.
Age range was from 18 to 75 years, and out of sixty patients, 46 were male and 14 were female [Table 1].
| Data | Value |
|---|---|
| Total number of patients | 60 |
| Mean age±SD | 43.81±10.72 |
| Male:female | 46:14 |
SD: Standard deviation
Majority of patient included in the study had carcinoma of buccal mucosa (40%), others had carcinoma tongue (23.33%), carcinoma central arch (10%), carcinoma postcricoid/supraglottic (8.33%), carcinoma esophagus (6%), carcinoma maxilla and hard palate (5% each), and carcinoma lip (1.66%) [Table 2].
| Diagnosis | Number of patients |
|---|---|
| Ca tongue | 14 (23.33) |
| Ca buccal mucosa | 24 (40) |
| Ca hard palate | 3 (5) |
| Ca postcricoid/supraglottic | 5 (8.33) |
| Ca central arch/mandible | 6 (10) |
| Ca esophagus | 4 (6.66) |
| Ca lip | 1 (1.66) |
| Ca maxilla | 3 (5) |
Ca: Carcinoma
They received either RT, CT or both [Table 3].
| Types of treatment | Number of patients (%) |
|---|---|
| Palliative RT | 17 (28.33) |
| Curative RT | 6 (10) |
| Palliative CT | 10 (16.66) |
| Curative CT | 8 (13.33) |
| Both RT and CT | 14 (23.33) |
| Only palliative treatment | 5 (8.33) |
CT: Chemotherapy, RT: Radiotherapy
Disease-related causes which lead to decrease voluntary oral intake are shown in Figure 1. Trismus Grade III and IV and severe mucositis were the more common reasons accounting 58.33% and 46.66%, respectively. Other causes were oro-cutaneous fistulas (26.66%), large fungating wound (35%), and large mass causing difficulty in swallowing (13.33%).
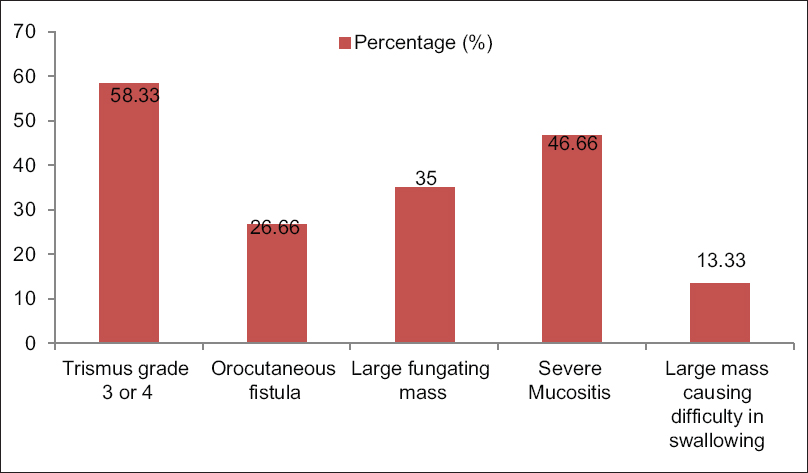
- Reason for less oral intake (multiple choices).
Most common psychological reasons for patient's refusal were “it will disrupt my body image” (88.33%), “unable to go outside/mix with people,” (80%) and “dependency on others for activities” (66.66%) [Table 4].
| Psychosocial reason | Number of patients (%) |
|---|---|
| Afraid of having tube | 37 (61) |
| Unable to go outside/mix with people | 48 (80) |
| Disrupt my body image | 53 (88.33) |
| Afraid of disease spread | 22 (36.66) |
| Discomfort/distress due to tube | 34 (56.66) |
| Able to take some liquid by the mouth | 25 (41.66) |
| Dependency on other for activities | 40 (66.66) |
| Unable to eat anything by the mouth after tube in situ | 28 (46.66) |
| Not enjoy taste of food by the mouth | 26 (43.33) |
Other reasons were “afraid of having tube (61%),” “discomfort/distress due to tube (56.66%),” “unable to eat anything by mouth after tube in situ (46.66%),” “not enjoy taste of food by mouth (43.33%),” “able to take some liquid by mouth (41.66%),” and “afraid of disease spread” (36.66%) [Table 4].
Postpsychological counseling patients' acceptability was evaluated by the Likert scale. Out of 60 patients, 47 patients (strongly agree 32 and agree 15) were agreed with NG tube feeding, whereas 13 patients (strongly disagree 1, disagree 9, and undecided 3) did not agree for NG tube feeding and required further counseling [Table 5].
| Five point Likert scale | Number of patients (%) |
|---|---|
| Strongly disagree | 1 (1.6) |
| Disagree | 9 (15) |
| Neutral | 3 (5) |
| Agree | 15 (25) |
| Strongly agree | 32 (53.33) |
| P | 0.000062 (P<0.5) |
DISCUSSION
Eating is the fundamental aspect of life which is often affected by disease and its treatment (e.g. chemo-RT) in HNC patients.[1] Problems such as difficulty in opening of mouth, difficulty and pain during chewing, acute severe mucositis, and other complications of cancer and its treatment lead to decrease voluntary oral intake and make very difficult for patients to maintain adequate hydration and nutrition.[10]
We find a significant higher number of male patients in our study because of habit of betelnut and tobacco chewing which was supported by Sharma et al.[11] study that shows positive association between tobacco use, male gender, and incidence of HNC.[11]
In our study, we found disease and its treatment-related causes which lead to decrease voluntary oral intake were trismus (58%) and severe mucositis (46.66%). Sari et al.[2] also described mucositis and trismus as the common complications in HNC patients taking radiation therapy in their review article. Other reasons in our study were large fungating wound (35%), oro-cutaneous fistulas (26.66%), and large mass causing difficulty in swallowing (15.33%).
Ehrsson et al.[1] found typical issue for patients with NG tube was that they felt embarrassed because part of the tube is visible which in turn hindered social activities. Similar to this in our study, we found the most common reasons for refusal of NG tube feeding were disrupt body image (88.33%), unable to go outside/mix with people (80%), and dependency on others for activities (66.66%). All these issues affect patients' social activities. Some other reasons we found were “afraid of having tube,” “discomfort/distress due to tube,” “unable to eat anything by mouth,” “not enjoyed taste of food by mouth,” “able to take some liquid by mouth,” and “afraid of disease spread.” Padilla and Grant[7] found most common psychosensory complaints was deprivation of favorite food. These reasons are varied according to personality characteristics and behavioral pattern of patient and family and also affected by socialcultural background.[712]
Lamparyk et al.[13] found the benefits of psychological intervention in reducing distress during medical procedure. We found statistically significant acceptance or willingness for NG tube feeding after psychosocial counseling which reduced distress in patients. Holden et al.[14] carried out a pilot study at the children's hospital Birmingham NHS trust assessing psychological preparation for NG feeding. They suggested that those who received detailed preparation had better acceptance for enteral feeding.
Rossella et al.[15] stated that psychological and educational treatment can contribute to the reduction and control of factors that may affect adaptation to the stoma and consequently on quality of life. In our study, we found that psychological counseling helps in psychosocial well-being and acceptance for NG tube feeding.
CONCLUSION
From this study, we conclude that though NG tube feeding is necessary for some HNC patients, there are lots of psychosocial problem regarding its acceptance for patients. For that adequate psychological assessment and counseling is necessary for patients' acceptance, compliance, and good quality of life.
Limitation
As psychosocial issues are different according to personality, behavioral pattern culture, regional background of patient and family, evaluation of this problems require large longitudinal multicenter study for generalization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Head and neck cancer patients' perceptions of quality of life and how it is affected by the disease and enteral tube feeding during treatment. Ups J Med Sci. 2015;120:280-9.
- [Google Scholar]
- Oral complications in patients receiving head & neck radiation therapy: A literature review. RGO Porto Alegre Out/dez. 2014;62:395-400.
- [Google Scholar]
- Gastroenteric tube feeding: Techniques, Problems and Solutions. World J Gastroenterol. 2014;20:8505-24.
- [Google Scholar]
- A clinical and economic evaluation of enteral nutrition. Curr Med Red Opin. 2011;27:413-22.
- [Google Scholar]
- Quality of life and home central tube feeding: a French prospective study in patients with head and neck or esophageal cancer. British J Cancer. 2000;82:263-9.
- [Google Scholar]
- Prospective study of percutaneous endoscopic gastrostomy tubes versus nasogastric tubes for enteral feeding in patients with head and neck cancer undergoing (chemo) radiation. Head Neck. 2009;31:867-76.
- [Google Scholar]
- Development and Validation of specific questionnaires to assess health related quality of life with home enteral nutrition: NutriQoL ® development. Patient Prefer Adherence. 2016;10:2289-96.
- [Google Scholar]
- Likert scale. 2008. Retrieved from: https://www.simplypsychology.org/likert-scale.html
- [Google Scholar]
- Prophylactic feeding tubes for patients with locally advanced head-and-neck cancer undergoing combined chemotherapy and radiotherapy-systematic review and recommendations for clinical practice. Curr Oncol. 2011;18:e191-201.
- [Google Scholar]
- Head and neck squamous cell carcinoma in young adults: A hospital-based study. Indian J Med Paediatr Oncol. 2019;40(1):18-22.
- [Google Scholar]
- Psychological aspects of artificial feeding in cancer patients. J Parenter Enteral Nutr. 1981;5:138-40.
- [Google Scholar]
- Effect of psychological preparation intervention on anxiety associated with pediatric anorectal menometry. Int J Pediatr. 2019;2019:7569194.
- [Google Scholar]
- Psychological preparation for Nasogastric tube feeding in children. Br J Nurs. 1997;6:376-81.
- [Google Scholar]
- Psychosocial distress and quality of life in ostomy patients with colo-rectal cancer: A systemic review of literature. Acta Med Med. 2018;34:1357.
- [Google Scholar]
Annexure -1







