Translate this page into:
Experiences of Living with Intestinal Ostomy: A Qualitative Meta-Synthesis
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims and Objectives:
The aim and objective of the study was to identify, compare, and synthesize published qualitative evidence to have in-depth understanding of experiences of patients living with intestinal ostomy.
Background:
Over the past two decades, there have been numerous qualitative studies published depicting intense experiences of stoma patients brought about by the need to adapt with changing conditions following stoma creation. Synthesizing the findings of these studies can improve the understanding among health-care providers of needed support and care for ostomates.
Design:
This was a qualitative meta-synthesis.
Methods:
Published articles were identified from the Medline, CINAHL, SciELO, PsycINFO, PubMed, WOS, Google Scholar and a hand search through selected journals published since 2000, and from references lists. Thirteen articles were selected using the predefined criteria.
Results:
A total of 222 patients, aged between 14 and 83 years from 13 studies, were identified for data collection. Ninety-seven were male and the rest of them were female. The themes identified were physical problems, psychological issues, social relations, environmental impact, and coping and adaptation to stoma.
Conclusions:
The findings of the study identified numerous challenges and limitations in the life of patients with stoma. However, improving their skills of using problem-solving coping strategies and their interactions with other ostomates can help them to live a better and well-adjusted life.
Keywords
Challenges with stoma
intestinal stoma
living experiences
quality of life
INTRODUCTION
The word “stoma” has come from the Greek word which means the mouth or opening. One well-known form of an artificial stoma is an intestinal ostomy, which is a surgically created opening in the large intestine or ileum that allows the removal of feces out of the body to drain into a pouch or other collection device.[1] Intestinal ostomy is a procedure that is implemented to treat several conditions, including acute diverticulitis, rectal cancer, trauma, or inflammatory bowel disease.[12] This therapeutic approach can be temporary or permanent and creates many challenges in terms of quality of life and functioning. Although ostomy is a life-saving surgery, there is immense evidence of maladjustment in ostomates throughout the world.[3]
The presence of a stoma enforces numerous changes and limitations in the life of the patient. These changes start, the moment the disease or condition is discovered, triggering different patient coping behaviors. People with a new ostomy generally pay more attention to the negative aspects of the stoma and its effect on his/her body image. At first, many patients would rather like to die than living with the stoma. Over the days, they start to realize that having an ostomy means gaining the opportunity for a new life. In this sense, it is noticed that, after an ostomy, individuals thus treated experience moments of emotional or psychological change that, by affecting the quality of life, self-esteem, body image, and even their sexuality, can generate anxiety and even depression.[456]
When subjected to this surgery, these people start living a different experience where their standard of living and rhythm of life begin to change. Their desires and values are often not fulfilled nor respected; they feel rejected, seeking seclusion because of the odor and elimination of feces through the abdomen.[7]
In view to complexity of the theme and intense experiences of stoma patients brought about by the need to adapt with changing condition, the meta-synthesis was done to explore the available evidence to have in-depth understanding of phenomenon.
Objective
The objective of the study was to identify, compare, and synthesize published qualitative evidence to have in-depth understanding of experiences of living with intestinal ostomy.
METHODS
A qualitative systematic review and meta-synthesis design was employed in the study. The process of meta-synthesis consisted of three steps: (a) identifying the published papers for inclusion and determination of their relevance, (b) quality appraisal of published papers and data extraction, and (c) summarizing and synthesis of findings.
Identifying the published papers for inclusion and determination of their relevance
Published articles were identified from the Medline, CINAHL, SciELO, PsychINFO, PubMed, WOS, Google scholar and a hand search through selected journals published since 2000, and from references lists. The keywords used for search were “Quality of Life,” Intestinal Stoma, “Living experiences,” and “challenges with stoma.” The suitability of the study for inclusion was determined by the following screening questions: (1) Do the report findings of paper involve qualitative methods for data collection and analysis? and (2) Is the focus of paper relevant to the synthesis topic?
Inclusion criteria
-
Qualitative studies with phenomenological, grounded, ethnographic, and descriptive research design
-
Studies with adult patients having intestinal stoma as participants.
Exclusion criteria
-
Studies including patients with significant language impairment, cognitive impairment, other major comorbid medical difficulties, or with a past history of psychiatric problems
-
The studies reporting focus from the perspectives of caregivers of ostomates
-
Studies reporting use of mixed method approach, quantitative approach, or case studies.
Quality appraisal and data extraction
Two main criteria were used in the evaluation and quality appraisal of qualitative research, i.e., credibility and relevance. Studies meeting inclusion and exclusion criteria were subjected to further scrutiny using the following series of seven questions.
Credibility
-
Were sampling strategies and data collection methods explained?
-
Was method of data analysis discussed and enough data provided to allow the reader to determine support of the data to the interpretations (auditability)
-
Did the authors acknowledge the influence of the research process and the presence of researcher including the role of prior biases, assumptions and experience, on the collected data (reflexivity)?
-
Has appropriate attention given to negative cases and to contradictory data?
-
Had the author explored alternative, plausible explanations for the data collected and incorporate a range of different perspectives (fair dealing).
Relevance
-
Was information regarding participants, settings, and context provided (transferability)?
-
Did the author broadly discuss the findings and proposed generalization of findings and/or suggest the scope of future research (analytic generalization)?
Summarizing and synthesis
Condensing labels were used to summarize and list down the perspectives of various studies. Themes identified by researchers were noted and cross-checked against their cited data. After summarization of data in each paper by labels, these were charted under unifying headings. Concepts were developed that synthesized the findings of all the papers included in the meta-synthesis.
RESULTS
Identifying the published papers for inclusion and determination of their relevance
The search identified 282 papers, of which 13 papers[891011121314151617181920] had potential relevance to the review question [Figure 1].
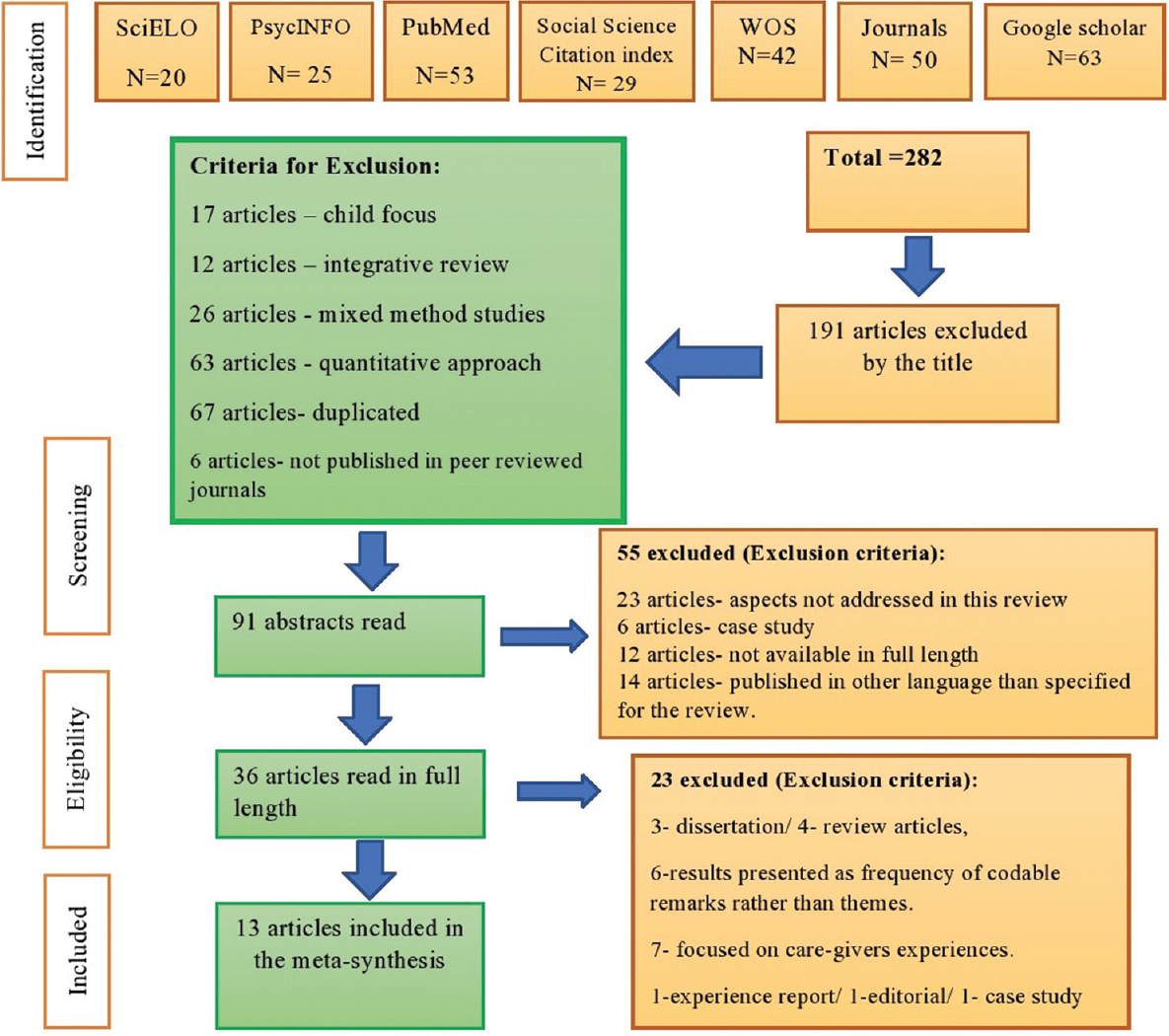
- Flow diagram of the selection process of articles of the meta-synthesis according to the preferred reporting items for systematic reviews and meta-analyses
Quality appraisal and data extraction
All 13 included studies satisfied the criteria for quality appraisal and data extraction [Table 1].
| Author’s name | Year of publication | Title of the study | Subjects | Themes |
|---|---|---|---|---|
| Alwi F et al. | 2018 | Quality of life of persons with permanent colostomy: a phenomenological study | 12 patients with permanent colostomy having end stoma | Limitation in daily living activities, limitations in marital relations and social relationship with others, negative feelings about having the colostomy, financial difficulties, increasing demands of living with colostomy, changes in the needs of rest, physical and expectation of complications, and hoping to live a normal life after colostomy |
| Ceylan H, Vural F | 2017 | Living with stoma - A phenomenological study | 19 patients having a stoma for at least 3 months | First encounter, challenges, and coping |
| Thorpe G et al. | 2016 | Adjusting to bodily change following stoma formation: A phenomenological study | 12 participants who had undergone stoma creation surgery | Changes in bodily appearance, disruption in bodily function, altered bodily sensation |
| Shaffy et al. | 2014 | Psychosocial experiences of the patients with colostomy/ileostomy: A qualitative study | 40 patients with colostomy/ileostomy with minimum time period of 6 weeks after surgery | Embarrassment with the ostomy appliance, feeling of disgust and alienation towards the body and feelings of uncleanliness with the ostomy appliance |
| Danielsen A K et al | 2013 | Learning to Live with a Permanent Intestinal Ostomy: Impact on Everyday Life and Educational Needs | 15 patients with permanent colostomy or ileostomy | Being different, training in living a life with a stoma |
| Danielsen AK et al. | 2012 | Impact of a temporary stoma on patients’ everyday lives | 7 patients with temporary stoma | Life before and after creation of the “stoma,” “uncertainty” and “mastery and personality,” putting life on hold |
| Shaffy et al. | 2012 | Physical, nutritional and sexual problems experienced by the patients with colostomy/ileostomy: A qualitative study | 40 patients with colostomy/ileostomy with minimum time period of 6 weeks after surgery | Physical problems, psychological problems, sexual problems |
| Dabirian A et al. | 2010 | Quality of life in ostomy patients: A qualitative study | 14 patients having had an ostomy in place for at least 6 months | Physical problems related to colostomy, impact of colostomy on psychological functioning, social and family relationships, travel, nutrition, physical activity, and sexual function, as well as religious and economic issues |
| Honkala S et al. | 2009 | Living with an ostomy: Women’s long term experiences | Seventeen women with stoma | Bodily restraints, I as a woman, reconciliation to a changed life, adaptation to daily life |
| Barnabe NC et al. | 2008 | Coping strategies of ostomized individuals | 11 ostomized subjects | I did not choose it; I had to accept it and I have to live with the ostomy |
| Nicholas DB et al. | 2008 | Struggles, strengths, and strategies: an ethnographic study exploring the experiences of adolescents living with an ostomy | 20 adolescents with an ostomy | Body intrusion and body image challenges, decreased independence and control, secrecy: Considerations in deciding whether to tell others about the ostomy, adjustment over time, challenges for the family, Sources of strength: Family and friends, benefits and growth |
| Annells M | 2006 | The experience of flatus incontinence from a bowel ostomy: A hermeneutic phenomenology | Six people with a bowel ostomy from a city in Australia | I am undignified, I am a secret, I am always with gas, I am not myself alone, I am without choice, I am a seeker of control, I am the smell, I am not normal, and I am living a life-sort of |
| Persson E., Hellstrom AL | 2002 | Experiences of Swedish Men and Women 6-12 Weeks after Ostomy Surgery | Nine patients with stoma for at least 6 months | Alienation from the body, altered body image, influences on sexual life, uncertainty, influences on social life, influences on sports and leisure activities, and physical problems |
Summarizing and synthesis
A total of 222 patients, aged between 14 and 83 years, from 13 studies were included in the study. Ninety-seven were male and the rest of them were female. Studies from 2000 to 2020 were included in the meta-synthesis.[891011121314151617181920] There were 11 phenomenological studies and 2 exploratory ethnographic studies. The method of data collection in the included studies was self-report technique, interviews using semi-structured questionnaire, open-ended questions, focused group interviews, and in-depth interview technique. The themes identified were physical problems, psychological issues, social relations, environmental impact, and coping and adaptation [Table 2].
| Major themes | Studies | Subthemes |
|---|---|---|
| Physical Problems |
Alwi F et al. (2018), Ceylan H, Vural F (2017), Thorpe G et al. (2016), Shaffy et al. (2014), Danielsen A K et al. (2013), Danielsen A K et al. (2013), Dabirian A et al. (2010), Honkala S et al. (2009), Nicholas DB et al. (2008), Annells M (2006), Persson E., Hellstrom AL (2002) | Limitation in physical and recreational activities Alteration in body image Issues in travelling Sleep disturbance Nutritional issues Alteration in clothing style Complications of stoma |
| Psychological Issues |
Alwi F et al. (2018), Thorpe G et al. (2016), Danielsen A K et al (2013), Shaffy et al. (2014), Dabirian A et al. (2010), Honkala S et al. (2009), Annells M (2006) | Impaired psychological wellbeing Comparison with normal people |
| Social Relations |
Alwi F et al. (2018), Ceylan H, Vural F (2017), Thorpe G et al. (2016), Shaffy et al. (2014), Danielsen AK et al. (2013), Dabirian A et al. (2010), Annells M (2006), Nicholas DB et al. (2008), Persson E., Hellstrom AL (2002) | Marital and sexual relationship Relationship with family friends and others |
| Environmental Impact |
Alwi F et al. (2018), Ceylan H, Vural F (2017), Thorpe G et al. (2016), Shaffy et al. (2014), Danielsen AK et al. (2013), Dabirian A et al. (2010), Honkala S et al. (2009) | Financial burden Lack of tailored counselling services |
| Coping and adaptation | Alwi F et al. (2018), Ceylan H, Vural F (2017) Danielsen A K et al. (2013), Dabirian A et al. (2010), Honkala S et al. (2009), Barnabe NC et al. (2008), Nicholas DB et al (2008), Annells M (2006) | Use of problem-solving coping strategies Learning in group |
Physical problems
Limitation in physical and recreational activities
Majority of the patients experienced lack of energy leading to a reduction in their usual activities. It affected their person's life style, ability of self-care, and care of family members. Patients also reported limitation in lifting heavy objects due to weakness and site of stoma.[891415] Stoma was also perceived as an obstacle in various recreational activities such as visiting to theater or cinema, opting for swimming, or just to have a day outing for shopping, as it is difficult to find public convenience for bag emptying.[9101112161820]
Alteration in body image
Stoma, stoma appliance, and abdominal wounds changed perceived appearance of ostomates. Patients reported feeling of shame and horror while having first sight of stoma. They viewed their body image as deeply unattractive and avoided looking at stoma. Temporary or permanent changes in abdominal shape were also reported to be disheartening.[10161820]
Issues in travelling
Difficulty in cleaning, emptying, or changing the stoma bag during long travels was the main issue hindering ostomates to plan for long journeys. Fear of passing of flatus in public transport further reported to restrict the travel.[810141516]
Sleep disturbance
Patients explained an increased need for resting as they never feel free while sleeping and often have to be awake in the event of leaking of stoma bag. They had to avoid few sleeping positions as per the site of stoma further adding to sleep disturbances.[89121416]
Nutritional issues
One major problem reported was a need to change diet to avoid obstruction and lack of proper information about needed dietary changes. Patients reported to have discomfort and problems such as belching, nausea, or gas formation after consuming some of the food items. The need to leave their favorite dishes to manage the stoma functioning was described as distressing.[9141516]
Alteration in clothing style
Ostomates mentioned impaired self-identity, as they could not dress like before, nicely and fashionably. They were forced to avoid tight fitting clothes as it reveals their stoma bag. Few positions of stoma made it compulsory to wear loose and baggy clothes to cover stoma site so that no one can see it. Furthermore, ostomy placed at the site of waistband added to problem of scraping and irritation, necessitating change in clothing style.[10131416]
Complications of stoma
Frequent irritation, itching, and rash around the ostomy site were common reported complication by the ostomates. Patients were severely discommoded by the problem of passing flatus and with the fear of passing it in the public.[1014161720]
Psychological issues
Impaired psychological well-being
Patients mentioned to suffer from some degree of cognitive and mental problems following stoma creation. Feeling of uncertainty of future further added to mental distress. Patients reported negative feelings about themselves and stoma creation such as guilt, feeling afraid, feeling alone, shame, getting upset easily, and remarked feeling of inferiority.[8101219] They often felt lack of confidence; few revealed events of mental break down and receiving psychiatric therapy for major depression.[101112131519]
Comparison with normal people
The limitations imposed by the stoma enhanced comparison with normal persons in surroundings such as family members and friends adding to feeling of jealousy, feeling of incompleteness, and inferiority, leading to mental distress and social isolation. Dependency on others for self-care further contributed to this comparison.[111416]
Social relations
Marital and sexual relationship
Majority of the patients described limited or no sexual intercourse following stoma creation, which added to the fear getting separated or divorced. Although many felt their partner to be supportive and helpful, but still they perceived changes in relationship with their partners.[891520] Problems with erection in males and fear of looking unattractive with stoma among females were common factors contributing to the avoidance of sexual activities.[89141520]
Relationship with family, friends, and others
Some of the patients mentioned that their family and friends accepted the stoma and tried to cooperate; however, others felt that they tried to maintain distance and avoid the ostomates. Patients felt more comfortable and less depressed when they received support of family and friends. Ostomates reported preference to avoid family or social gatherings because of fear of offensive gas emission.[8910151619] Further dilemma of disclosing about stoma and self-imposed limits about disclosures to the gathering restricted their participation. Feeling of getting nervous and upset easily, feeling of inferiority, and shame made public interaction very difficult for the patients, further adding to social isolation.[91011131820]
Environmental impact
Financial burden
Patients reported that they had to either change or leave their job following stoma creation, which affected their income. Various complications of stoma hindered working hours and increased need of sick leaves, further decreasing income. Moreover, disease-related costs, for example, buying bags, gloves, and stoma care kits, enhanced financial burden.[8910141516]
Lack of tailored counseling services
Patients experienced that follow-up counseling services were not tailored to their specific needs related to stoma care and complication management. Lack of regular meetings and failure of coordinator to address personal questions were major concerns of patients.[121618]
Coping and adaptation
Use of problem-solving coping strategies
Patients reported to focus on problem-solving strategies to deal with various limitations, to establish relationship with family members and significant others, and to have continuity of daily activity performance. The personal competence of being positive and experimenting with different ways to resolve limitations had a great influence on adaptation process.[8913151617]
Learning in group
Learning in group with and from another person with stoma was mentioned as extreme helpful to enable individual to manage stoma. Patients reported to have improved mood and ability to relax when they got opportunity to interact with other ostomates. Experimenting and planning activities together was mentioned to solve many problems of every day's life with stoma.[12161820]
DISCUSSION
The main focus of the meta-synthesis was to assess experiences of living with intestinal ostomy which were categorized in various themes as physical problems, psychological issues, social relations, environmental impact, and coping and adaptation. The findings of the meta-synthesis exhibited the complexity and diversity of experiences of individuals living with intestinal stoma. When it is concerned with physical problems, patients reported limitation in numerous aspects such as limitation in physical and recreational activities, inability to opt for long journeys, sleep disturbance causing increased felt need for rest, inability to consume various food items, imposed need to change the clothing style, and necessity to deal with frequent complication of stoma (Alwi F et al. (2018), Ceylan H, Vural F (2017), Thorpe G et al. (2016), Shaffy et al. (2014), Danielsen A K et al. (2013), Danielsen A K et al. [2012), Dabirian A et al. [2010), Honkala S et al. [2009), Nicholas DB et al. [2008), Annells M [2006), Persson E., Hellstrom AL [2002). The fear of leakage, gas, and obstruction along with a lack of energy imposed various limitation in the life of ostomates.
Stoma was found to have devastating psychological impact on ostomates. Negative feelings about stoma creation and themselves such as guilt, feeling afraid, feeling alone, shame, getting upset easily, and remarked feeling of inferiority impaired psychological well-being of patients (Alwi F et al.(2018), Thorpe G et al.(2016), Danielsen A K et al.(2013), Shaffy et al.(2012), Dabirian A et al.(2010), Honkala S et al.(2009), Annells M (2006).
Limitations caused by stoma imposed social isolation among ostomates. However, the support of family and friends was positively appreciated by patients. Concern about sexual life and relationship stability was more evident and emphasizes counseling needs in this area. (Dabirian A et al.(2010), Shaffy et al.(2012). Financial burden was other added concern because of inability to carry out routine job, need to either leave or change the job, and increased need of sick leaves. Bearing expenses of routine stoma care further adds to this stress. (Alwi F et al.(2018), Dabirian A et al.(2010), Honkala S et al.(2009).
However, most of the patients reported use of problem-solving coping strategies to deal with these limitations, adding to their personal competence of being positive and proactive, strongly influencing their rehabilitation process. (Barnabe NC et al.(2008), Nicholas DB et al.(2008), Annells M (2006). Various interventional studies enlightened innovative methods of such preoperative intensive education combined with traditional postoperative education (Chaudhri et al. 2005, Bryan and Dukes 2010),[2122] use of multimedia in patients' teachings (Lo et al. 2011),[23] follow-up using telemedicine or telenursing services (Bohnenkamp et al. 2004)[24] to improve self-care capacities of ostomates. Individual-based folAlow-up counseling session can further enhance the patient's ability to combat imposed challenges by stoma.[25]
Limitation and recommendations
The meta-synthesis focused on the qualitative evidence only. Although qualitative evidence provides better understanding and insight into experiences of patients with stoma, the addition of quantitative evidence can enhance the degree of certainty with the help of quantitative analysis. This study recommends and emphasizes the need for meta-analysis of quantitative evidence to have in-depth knowledge of consequences of having a stoma. Furthermore, the studies included in the meta-synthesis focused on the limitation related to stoma but lacked exploration on techniques to manage those limitations to improve health-related quality of life or to reduce cost. The study recommends an additional research to assess the effect of group learning on coping and adaptation to stoma among ostomates and to explore further techniques to ease the life of ostomates.
CONCLUSIONS
The findings of the study identified a numerous challenges and limitations in life patients with stoma. However, improving their skills of using problem-solving coping strategies and their interactions with other ostomates can help them to live a better and well-adjusted life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Digestive System Principles of Anatomy and Physiology (3rd ed). New Jersey: Elsevier Publication, Von Hoffman Press; 2003. p. :881-95.
- Survival and psychosocial adjustment to stoma surgery and non-stoma bowel resection: A 4-year follow-up. Psychosomatic Res. 1997;42:235-44.
- [Google Scholar]
- Coping and acceptance: The greatest challenge for veterans with intestinal stomas. J Psychosom Res. 2009;66:227-33.
- [Google Scholar]
- Quality of life of stoma patients: Temporary ileostomy versus colostomy. World J Surg. 2003;27:421-4.
- [Google Scholar]
- Quality of life in patients with stomas: The Montreux Study. Ostomy Wound Manage. 2003;49:48-55.
- [Google Scholar]
- Quality of life assessment in stoma patients in a tertiary care ospital in South India: A cross- sectional study. Int Surg J. 2017;4:2037-41.
- [Google Scholar]
- Quality of life of person with permanent colostomy: A Phenomenological study. J Coloproctol. 2018;8:295-301.
- [Google Scholar]
- Adjusting to bodily change following stoma formation: A phenomenological study. Disabil Rehabil. 2016;38:1791-802.
- [Google Scholar]
- Psychosocial experiences of the patients with colostomy/ileostomy: A qualitative study. Indian J Soc Psychiatry. 2014;30:28-34.
- [Google Scholar]
- Impact of a temporary stoma on patients' everyday lives: Feeling of uncertainty while waiting for closure of the stoma. J Clin Nurs. 2013;22:1343-52.
- [Google Scholar]
- Learning to live with a permanent intestinal ostomy: Impact on everyday life and educational needs. J Wound Ostomy Continence Nurs. 2013;40:407-12.
- [Google Scholar]
- Physical, nutritional and sexual problems experienced by the patients with colostomy/ileostomy: A qualitative study. Nurs Midwifery Res J. 2012;8:210-22.
- [Google Scholar]
- Quality of life in ostomy patients: A qualitative study. Patient Prefer Adherence. 2010;5:1-5.
- [Google Scholar]
- Living with an ostomy: Women's long tern experiences. Vard I Norden. 2009;92:19-22.
- [Google Scholar]
- Dell'Acqua MCQ.Coping strategies of ostomized individuals. Rev Latino-Am de Enfermagem. 2008;16:712-9.
- [Google Scholar]
- Struggles, strengths, and strategies: An ethnographic study exploring the experiences of adolescents living with an ostomy. Health Quality Life Outcomes. 2018;6:114.
- [Google Scholar]
- The experience of flatus incontinence from a bowel ostomy: A hermeneutic phenomenology. J Wound Ostomy Continence Nurs. 2006;33:518-24.
- [Google Scholar]
- Experiences of Swedish men and women 6 to 12 weeks after ostomy surgery. J Wound Ostomy Continence Nurs. 2002;29:103-8.
- [Google Scholar]
- Preoperative intensive, community-based vs.traditional stoma education: A randomized, controlled trial. Dis Colon Rectum. 2005;48:504-9.
- [Google Scholar]
- The enhanced recovery programme for stoma patients: An audit. Br J Nurs. 2010;19:831-4.
- [Google Scholar]
- Multimedia education programme for patients with a stoma: Effectiveness evaluation. J Adv Nurs. 2011;67:68-76.
- [Google Scholar]
- Traditional versus telenursing outpatient management of patients with cancer with new ostomies. Oncol Nurs Forum. 2004;31:1005-10.
- [Google Scholar]
- Adjustment to colostomy: Stoma acceptance, stoma care self-efficacy and interpersonal relationships. J Adv Nurs. 2007;60:627-35.
- [Google Scholar]






