Translate this page into:
Peaceful End of Life in an Unviable Newborn: A Case Report
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The limit of viability is a period of uncertainty regarding the prognosis and treatment, where palliative care (PC) is important to dignify death, although, in several countries, they are not implemented as in Colombia. The peculiarities of newborns make PC differ from care at other stages of life and which are rarely accepted by professionals who consider them overwhelming. The case of a newborn of 23 weeks of gestation is exposed where nursing care is revealed to the newborn and his family according to the theory of the peaceful end of life (PEL). The theory of the PEL is useful in the development of neonatal PC, which must be differentiated, improving well-being, and family support. Furthermore, health systems must recognize emotional risks for professionals.
Keywords
Extremely premature
fetal viability
infant
infant
newborn
nursing care
palliative
INTRODUCTION
In Colombia, 2499 newborns (NB) were born between 22 and 27 weeks of gestation during 2017 (extremely premature),[1] in a period that includes the limit of the viability, where the prognosis of life and clinical treatment are uncertain. Health professionals move between therapeutic incarnation, their obligation to save lives and the uncertainty of the benefits of palliative care (PC) in such small humans. This case reveals the nursing care framed in the theory of the peaceful end of life (PEL) and reflects on the care of ultra-premature NB.
CASE REPORT
It is presented using the nursing situation methodology proposed by Boykin and Schoenhofer;[2] influenced by modern philosophies that recognize other forms of knowledge and board the human in an integral way.
The calm of the shift was interrupted by the arrival of a patient with 23 weeks of gestation, who needed an emergency cesarean section, by a rupture of membranes of a week of evolution with the signs of infection. Based on the calculated estimated weight, it was expected that the newborn would not be so immature, the health team agreed to be ready for revival.
When Jerome was born, the team agreed in that was better not to revive him for his immaturity. Jerome remained in deep apnea, hypotonic, and cyanotic, however, with the minimum stimulus of taking anthropometric measurements, he began to sob and cry. He had his eyes fused and weighed 600 g. He was crying with such vitality that I asked again the conduct to follow; the pediatrician repeated that the baby was very immature, and it was not fair to subject him to an infamous quality of life (decision that was taken with the parents).
Once the medical evaluation was completed, the entire team left the site. I started talking to him, I performed all the protocol prophylaxis, I cleaned him, I got a nappy, I made a hat with a sterile compress, and I wrapped him with hot fields. I spoke with Jerome's father and facilitated his entry into the room, confirmed his religious beliefs with him and I applied sterile water to him making the sign of the cross, in a ritual that resembles the baptism of Catholics. The very shocked father left quickly. Again, Jerome and I alone, he looked cyanotic and with dyspnea, I wanted to run away and not hear his crying, but I stayed there to accompany him, to make his position changes, monitor his temperature and all those things proper to the attention of the NB. Three hours later, before finishing my shift, I handed him to my colleagues in the neonatal unit, saturating 69% and with great vitality in his expression. Finally, the newborn died in his mother's arms, 7 h after birth.
On leaving, I was able to release what I felt, I needed a few minutes of crying to understand that my profession is beautiful and demanding, requires strength and personal balance to face difficult decisions, but each one of the lived experiences broadens the vision of care and edifies a more integral human being.
The case allows to identify as protagonists the NB, his family and the nurse; transcending the positivist vision of the human divided into parts and the professional as an observer that does not change with the experience of caring. The focus is the PEL theory, as can be seen in Figure 1.[34]
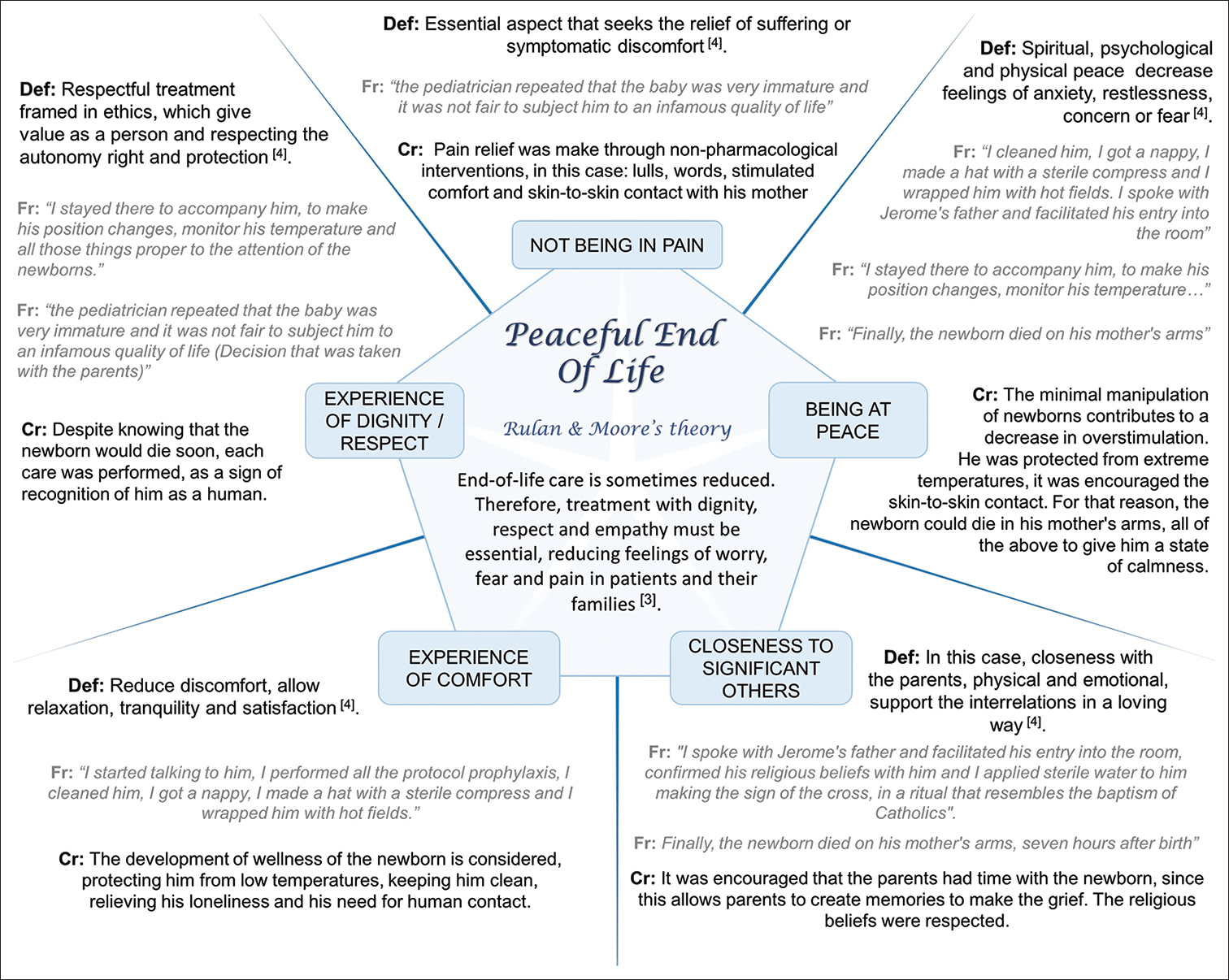
- Peaceful end of life theory in the case. The five concepts of the theory are defined; show a fragment of the case and the nursing care that was performed. Def: Definition, Fr: Case fragment, Cr: Care
DISCUSSION
An element of PC is assistance for dignified death. Colombia decriminalizes assisted death in adults in 1997 and 20 years later materializes it; being the only country in Latin America to legislate on this aspect, but children are not included yet. Assisted death is not the only way to dignify death; however in such small and fragile bodies, the limit between comfort and assistance can be a very fine line. This circumstance creates anguish in health professionals, tension and distancing of PC; socially, the death of those who have just been born is not conceived. Therefore, neonatal and PC care is poorly boarded and defined in the care units.
The peculiarities of NB do not allow PC activities to be inferred from care at other stages of life. In Figure 2[321] are the arguments that support the care activities reflected in the case.

- Scientific evidence of the care oriented by peaceful end of life theory
The attention of the NB to the limit of viability requires a look focused on PC, to avoid suffering and dignify life and death.[2223] The role of the nurse is: to support families for decision making that helps clear information; take care not only of physiological aspects but also participate in the defense of the patient and allow time, closeness and intimacy between the parents and the newborn;[23] as well as the other environmental aspects that favor tranquility and respond to the individual needs of each family.
The proximity to suffering and death leads professionals to emotional overload, intense sadness, and a sense of loss, so they feel fear of PC, relating to the lack of motivation.[2224] This is seen as one of the most stressful activities for nurses and can be a cause of disinterest in the care, as they often experience great frustration. However, sensitive and differentiated care of families living this painful experience should be a priority.
Another circumstance that concerns health staff is the continuous balance between the beneficence and maleficence of treatments or the limitation of therapeutic efforts. As well as the constant reflection on the elements that constitute the well-being and quality of life of the NB.[19]
It should not be forgotten that the case on which it is reflected, exposes a highly sensitive moment where human treatment must be gentle, considerate, and honest.[25] These require that the health staff involved receive frequent training, and this topic is involved in the agendas of the neonatal care units.
CONCLUSION
-
Neonatal PC is important to promote a dignified death in those who have just been born
-
The care must be multifactorial, sensitive, and differentiated, improving the well-being of the NB, and promoting family support
-
Professionals working in neonatal units must commit to the attention of NB to the limit of viability and health systems must recognize the risks to the emotional health of professionals and the needs of special training
-
The PEL theory is useful in generating the comprehensive neonatal or perinatal PC plan and favors evidence-based practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Demography and Population Statistics. Available from: https://wwwdanegovco/indexphp/estadisticas-por-tema/demografia-y-poblacion/nacimientos-y-defunciones
- 2013. Health Care System Transformation for Nursing and Health Care Leaders: Implementing a Culture of Caring. Springer Publishing Company; ProQuest Ebook Central Available from: http://ebookcentralproquestcom/lib/unal/detailactiondocID=1600439
- Nursing theories for research and health care practice in palliative care. Revista Latinoamericana de Bioéica. 2016;17:60-79.
- [Google Scholar]
- Theory construction based on standards of care: A proposed theory of the peaceful end of life. Nurs Outlook. 1998;46:169-75.
- [Google Scholar]
- Stress and pain in the perinatal period: Pathophysiology, consequences and management Avances de Investigación en Salud a lo largo del ciclo vital. 2018;2nd:155-62.
- A systematic review of behavioral and environmental interventions for procedural pain management in preterm infants. J Pediatr Nurs. 2019;44:22-30.
- [Google Scholar]
- Oral glucose and listening to lullaby to Decrease pain in preterm infants supported with NCPAP: A Randomized controlled trial. Pain Manag Nurs. 2019;20:54-61.
- [Google Scholar]
- Effect of non-nutritive sucking and sucrose alone and in combination for repeated procedural pain in preterm infants: A randomized controlled trial. Int J Nurs Stud. 2018;83:25-33.
- [Google Scholar]
- Randomised crossover trial showed that using breast milk or sucrose provided the same analgesic effect in preterm infants of at least 28 weeks. Acta Paediatr. 2018;107:436-41.
- [Google Scholar]
- Assessment of continuous pain in newborns admitted to NICUs in 18 European countries. Acta Paediatr. 2017;106:1248-59.
- [Google Scholar]
- Objective assessment of induced acute pain in neonatology with the newborn infant parasympathetic evaluation index. Eur J Pain. 2018;22:1071-9.
- [Google Scholar]
- Do pain measurement instruments detect the effect of painreducing interventions in neonates A systematic review on responsiveness. 2018. Pain. 46:257-69. Available from: https://wwwcambridgeorg/core/product/identifier/S0047404517000161/type/journa l_article
- [Google Scholar]
- 2015. External Circular 037 of 2015 Issued Jointly by the National Administrative Department of Statistics (DANE) and Ministry of Health and Social Protection of Colombia. Available from: https://wwwminsaludgovco/sites/rid/lists/bibliotecadigital/ride/de/dij/circular-externa-conjunta-0037-de-2015pdf
- Ethics and palliative care in the perinatal world. Semin Fetal Neonatal Med. 2018;23:35-8.
- [Google Scholar]
- Decision-making at the limit of viability: The Austrian neonatal choice context. BMC Pediatr. 2019;19:204.
- [Google Scholar]
- Delivery room deaths of extremely preterm babies: An observational study. Arch Dis Child Fetal Neonatal Ed. 2017;102:F98-103.
- [Google Scholar]
- Interventions to hypothermia at birth in preterm and/or low birth weight infants. Cochrane Database Syst Rev. 2018;2:CD004210.
- [Google Scholar]
- The Nursing care for newborns with low weight. Revista Uruguaya de Enfermería. Revista Uruguaya de Enfermerí. 2014;9:23-30.
- [Google Scholar]
- Nutrition and hydration in newborns: Limiting treatment decisions. Cuad Bioéica. 2015;26:241-9.
- [Google Scholar]
- Non-sedation of the neonate for radiologic procedures. Pediatr Radiol. 2018;48:524-30.
- [Google Scholar]
- Peri-viability: Limits of prematurity in a regional hospital in the last 10 years. An Pediatr (Barc). 2014;80:159-64.
- [Google Scholar]
- Bioethics in end-of-life decisions in neonatology: Unresolved issues. An Pediatr (Barc). 2017;87:e2.
- [Google Scholar]
- A proposed model for perinatal palliative care. J Obstet Gynecol Neonatal Nurs. 2017;46:904-11.
- [Google Scholar]
- Brazilian neonatal nurses’ palliative care experiences. J Perinat Neonatal Nurs. 2018;32:E3-10.
- [Google Scholar]






