Translate this page into:
Unfolding Role of Erector Spinae Plane Block for the Management of Chronic Cancer Pain in the Palliative Care Unit
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pain adversely affects the quality of life in cancer patients. Although conventional oral analgesics and co-analgesics manage 80%–90% of pain, interventional pain management techniques may be useful in the management of cancer pain refractory to opioid analgesia or in patients unable to tolerate systemic opioids. Herein, we report three cases depicting the successful role of erector spinae plane block in our palliative care unit for the management of different chronic cancer pain.
Keywords
Cancer pain
palliative care
ultrasound
INTRODUCTION
Pain is one of the most frequent and frightening symptoms in cancer and has been shown to affect the quality of life adversely. The prevalence of pain varies from 39.3% after curative treatment to 66.4% in advanced, metastatic, or terminal disease.[12] Pain can be well managed in 80%–90% of these patients with conventional analgesics and co-analgesics, which can usually be taken orally. Prescription should be according to the principles of the WHO analgesic ladder, although approximately 10% of patients have pain that remains difficult to manage and who may benefit from some form of interventional technique.[34] Neuraxial techniques have some contraindications or limitations (coagulation disruptions, deformities of the thoracic spine, and patient refusal), which mandate searching for an analgesic alternative.[5] Erector spinae plane (ESP) block is one of the newer interfascial techniques with great safety and potential applications. This technique is first described by Forero et al., in which drug is injected below the erector spinae muscle for the management of thoracic neuropathic pain.[6] ESP block has been mainly used as a postoperative analgesia method in many surgical procedures.[7] ESP block in chronic cancer pain has not been studied extensively. ESP block at the lumbar level is also not extensively studied in chronic cancer pain. There are few case reports mentioning the use of lumbar ESP block in hip arthroplasty and failed back syndrome.[89] Herein, we report three cases depicting the successful role of ESP block in our palliative care unit for the management of chronic cancer pain. Informed written consent was obtained from the patients for reporting the same.
CASE REPORTS
Case 1
A 19-year-old female (50 kg; 160 cm) was admitted in the palliative care unit of our department with complaints of severe burning and stretching pain in the right flank region. Her pain scores were 10/10 on the Numeric Rating Scale (NRS), where 0 means no pain and 10 means worst possible pain. The patient was a postoperative case of desmoid tumor for which resection was done 2 years back [Figure 1]. Skin on the right side flank region develops pain, thickness, and tenderness from the past 6 months. The patient received medical treatment (morphine, nonsteroidal anti-inflammatory drugs [ibuprofen and paracetamol], and gabapentin), but the pain did not improve. Hence, we decided to perform lumbar ESP block.

- Patient with painful postoperative scar of desmoid tumor
Under all aseptic precautions, a linear ultrasound probe was placed longitudinally at the level of transverse process of L2. The skin was infiltrated with 2 ml of 1% lignocaine. The 10-cm Stimuplex needle (Stimuplex® A, B. Braun Melsungen AG, Germany) was inserted by the in-plane approach to touch the surface of transverse process of L2 [Figure 2]. A total of 20 ml of 0.375% ropivacaine and 40 mg triamcinolone was injected into the target plane between the erector spinae muscles and the transverse process. The patient had adequate pain relief (3/10 on NRS) 10 min after the block and had extensive sensory blockade from dermatome T10 to L5. NRS was noted for 24 h after the procedure [Table 1]. The patient was discharged with oral medicines tapered. The patient was still pain-free without consumption of any oral analgesics at follow-up after 8 weeks.
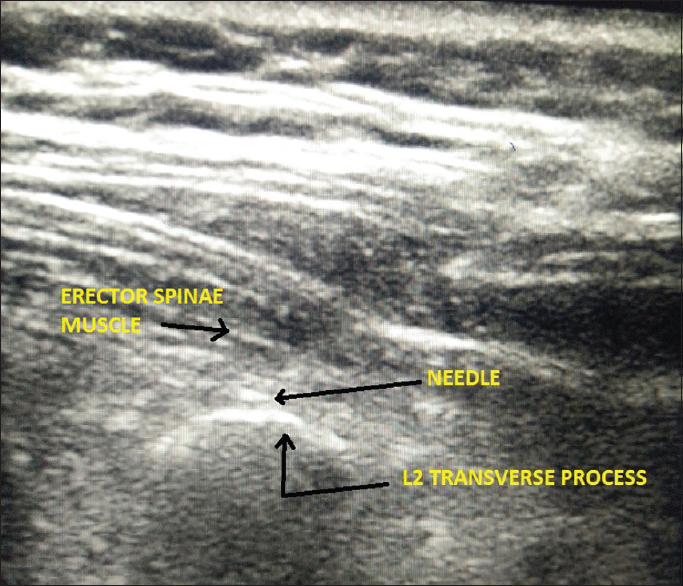
- Ultrasound image showing needle placement at L2 transverse process below the erector spinae muscle
| NRS | Before ESP block | 10 min after block | 15 min | 20 min | 30 min | 1 h | 6 h | 12 h | 24 h |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 10 | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 3 |
| Case 2 | 7 | 1 | 1 | 2 | 2 | 3 | 3 | 2 | 2 |
| Case 3 | 9 | 0 | 1 | 1 | 1 | 1 | 2 | 1 | 1 |
NRS: Numeric Rating Scale, ESP: Erector Spinae Plane
Case 2
A 42-year-old male (45 kg; 155 cm) with right Pancoast tumor severe pain (7/10 on NRS) from 5 months in dermatome distribution from C5 to T3, incompletely relieved on medical treatment. Right ESP block was given at T2 level in the sitting position. Following administration of 20 ml of 0.375% ropivacaine and 40 mg triamcinolone, pain was relieved in few minutes (1/10 on NRS) with sensory blockade from C3 to T5 on the right side. NRS score was noted for 24 h [Table 1]. The patient was discharged with oral medications tapered. The patient was still pain-free without consumption of any other oral analgesics at the follow-up after 2 months.
Case 3
A 64-year-old male (46 kg, 152 cm) presented with postthoracotomy pain syndrome 1 year after undergoing right bilobectomy. He had severe pain (9/10 on NRS) over the anterior and posterior right chest area and described it as burning, tingling, and current-like sensation around the thoracotomy scar at the T8-T9 level. Despite the high dosage of oral analgesics, he experienced significant pain. A right ESP block with 20 mL of 0.375% ropivacaine and 40 mg of triamcinolone was performed at the T8 level. Following the injection, pain was relieved in few minutes (0 on 10 on NRS) with sensory blockade from T5 to T12 on the right side. NRS score was noted for 24 h [Table 1]. The patient was discharged with oral medications tapered. The patient remained pain-free for 1.5 months without consumption of any other oral analgesic. A second ESP block was performed with 20 mL of 0.25% ropivacaine and 40 mg triamcinolone which again produced significant analgesia lasting 2 weeks.
DISCUSSION
The ESP block was previously described by Forero et al. in video-assisted thoracoscopic surgery[6] and laparoscopic ventral hernia repair.[10] Veiga et al. described the use of this technique in radical mastectomy and reported opioid-sparing effect and adequate analgesia.[11] Bonvicini et al. have also reported effective postoperative analgesia with bilateral ESP blocks in breast cancer surgery.[12]
Takahashi and Suzuki successfully described the role of lumbar ESP block in a case of failed back surgery syndrome-associated low back pain.[9] Tulgar et al. reported a case of hemiarthroplasty which was successfully performed under a combination of ultrasound-guided lumbar ESP block and quadratus lumborum block.[8] ESP block has emerged as a regional technique with effective analgesia along with simplicity and safety.[4] There are minimal procedure-related complications in the ESP block as compared to neuraxial blocks as there are no structures at risk of injury in the vicinity.[13] Following the principles of cancer pain assessment, the management of total pain, use of WHO ladder of pain, and interventional pain management in severe, intractable pain is now the essence of palliative medicine.[14]
This report suggests that ESP block can also be used for different types of chronic cancer pain. Our findings are based on a case series; therefore, we further suggest controlled studies to know the efficacy of ESP block as compared to conventional analgesic techniques in terms of technical difficulty, patient comfort, and duration of pain relief in chronic pain patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Update on prevalence of pain in patients with cancer: Systematic review and meta-analysis. J Pain Symptom Manage. 2016;51:1070-90.
- [Google Scholar]
- Neuropathic pain in cancer patients: Mechanisms, syndromes, and clinical controversies. J Pain Symptom Manage. 1997;14:99-117.
- [Google Scholar]
- Cancer pain management: Part II: Interventional techniques. Contin Educ Anaesth Crit Care Pain. 2015;15:68-72.
- [Google Scholar]
- Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592-6.
- [Google Scholar]
- Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev. 2005;1:CD004088.
- [Google Scholar]
- The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621-7.
- [Google Scholar]
- Ultrasound-guided bilateral erector spinae plane block could provide effective postoperative analgesia in laparoscopic cholecystectomy in paediatric patients. Anaesth Crit Care Pain Med. 2019;38:87-8.
- [Google Scholar]
- Combination of lumbar erector spinae plane block and transmuscular quadratus lumborum block for surgical anaesthesia in hemiarthroplasty for femoral neck fracture. Indian J Anaesth. 2018;62:802-5.
- [Google Scholar]
- Erector spinae plane block for low back pain in failed back surgery syndrome: A case report. JA Clin Rep. 2018;4:60.
- [Google Scholar]
- The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452-60.
- [Google Scholar]
- Erector spinae plane block for radical mastectomy: A new indication? Rev Esp Anestesiol Reanim. 2018;65:112-5.
- [Google Scholar]
- Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2018;44:3-4.
- [Google Scholar]
- Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121.
- [Google Scholar]






