Translate this page into:
Quality of Sleep in Patients with Cancer: A Cross-sectional Observational Study
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Insomnia and poor sleep quality are common problems in patients with cancer. It interferes with the coping ability, symptoms, and treatment outcomes. The Pittsburgh Sleep Quality Index (PSQI) is a reliable, valid instrument to assess the quality of sleep in patients with cancer.
Patients and Methods:
The study was conducted at the department of medical oncology of a tertiary cancer care center. Consecutive eligible participants were recruited and evaluated for sleep quality using PSQI questionnaire. The questionnaire was administered only once with the questions evaluating to the quality of sleep over the last 1 month. A PSQI total score of ≤5 was suggestive of good quality of sleep and a score of >5 was indicative of poor quality of sleep.
Results:
Ninety-two consecutive consenting cancer patients admitted for chemotherapy participated in the study. Thirty-one (33.7%) patients had early cancer and 35 (38%) patients had Stage IV metastatic disease. Thirty-six (39.1%) patients reported sleep of <6 h and 30 (32.6%) patients had impaired functioning during day due to sleepiness. Fifty-three (57.6%) patients had poor total PSQI score, of which 39 (73.5%) were female and 14 (26.5%) were male. The study showed no correlation of the PSQI scores with the stage of the disease, and the prior treatment received.
Conclusions:
The study showed that Indian cancer patients have short sleep duration and poor quality of sleep. A higher prevalence of sleep disturbances was seen among female cancer patients. PSQI questionnaire can be a cost-effective way of screening cancer patients for poor quality of sleep.
Keywords
Cancer
Pittsburgh Sleep Quality Index
sleep
INTRODUCTION
The management of cancer is usually associated with high levels of emotional and psychological distress among patients and their relatives.[1] Sleep disturbance is one of the most common complaints in cancer patients.[1] Insomnia is defined as difficulty in initiating or maintaining sleep for a duration of at least 1 month and hence resulting in clinically significant distress and/or social and occupational impairment.[1] Insomnia and sleep disturbances can present before and after the diagnosis of cancer and may persist during and/or after the completion of treatment.[2] Many times, insomnia in cancer patients is aggravated by the treatments and their side effects and hence should be identified at the earliest and managed proactively.[3] Insomnia is multifaceted and affects several dimensions of quality of life of a patient. Patients with insomnia are prone to emotional disturbances, chronic fatigue, poor professional performance, and dependence on sedatives.[4] There is evidence to suggest a strong correlation of poor quality of sleep with profound negative outcomes, including decreased physical and psychological functioning, and a worse quality of life.[567] Furthermore, sleep disturbances can result in unplanned interruptions, poorer compliance and tolerance for treatment, or many a time a change in the treatment plan and may even be linked to more adverse events and a worse prognosis.[8] Based on the Pittsburgh Sleep Quality Index (PSQI) measures, it has been found that insomnia in cancer patients at the initiation of treatment is higher than that in the general population and ranged between 26% and 57%.[5910] This study of insomnia focuses on an important, underrecognized aspect among cancer patients.
PATIENTS AND METHODS
Study design and patients
A cross-sectional observational study was conducted at the department of medical oncology of a tertiary cancer care center between January 2017 and June 2017. The consecutive eligible participants were recruited after obtaining written informed consent. The inclusion criteria were adult patients diagnosed to have cancer and admitted for first course of chemotherapy. The exclusion criteria consisted of patients with previously diagnosed psychiatric illness or patients admitted for diagnosis of malignancy and patients with concurrent use of medications known to affect sleep. PSQI questionnaire was administered and compiled by a nurse. The questionnaire consisted of seven domains (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction) with a possible score of 0–3 each, making the possible total range of score from 0 to 21. A PSQI total score of ≤5 was suggestive of good quality of sleep and a score of >5 was indicative of poor quality of sleep. The study questionnaire evaluated the quality of sleep over the last 1 month. The data were collected on predesigned Microsoft Excel spread sheets, and the entries were double checked for any data entry errors. Continuous data were presented as mean and standard deviation (SD); categorical variables were presented as counts with percentages. The relationship between parameters was assessed with the Spearman's correlation test. All the statistical analyses were performed with SPSS version 20.0 (IBM Corp., Armonk, NY, USA). P < 0.01 was considered statistically significant.
RESULTS
Patient characteristics
Ninety-two consecutive consenting cancer patients admitted for chemotherapy in the medical oncology ward were administered the study questionnaire.
Sociodemographics
Sixty-seven (72.8%) patients were female and 25 (27.2%) were male. Thirty-one (33.7%) patients had early stage of cancer (Stage I and II) and 61 (66.3%) patients were diagnosed as advanced cancer (Stage III and IV), of which 35 (38%) patients had stage IV metastatic disease. The overall median age was 53 years with a range from 17 to 79 years. The median age was 53 years in females and 57 years in males. Ninety patients were married. Fifty patients were manual laborers and 35 patients were homemakers. Fifty-eight patients had undergone surgery and twenty patients had also received radiation before chemotherapy [Table 1].
| Variable | n (%) |
|---|---|
| Sex | |
| Male | 25 (27.2) |
| Female | 67 (72.8) |
| Education | |
| Illiterate | 39 (42.4) |
| Primary | 30 (32.7) |
| Secondary | 10 (10.9) |
| Graduate | 2 (2.1) |
| Postgraduate | 11 (11.9) |
| Marital status | |
| Married | 90 (97.8) |
| Single/divorced | 2 (2.2) |
| Occupation | |
| Homemaker | 35 (38) |
| Cooly | 50 (54.4) |
| Student | 2 (2.1) |
| Others | 5 (5.5) |
| Site | |
| Breast | 31 (33.7) |
| Upper GIT | 18 (19.7) |
| Ovary | 14 (15.2) |
| Cervix/endometrium | 7 (7.6) |
| Colorectal | 10 (10.9) |
| Lung | 8 (8.6) |
| Others | 4 (4.3) |
| Stage | |
| I | 9 (9.6) |
| II | 18 (19.7) |
| III | 30 (32.7) |
| IV | 35 (38) |
| Disease extent | |
| Early | 31 (33.7) |
| Advanced | 61 (66.3) |
| Surgery | |
| Yes | 58 (63) |
| No | 34 (37) |
| Radiation therapy | |
| Yes | 20 (21.7) |
| No | 72 (78.3) |
GIT: Gastrointestinal tract
Sleep scores
The average global PSQI score was 6.57 (SD = 3.52). The range of scores was 1–17. The mean scores of PSQI were 6.89 (SD 3.64) in females and 5.72 (SD 3.04) in males. There were 53 (57.60%) patients who had poor total PSQI score (>5), of which 39 (73.5%) were female and 14 (26.5%) were male [Figure 1].
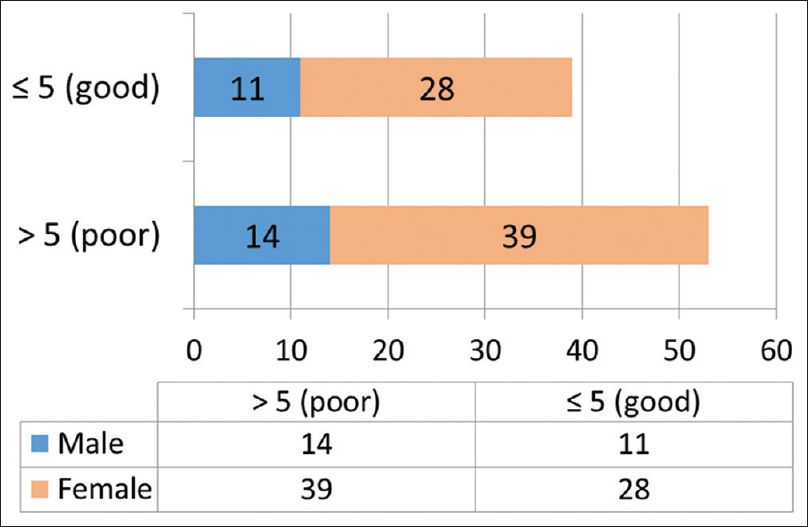
- Pittsburgh Sleep Quality Index scores in males and females.
Thirty-six (39.1%) patients complained of sleep of <6 h duration, of which 26 were female [Figure 2]. Thirty-six (39.1%) patients complained of significant sleep disturbance [Figure 3] and 30 (32.6%) patients had daytime dysfunction due to sleepiness [Figure 4]. Thirty-four (36.9%) patients had poor sleep efficiency [Figure 5].

- Number of hours of sleep in males and females.

- Sleep disturbance scores in males and females.

- Daytime dysfunction scores in males and females.

- Sleep efficiency scores in males and females.
The correlation between the sleep score with the stage of the disease and the prior treatment was analyzed using the Spearman's correlation test. There was no correlation of the PSQI scores with the stage and the prior treatment received [Table 2].
| Spearman’s rho | Stage | Radiation therapy | Surgery | PSQI score |
|---|---|---|---|---|
| Stage | ||||
| Correlation coefficient | 1.000 | 0.328** | −0.479** | −0.180* |
| Significant (two-tailed) | 0.000 | 0.000 | 0.031 | |
| n | 92 | 92 | 92 | 92 |
| Radiation therapy | ||||
| Correlation coefficient | 0.328** | 1.000 | −0.232** | −0.113 |
| Significant (two-tailed) | 0.000 | 0.006 | 0.182 | |
| n | 92 | 92 | 92 | 92 |
| Surgery | ||||
| Correlation coefficient | −0.479** | −0.232** | 1.000 | 0.076 |
| Significant (two-tailed) | 0.000 | 0.006 | 0.365 | |
| n | 92 | 92 | 92 | 92 |
| PSQI score | ||||
| Correlation coefficient | −0.180* | −0.113 | 0.076 | 1.000 |
| Significant (two-tailed) | 0.031 | 0.182 | 0.365 | |
| n | 92 | 92 | 92 | 92 |
PSQI: Pittsburgh Sleep Quality Index. *P<0.05, **P<0.01
DISCUSSION
Sleep disorders are often not or underdiagnosed in cancer patients, and a higher prevalence has been seen among female cancer patients.[1] Usually, the sleep disturbances in patients with cancer on chemotherapy are multifactorial. The significant psychological impact of the disease, the chemotherapy, and medications such as corticosteroids have all been reported as potential contributors.[11] A systematic review of sleep disorders in cancer patients found that it is difficult to assess the prevalence of particular types of sleep disorders in cancer due to the focus on studying symptoms of poor sleep and not characterizing the underlying sleep disorders.[12] Thus, it is crucial to identify the causative factors behind the sleep disturbances to treat insomnia. Psychological interventions such as cognitive behavioral therapy have demonstrated clinical benefit to insomnia patients in randomized clinical trials.[13] However, access to these psychological therapies is usually limited or not available in most of the centers treating cancer patients. Yoga has also shown to improve symptoms,[14] and acupuncture has also shown to effectively reduce cancer-related depression, improve sleep quality, and thus improve the quality of life of cancer patients.
Our study showed that clinically significant sleep disturbance occurred in high numbers of cancer patients on chemotherapy, reflecting a significant symptomatic burden that is poorly documented and managed in routine clinical practice. The median age of patients in our cohort was 53 years, consistent with the data from India.[10] Our results are consistent with the previous studies where higher levels of sleep disturbance have been observed in women undergoing chemotherapy.[71516171819]
A longitudinal study conducted in North America found a higher prevalence of sleep disturbance among female patients undergoing adjuvant chemotherapy for breast cancer, in which 48.5%–65.8% of patients had PSQI scores ≥5.[20] Similarly, in a cross-sectional study of breast cancer survivors in Bahrain, significant sleep disturbances in 17.6% of women were documented, ranking second after fatigue as the most distressing symptom.[6] This prospective study using validated tools found that the sleep quality was poor in female cancer patients and the incidence of clinical insomnia was high in cancer patients. The limitations of this study include small sample size and lack of additional measures such as the health-related quality of life not being included in the study.
CONCLUSIONS
The study has shown that patients with cancer experience an increase in insomnia and sleep disturbances during the treatment which is largely overlooked in routine clinical practice. There is an unmet need to routinely screen patients for sleep disorders to minimize the disease burden and to improve the quality of life. More studies are required to develop strategies in routine practice to diagnose, prevent, and treat insomnia among cancer patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [Google Scholar]
- A prospective study of quality of life in breast cancer patients undergoing radiation therapy. Adv Radiat Oncol. 2016;1:10-6.
- [Google Scholar]
- Cancer treatments and their side effects are associated with aggravation of insomnia: Results of a longitudinal study. Cancer. 2015;121:1703-11.
- [Google Scholar]
- Insomnia in the context of cancer: A review of a neglected problem. J Clin Oncol. 2001;19:895-908.
- [Google Scholar]
- Relationship between mood disturbance and sleep quality in oncology outpatients at the initiation of radiation therapy. Eur J Oncol Nurs. 2010;14:373-9.
- [Google Scholar]
- Predictors of initial levels and trajectories of depressive symptoms in women with breast cancer undergoing radiation therapy. Cancer Nurs. 2013;36:E34-43.
- [Google Scholar]
- Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol. 2011;78:127-37.
- [Google Scholar]
- Subjective sleep and overall survival in chemotherapy-naïve patients with metastatic colorectal cancer. Sleep Med. 2015;16:391-8.
- [Google Scholar]
- Sleep-wake circadian activity rhythm parameters and fatigue in oncology patients before the initiation of radiation therapy. Cancer Nurs. 2011;34:255-68.
- [Google Scholar]
- The prevalence of insomnia in the general population in china: A meta-analysis. PLoS One. 2017;12:e0170772.
- [Google Scholar]
- Insomnia in cancer-associations and implications. Asian Pac J Cancer Prev. 2015;16:6711-4.
- [Google Scholar]
- Systematic review of sleep disorders in cancer patients: Can the prevalence of sleep disorders be ascertained? Cancer Med. 2015;4:183-200.
- [Google Scholar]
- Sleep disturbance in adults with cancer: A systematic review of evidence for best practices in assessment and management for clinical practice. Ann Oncol. 2014;25:791-800.
- [Google Scholar]
- Yoga for the treatment of insomnia among cancer patients: Evidence, mechanisms of action, and clinical recommendations. Oncol Hematol Rev. 2014;10:164-8.
- [Google Scholar]
- Impact of breast cancer treatments on sleep disturbances a systematic review. Breast. 2014;23:697-709.
- [Google Scholar]
- Trajectories of sleep disturbance and daytime sleepiness in women before and after surgery for breast cancer. J Pain Symptom Manage. 2013;45:244-60.
- [Google Scholar]
- Inflammation and behavioral symptoms after breast cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517-22.
- [Google Scholar]
- Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med. 2008;4:441-9.
- [Google Scholar]
- The relative importance of specific risk factors for insomnia in women treated for early-stage breast cancer. Psychooncology. 2008;17:9-18.
- [Google Scholar]
- Longitudinal prospective assessment of sleep quality: Before, during, and after adjuvant chemotherapy for breast cancer. Support Care Cancer. 2013;21:959-67.
- [Google Scholar]






