Translate this page into:
Deaths in the Emergency Department: An Assessment of Patient's End-of-Life Trajectory and Quality of Care
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
A considerable proportion of deaths occur in the emergency department (ED), and yet a palliative care approach is not well integrated. End-of-life patients often either receive invasive care, or their care is neglected due to being perceived as not being “acutely” ill. While a small proportion of these deaths are of an unpredictable nature, most have identifiable dying trajectories: (a) advanced cancer, (b) organ failure, (c) chronic frailty, and (d) sudden death.
Aims:
This study aims (1) to determine the incidence, nature and illness trajectory of deaths in the ED; (2) to examine to which extent end of life discussions took place; (3) to analyze the aggressiveness of the care; and (4) to determine if palliative care services were being consulted.
Methods:
This retrospective study was conducted in a large tertiary hospital and cancer center in Saudi Arabia over a 1 year period. Data collection included demographics, clinical presentation, end-of-life care, and palliative care involvement.
Results:
Our study included 103 patients. Cancer was the main diagnosis (45.7%). Deaths were related to advanced cancer (45.6%), followed by organ failure (29.1%), sudden death (13.6%), and chronic frailty (11.7%,). 35.9% had a documented Do-Not-Attempt-Resuscitation (DNAR) status prior to admission. 51.5% received aggressive treatments. Palliative care was consulted for 19.4% of patients, among which 50% of referrals occurred 1 day prior to death.
Conclusions:
End-of-life care discussions tend to occur late in the disease trajectory; a number of patients are subjected to aggressive treatments, and palliative care services remain underutilized. An early, integrated and collaborative approach is warranted to address the challenges of end of life care.
Keywords
Death
emergency
end of life
palliative care
Saudi Arabia
INTRODUCTION
A considerable proportion of deaths occur in the emergency department (ED), and yet, palliative care is not well integrated into this setting.[1234567] Several obstacles have been identified: limited knowledge and understanding about the ED physician roles in providing palliative care, lack of knowledge about pain and symptom control, gaps in understanding legal and ethical issues around decision-making at the end of life (EoL), limited information available about the patient's condition upon arrival, and logistical challenges related to the ED environment itself.[3] The environment is often characterized by narrowed spaces, lack of privacy for patients and families, multiple noises, and staff rushing from one patient to another to attend to urgent situations. The management of the dying process has not traditionally been considered a core aspect of emergency medicine, and EDs tend to have more of a rescue-oriented culture.[18] Discussions about patients' goals of care do not always take place in this setting.[3] The ED physician may be unaware of the patient's wishes and discussions that have taken place in the outpatient setting, as well as the life expectancy. Without these information the default course of action is often “to do everything.” Finally, we are witnessing that the ED has also become a place where exacerbations of life-limiting illnesses and chronic conditions are being actively managed.[9] A growing number of patients admitted to the ED at the EoL are found to be receiving increasingly invasive care.[210] Aggressive care at the EoL continues to be a trend despite evidence that it does little to improve quality of life and does not result in better outcomes.[1112] It has been shown to have a negative effect on the patient's quality of life and affects family members who are consequently subjected to higher psychological distress.[13]
The objectives of this study were: (1) to determine the incidence, nature and illness trajectory of deaths occurring in the ED of a large tertiary hospital in Saudi Arabia; (2) to examine to which extent EoL discussions had taken place prior and during the final ED visit; (3) to analyze how aggressive the care was at the EoL; and (4) to determine the involvement of palliative care services.
Three typical chronic illness trajectories have been identified: (1) advanced cancer, (2) organ failure, and (3) chronic frailty.[1] Patients with advanced cancer tend to have a more predictable decline, characterized by an initial good functioning state followed by rapid deterioration, most often over the span of a few months. In contrast, those with organ failure, such as heart failure or lung diseases, tend to have a trajectory marked by periods of acute exacerbations, with an overall slow decline in function between these episodes, with death often coming suddenly.[14] In the chronic frailty group, conditions such as degenerative neurological diseases and dementias often present with a poor functional baseline, and their decline is usually slow, in some cases extending over several years. A fourth trajectory is a sudden death. It can occur either in a person with no known prior health condition, or one with a stable or early chronic disease.[1] Understanding these four distinct trajectories can assist with prognostication and therefore offer guidance as to when initiate EoL care discussions that consequently enable adjustment of care. Best care models suggest that high-quality palliative care should be provided across the disease trajectory at each entry into the healthcare system.[7] An ED visit can provide an opportunity to refine and modify the patient's plan of care.[14]
In Saudi Arabia, palliative care implementation is still facing challenges in its full integration into the healthcare system. Some identified barriers are (1) gaps in the implementation of national policies, (2) lack of accessibility to primary health-care services and home care outside large cities, (3) gaps in healthcare providers' education, (4) limited specialized palliative care teams, and (5) public and healthcare providers' lack of awareness about palliative care. There is a paucity of studies about palliative care in Saudi Arabia, and none, to the best of our knowledge, have examined the EoL trajectory and quality of care of patients who die in the ED.
METHODS
This study is a retrospective chart review conducted at a 960-bed large tertiary hospital and cancer centre providing care to the adult and pediatric population in Saudi Arabia. This center is a large 960-bed hospital and regional cancer center that provides tertiary care to an adult and pediatric population. This hospital has an 8-bed tertiary palliative care unit, a consultation service, specialized outpatient clinics, and involvement in home care. The hospital's ED receives an estimated 55,000 visits per year. The study investigated the EoL trajectories of all patients who died in the ED over a 1-year period, from June 1, 2017, to June 1, 2018. Patients who came in cardiac arrest and for which no resuscitation interventions were initiated were considered “dead on arrival” and excluded from all analyses. This study was approved by the Research Ethics committee of the hospital and was conducted according to the ethical principles of the 2013 Declaration of Helsinki. The investigators requested a waiver of written consent for patients' participation as the study only involved the collection of data of deceased patients. All data were extracted from patients' medical file. The first part included demographics, clinical presentation features, and circumstances of death [Table 1]. The second part included data about previous and current EoL care discussions, Do-Not-Attempt-Resuscitation (DNAR) status, presence of aggressive interventions at the EoL, and palliative care services involvement. After data extraction, all patients were classified into one of the four “classical trajectory of dying,” by two independent investigators. The same methodology as used by Yash Pal et al.[1] in their study, “Death among elderly patients in the ED: A needs assessment for end-of-life care” has been reproduced to assign each patient in one of the EoL trajectories.[1] As seen in the original study, when two possible trajectories were present, a hierarchical order was used: Advanced cancer supplanted chronic frailty, which supplanted organ failure. When no prior co-morbidities were identified, patients were classified in the sudden death trajectory. The investigators who classified patients in the EoL trajectories are recognized as experts in their specialty and have over 10 years of experience in the field of palliative care.
| Variables | No. (%) |
|---|---|
| Sex | |
| Female | 43 (41.7%) |
| Male | 60 (58.3%) |
| Age* | 57 (SD 22) (63) |
| Main diagnosis | |
| Cancer | 47 (45.6%) |
| Cardiac and coagulation diseases | 13 (12.6%) |
| Miscellaneous | 13 (12.6%) |
| Multiple comorbidities | 10 (9.7%) |
| Renal diseases | 8 (7.8%) |
| Neurological disorders | 7 (6.8%) |
| Lung diseases | 5 (4.9%) |
| Reason for ED visit | |
| Circulatory and coagulation | 26 (25.2%) |
| Neurological | 22 (21.4%) |
| Respiratory | 19 (18.8%) |
| Miscellaneous | 15 (14.6%) |
| Pain | 10 (14.6%) |
| General deterioration | 8 (7.8%) |
| GI symptoms | 3 (2.9%) |
| Services | |
| Emergency | 38 (36.9%) |
| Medicine | 26 (25.2%) |
| Oncology | 25 (24.3%) |
| Surgery | 14 (13.6%) |
| Days between DNAR and death (n=64) | |
| 1 day | 15 (23.4%) |
| 2-7 days | 17 (26.6%) |
| 8-64 days | 16 (25%) |
| 64-1562 days | 16 (25%) |
*For the age, the mean, SD, median are reported
Statistical considerations
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 21.0 IBM SPSS Statistics for Windows, version 21 (IBM Corp., Armonk, N.Y., USA) for Windows. Descriptive statistics and graphic analyses were used. Categorical variables are reported as frequency and percentage values. Continuous variables are reported with their mean, standard deviation (SD), and median. The degree of agreement between the two investigators in regard to the categorization of patients' EoL trajectory was tested using Cohen's Kappa coefficient. A one-way analysis of variance (ANOVA) was performed to analyze variables categorized in three or more groups, such as the EoL trajectories groups and the Medical Service groups. It was followed by post hoc pair-wise comparison when the ANOVA revealed significant differences. An independent t-test was used to compare the utilization of aggressive treatment with “full code” and DNAR patients.
RESULTS
Demographics
Over a period of 1 year, 123 patients died in the ED. After excluding 20 patients considered “dead on arrival,” 103 deceased patients were included in the final analyses (n = 103). Males accounted for 58.3%, and the mean age was 57 years (SD = 22). Eight patients were under 18 years old. Cancer was the main diagnosis (45.7%) and the most common reasons for the ED visit were cardiac events (25.2%) and neurological complications (21.4%) [Table 1]. All patients were initially seen by emergency physicians and 63.1% were then transferred to the care of three primary service groups: Oncology (Medical-Oncology, Hematology-Oncology, Pediatric-Oncology), Medicine (Cardiology, Endocrinology, Nephrology, Pulmonary), and Surgery (Liver Transplant, General Surgery, Neurosurgery). The median duration of stay in the ED (between admission and death) was 20 h (mean = 72.5 h; SD = 169.74). 35.9% (n = 37) had a documented DNAR prior admission, and the median duration between the DNAR status being documented, and the time of death was 7.5 days (mean = 87.97; SD = 226.97). In the last year of life, the mean number of visits to the ED was 1.91 (SD = 2.035) and hospitalizations, 1.04 (SD = 1.228).
End-of-life trajectories
The analysis of end-of-life trajectories showed that the majority of deaths were related to advanced cancer (45.6%), followed by organ failure (29.1%), sudden death (13.6%), and chronic frailty (11.7%) [Figure 1]. The congruence between the two investigators regarding the classification of patients into the EoL trajectories was high with Cohen's Kappa coefficient of 0.85.
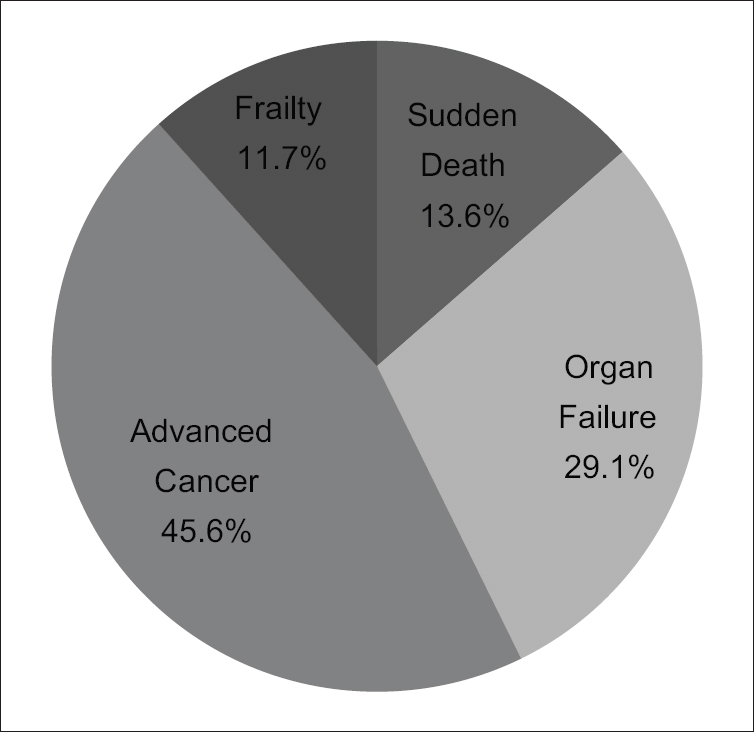
- Distribution of EoL trajectories for all deaths in the ED (N=103)
Aggressive treatments
About 51.5% (n = 53) of all patients received forms of aggressive treatment during their stay in the ED: Cardiopulmonary resuscitation (73.6%), intubation (56.5%), inotropes (75.5%), and ICU consultation (28.3%). According to an ANOVA post hoc test, results showed that the patients in the sudden death and organ failure groups received significantly more aggressive treatments that those from the advanced cancer and chronic frailty ones. No differences were found between the sudden death and the organ failure groups (P = 0.967) regarding the aggressiveness of intervention. After excluding the sudden death group (for which we expected more aggressive treatments), results showed that the emergency medicine service (EMS) was significantly more aggressive than the oncology, surgery, and medicine medical services. Furthermore, when excluding both patients with a DNAR order prior admission and the sudden death group simultaneously, the oncology and surgery services tended to be less aggressive than the medicine and EMS services [Figure 2]. According to independent sample tests (P < 0.001), patients with a previous DNAR order received significantly less aggressive treatments than full code patients. Overall, DNAR tended to be discussed late in the disease trajectory, but results also showed a significant variability between the different EoL trajectory groups (F (3, 63) = 5.29, [P = 0.003]). DNAR tended to be discussed earlier in the chronic frailty group (median = 126.0) (mean = 325.50 days; SD = 488.74; P = 0.001) than in the advanced cancer group (median = 5.0) (mean = 42.07; SD = 76.96) and the organ failure one (median = 7.0) (mean = 58.64; SD = 135.67).
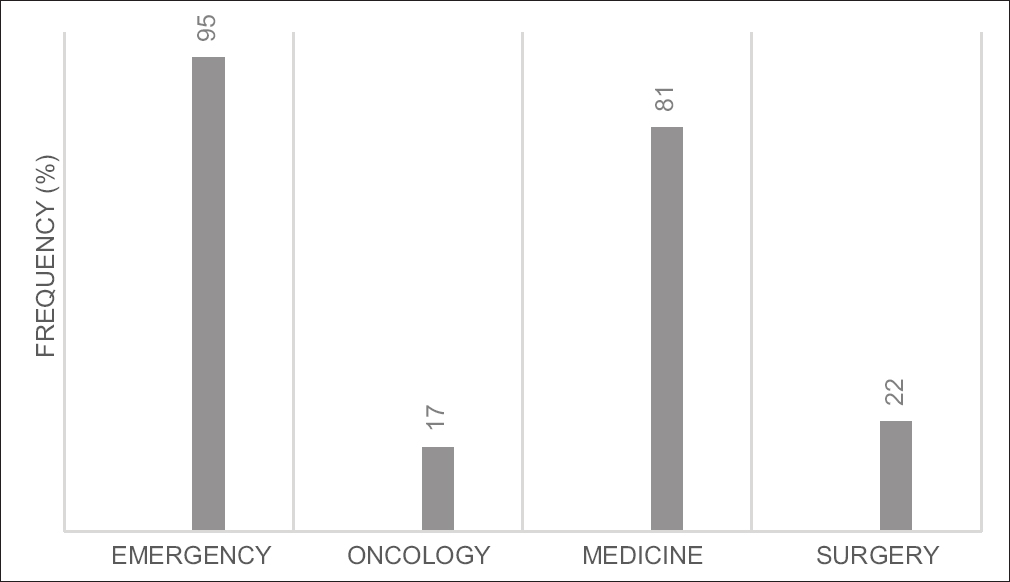
- Proportion of aggressive measures at the EoL in the ED per medical service
End-of-life discussions
After excluding the sudden death group, the extent to which EoL care discussions had been conducted prior and during this ED final visit were analyzed. Goals of care focusing on strict comfort care, withholding/withdrawing treatments, DNAR, prognosis, and preference for place of death are general components of high-quality EoL care discussions. ED physicians' explored at least one of these components in 40.4% (n = 36) of the cases. DNAR was the single most frequently discussed component (31.5%, n = 28), and place of death was the least discussed (6.7%, n = 6). Physicians from the primary services, whether from Oncology, Surgery or Medicine, discussed at least one component in 85.2% (n = 52) of the cases. DNAR (n = 44, 72.1%) was the most frequent and place of death (18.0%, n = 11) the least frequently discussed. Both oncology and surgery services discussed DNAR and goals of care focusing on comfort care significantly more frequently than Medicine services (P = 0.01). The palliative care service explored at least one component of an EoL care discussion in 80% (n = 16) of the cases it was consulted for. Prognosis was the most frequent component (65%, n = 13) followed by focus on comfort care (35%, n = 7), DNAR (20%, n = 4), and withholding treatment (10%, n = 2). The place of death was not discussed in any of the cases [Figure 3].
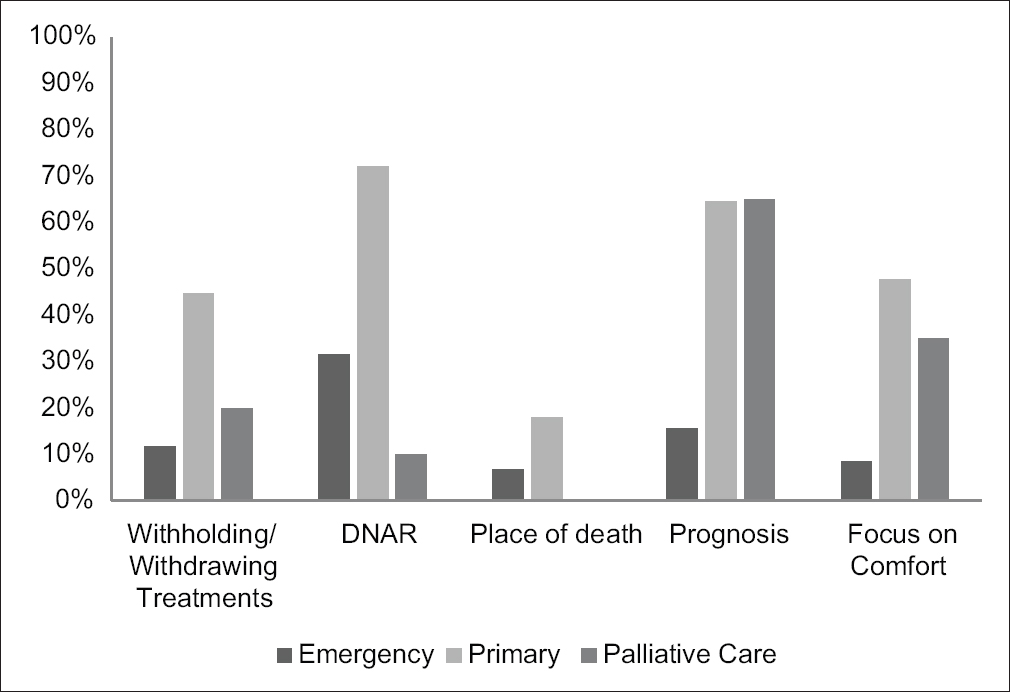
- Frequency of EoL discussions per medical services
Palliative care involvement
In the year preceding the patient's death, palliative care service was involved in the care of 22 out of these 103 patients. One striking finding is that 10/22 patients were referred to only a day prior to their death. The remaining were mostly referred by oncology, and the length of time between referral and time of death ranged from 15 to 76 days. During the admission to the ED when patient death occurred, Palliative care was consulted for 19.4% (n = 20) of cases. Oncology referred the most with 14 out of their 25 patients. Surgery consulted for 4/14 patients, medicine for 2/26, and emergency for none. Most of these consultations were for patients in the advanced cancer trajectory (19/20 patients referred) [Figure 4].
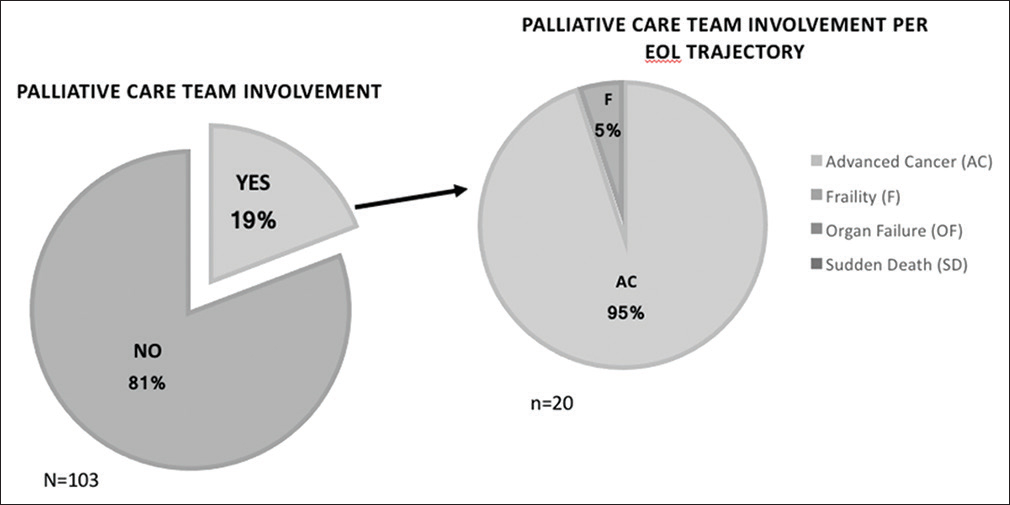
- Frequency of palliative care team involvement on the total number of deaths and per EOL trajectories
DISCUSSION
To the best of our knowledge, this is the first study looking into the EoL trajectories of patients dying in an ED in Saudi Arabia. Our study demonstrates that EoL care discussions are occurring late in the disease trajectory, a considerable number of patients are subjected to aggressive forms of treatment at the EoL and palliative care services remain underutilized. Most patients were categorized in the advanced cancer trajectory, which was not surprising as this study was conducted in a large tertiary cancer center. Nevertheless, considering that the advanced cancer trajectory has the most predictable course over the others, the results also indicate gaps in care planning in the last months of life of individuals affected by cancer. In 1988, in Saudi Arabia, a fatwa, which is a legal decision, was released and served as ground for the DNAR policies currently implemented in the Kingdom.[15] For a DNAR to be valid, three medical consultants must agree that the patient's medical condition is terminal and patients as well as families' input is not legally required.[15] Some 30 years later, important inconsistencies regarding the understanding, process and implementation of DNAR policies in Saudi Arabia remain.[16] There is also a lack of understanding of the ethical rules that must guide the care of patients with DNAR.[15] Some patients, families, and health-care providers associate DNAR with “no care” and are reluctant to have these discussions. The lack of systematic high-quality EoL care discussions can lead patients to be subjected to aggressive treatments. In a retrospective study conducted in Qatar, Hassan et al.[13] suggested that aggressive care was most likely attributable to factors such as a lack of chronic care facilities, a lack of appropriate prognostication models, delayed referrals to palliative care, and the unease of many oncologists to refer to palliative care. A study conducted by Al-Zahrani et al. (2013)[17] in a hospital in Saudi Arabia showed that 43% of all patients who died of cancer over a 1-year period had received disease-modifying treatments in the last year of life, among which 66% in the last 2 months and 14% in the last 2 weeks of their life. EoL care discussions need to occur in a calm setting, with proper time allocated for patients/family to ask questions about the condition, prognosis, and treatment options.[18] Time is needed to express concerns, preferences, and deal with the emotions associated with the declining condition. Optimally, these discussions should occur weeks, even months, before the patient enters the terminal stage. An EoL discussion is not a one-time discussion but should be an ongoing collaborative process. These discussions are about exploring what the patient/family knows about the overall condition and prognosis and with that understanding in mind, finding out what is important for them at this moment. For example, some patients, knowing that their time might be limited, may wish to engage in legacy planning or spend maximum time with their loved ones instead of being in and out of the hospital. Others may want to pursue curative treatments. It is also a choice to be respected and accommodated when feasible. When a patient is brought to an ED at the EoL, often because of acute symptoms requiring prompt attention, this patient/family is most often not in a mental state to process complex information and consider care options. A considerable proportion of aggressive treatments in the ED occur due to a lack of proper EoL discussions prior to this visit. Results have shown that outside DNAR, other components of high-quality EoL discussions were less explored. For example, preference for place of death was rarely brought up, and opportunities to have patients die in a more suitable environment than the ED are probably being missed. In a retrospective study analyzing all cancer deaths in Qatar over an extended period (2006–2012) (n = 1224), only 0.4% of patients died at home.[12] A study examining the place of death of cancer patients in Kuwait in 2009 indicated that 98.7% had died in the hospital (Alshemmari et al., in 2015).[19] The reasons why a very limited amount of patients choose to die home in Gulf countries need to be investigated further. Some patients/families might feel “safer” in the hospital, but this also bears the question, “Why?” If patients/families are not aware of the declining condition, poor prognosis, possible options at this stage, and do not have the proper support, they are not likely to choose to go home. Alsirafy et al. (2016)[20] conducted a retrospective cohort study in Saudi Arabia, investigating the reasons for ED visits by patients affected with terminal cancer (n = 154). Patients visited the ED in average 2.3 times in the last 3 months, and it was found that a significant number of these visits would have been most likely avoidable if there had been an earlier integration of palliative care services and better communication between medical services in general (Alshemmari et al., in 2013).[19] It seems that palliative care is still very much associated with dying and terminal care as half of the consultations in our current study occurred in the very last day of the patient's life.
Every visit to the ED should be considered as an opportunity to review the goals of care, including the DNAR status, of any patient with an identifiable EoL illness trajectory. During these admissions, primary treating teams should be contacted to do so, and palliative care services, as well as a home care, should also be considered. Even if this leads to a slightly longer stay, it will more likely lead to less readmissions/hospitalizations and more importantly, to better quality of care. To put this in place, ED physicians need to be well trained in recognizing the different EoL trajectories, on how to provide basic pain and symptom management, as well as how to conduct high-quality EoL care discussions in the particular ED setting. For patients for which EoL in the ED cannot be prevented, individual rooms for family to gather in the last moments should be available. Although our recommendations go beyond strictly aiming at providing better EoL care in the ED, the ultimate goal should be to prevent multiple emergency visits by having in place proper follow-up and support in the outpatient setting and community. An early multidisciplinary integrated approach where all health-care professionals work together toward the same goals is required. Goals of care need to be explored all along the course of the disease as the condition changes. Moreover, the responsibility of exploring goals of care should be a shared task between all members of the extended treating team and not solely rest on the primary treating team as well as on the medical service. It is everyone's responsibility to find out what is important for patients and families and to align the care in this direction. This is what true patient-centered care is.
Limitations
First, this study was conducted in a single center in Saudi Arabia. Most of the cases were cancer-related since the study was conducted in a tertiary oncology center. Results may not be applicable elsewhere. Second, the study design itself can lead to bias as the results are dependent on the available data contained in the medical files. Third, patients followed at this hospital are coming from all over the country. Significant data regarding the last months of life might be missing as some might have presented themselves to other EDs as well during this period. Finally, the exercise to classify each patient in an EoL trajectory is not without bias, especially when a decision as to be made between two competing illness trajectories.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Lori Nancarrow for reviewing the manuscript.
REFERENCES
- Death among elderly patients in the emergency department: A needs assessment for end-of-life care. Singapore Med J. 2017;58:129-33.
- [Google Scholar]
- A literature review on care at the end-of-life in the emergency department. Emerg Med Int. 2012;2012:486516.
- [Google Scholar]
- The integration of palliative care into the emergency department. Turk J Emerg Med. 2015;15:100-7.
- [Google Scholar]
- Integrated model of palliative care in the emergency department. Western J Emerg Med. 2013;14:633-6.
- [Google Scholar]
- A model for emergency department end-of-life communications after acute devastating events- Part II: Moving from resuscitative to end-of-life or palliative care treatment. Acad Emerg Med. 2012;19:1300-8.
- [Google Scholar]
- Am I doing the right thing? Provider perspective on improving palliative care in the emergency department. Ann Emerg Med. 2009;54:86-93.
- [Google Scholar]
- Research priorities for palliative and end-of-life care in the emergency setting. Acad Emerg Med. 2011;18:e70-6.
- [Google Scholar]
- Why do cancer patients die in the emergency department.: An analysis of 283 deaths in NC EDs? Am J Hosp Palliat Care. 2013;30:178-82.
- [Google Scholar]
- Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49:497-504.
- [Google Scholar]
- Family perspectives on aggressive cancer care near the end of life. J Am Med Assoc. 2016;315:284-92.
- [Google Scholar]
- Patterns in place of cancer death in the State of Qatar: A population-based study. PLoS One. 2014;9:e109615.
- [Google Scholar]
- Trends in the aggressiveness of end-of-life cancer care in the state of Qatar. J Glob Oncol. 2016;2:68-75.
- [Google Scholar]
- Treating cancer patients who are near the end of life in the emergency department. Emerg Med Clin North Am. 2009;27:341-54.
- [Google Scholar]
- Perspectives of interns and residents toward do-not-resuscitate policies in Saudi Arabia. Adv Med Educ Pract. 2016;7:165-70.
- [Google Scholar]
- Shifting paradigm: From “No code” and “Do-not-resuscitate” to “Goals of care” policies. Ann Thora Med. 2018;13:67-71.
- [Google Scholar]
- Pattern of cancer deaths in a Saudi tertiary care hospital. Am J Hosp Palliat Care. 2013;30:21-4.
- [Google Scholar]
- Advance Care Planning in End-Of-Life Care. New York: Oxford University Press; 2018.
- The place of death of patients with cancer in Kuwait. BMJ Support Palliat Care. 2015;5:510-2.
- [Google Scholar]
- Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidability. Am J Hosp Palliat Care. 2016;33:658-62.
- [Google Scholar]






