Translate this page into:
How Patients of Oral Cancer Cope Up with Impact of the Disease? A Qualitative Study in Central India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Oral cancer is an important cause of mortality and morbidity in India. The disease per se and side effects of different treatment modalities impart a negative physical and psychosocial impact on the patients. This study was designed to have a better understanding of patients concerns.
Materials and Methods:
This is a qualitative study using in-depth interviews on 24 purposively selected oral cancer patients who have completed their treatment. The study was conducted from January 2016 to September 2017 in both urban and rural community development block in a district in Central India. Participants were selected irrespective of age, sex, occupation, education, stage of disease, and treatments received. The recorded interviews were transcribed for analysis, done using ATLAS ti. The study was conducted after ethical approval.
Results:
Concerns regarding quality of life, social constraints, financial security, and eating problems were the four major themes, which evolved from the analysis. Emotional and physical distress, disfigurement, dependency, feeling blamed, and avoidance are the evolved subthemes that had a negative psychosocial impact. Spiritualism, acceptance of the disease and increased public attention and support are the factors that increase the confidence among the cancer patients.
Conclusion:
Quality of life of oral cancer patients should be given prime focus along with continuum of care starting from early means of diagnosis by screening to treatment completion. Nevertheless, it is the family support that seems to play the most vital role in helping cancer patients cope up with the problems.
Keywords
Impact on patients
oral cancer
qualitative analysis
quality of life
INTRODUCTION
In Indian scenario, oral cancer is one of the most commonly occurring cancers with an estimated 600,000–700,000 deaths in 2012.[1] The International Agency for Research on Cancer GLOBOCAN project[2] has predicted that India's cancer burden will nearly double in the next 20 years, from slightly over a million new cases in 2012 to more than 1.7 million in 2035. Oral cancer is treated by different modalities that depend on the stage of presentation. Due to different reasons, most of the patients of oral cancer present late with advanced disease. The treatment options include combination of surgery, radiotherapy and chemotherapy. Palliative therapy is often required in advanced disease. The side effects of the treatment increase the suffering of the oral cancer patients. Among the different physical complains of the patients, the most common are pain, dryness of mouth, sticky saliva, feeding problems, and problem in speaking.[3] Disfigurement resulting from the massive surgeries undertaken to control the disease results in a psychological stress to the patients apart from the physical agony.[45] The other problems are professional limitations, economic crisis. and disruption of family. The ramification of these problems of cancer survivors is not a new discovery, but most of the studies focus on the quantitative analysis using some standardized tools such as European Organisation for the Research and Treatment of Cancer.[6] But with these tools, it is not easy to understand the experience of the oral cancer patients as regards to their coping with different problems they face because of the disease and its treatment. As a result of which, this very study was designed to have a detailed understanding of the problems faced by the oral cancer patients from the time of diagnosis till the end of treatment procedures.
MATERIALS AND METHODS
We used in-depth interviews (IDI) in this qualitative study. During the IDIs, the participants were encouraged and prompted to talk in depth about the different problems they came across since the diagnosis of oral cancer and how they could cope up with the problem. We focused on understanding the experiences and the needs of the oral cancer patients as regards to the early diagnosis and treatment of the disease.
Study participants
The study participants included 24 patients of oral cancer who have completed their treatment 2–4 months before the interviews were taken and went to the cancer hospital for regular follow- up. The participants were purposively chosen study respondents who could provide rich, relevant, and diverse information pertinent to the research objectives. They were selected irrespective of age, sex, occupation, educational qualification, stage of disease, and treatments received. Cancer occurring in lip, tongue, buccal mucosa, gingiva buccal mucosa and alveolus were regarded as oral cancer in our study.
General characteristics of the study participants are shown in Table 1, where we found six of them were females and the rest were males. More than half of the patients were elderly (>60 years). Farming and daily labor were the most common occupations among the males while females were mostly homemakers. Majority of the patients were suffering from advanced oral cancer (Stage III and Stage IV). Combinations of treatments (Surgery, chemotherapy, and radiation) were used to treat the patients. Futhermore, in the advanced disease, the patients received palliative therapy.
| Participant ID | Age (years) | Sex | Site of oral cancer | Occupation | Education | Stage of disease (TNM) | Treatment received |
|---|---|---|---|---|---|---|---|
| P1 | 54 | Male | Buccal | Farmer | Class 6 | II | SX + RT |
| P2 | 62 | Male | Tongue | Farmer | Illiterate | III | SX + RT + CT |
| P3 | 38 | Male | Alveolus | Auto driver | Class 10 | IV | SX + RT + CT |
| P4 | 51 | Female | Buccal mucosa | House wife | Graduate | II | SX + RT |
| P5 | 60 | Male | Alveolus | Daily labour | Illiterate | III | SX + RT + PL |
| P6 | 54 | Female | Buccal mucosa | Daily labour | Class 8 | IV | RT + CT + PL |
| P7 | 35 | Male | Buccal mucosa | Farmer | Class 5 | IV | SX + RT + PL |
| P8 | 67 | Male | Lip | Retired employee | Class 12 | I | SX + RT |
| P9 | 74 | Male | Alveolus | Not working | Class 4 | III | SX + RT + CT |
| P10 | 82 | Male | Gingivo buccal mucosa | Not working | Illiterate | IV | RT + CT + PL |
| P11 | 77 | Male | Gingivo buccal mucosa | Retired employee | Class 10 | IV | SX + RT + CT + PL |
| P12 | 65 | Male | Buccal mucosa | Farmer | Class 6 | IV | SX + RT + CT + PL |
| P13 | 64 | Female | Buccal mucosa | Daily labor | Class 6 | III | SX + RT + CT |
| P14 | 60 | Female | Tongue | Business | Class 10 | II | SX + RT + CT |
| P15 | 58 | Male | Alveolus | Farmer | Class 8 | III | SX + RT + CT + PL |
| P16 | 44 | Male | Alveolus | Farmer | Class 5 | II | SX + RT |
| P17 | 35 | Male | Tongue | Daily labour | Illiterate | I | SX + RT |
| P18 | 70 | Male | Lip | Shop | Class 7 | II | SX + RT |
| P19 | 59 | Female | Buccal mucosa | Daily labour | Class 5 | III | SX + RT + CT |
| P20 | 43 | Male | Gingivo buccal mucosa | Auto driver | Class 12 | IV | SX + RT + CT + PL |
| P21 | 70 | Male | Gingivo buccal mucosa | Retired employee | Graduate | II | SX + RT |
| P22 | 36 | Male | Lip | Service | Graduate | II | SX + RT |
| P23 | 65 | Male | Gingivo buccal mucosa | Not working | Class 5 | IV | SX + RT + CT + PL |
| P24 | 64 | Female | Buccal mucosa | Daily labour | Illiterate | III | SX + RT + CT |
SX: Surgery, RT: Ratiaotherapy, CT: Chemotherapy, PL: Palliative therapy, TNM: Tumor node metastasis
Study procedure
An interview guide [Table 2] was compiled beforehand. Open questions were used to encourage the study participants to express their feelings and experiences as regards to the disease per se Before the study, a pilot interview was conducted with two patients to check if the patients could understand the study question and give feedback. The pilot interview was also included in the final analysis. The study was done from January 2016 to September 2017.
| How can you differentiate between your present life and your past, when you did not have Cancer? |
| Probes: |
| Personal life |
| Family life |
| Financial life |
| Social life |
| Psychosocial life |
| Please tell me about your social and psychological support |
| Probes: |
| Support from family and friends-adequate or not |
| Role of spiritual/religious leaders in your life |
| What are the different things you think about future? |
| Probes: |
| Your future |
| Future of family |
| Regarding insecurity |
| Concerns about financial life in future |
| Did you face any problems/challenges at the different facilities you visited for treatment of your oral cancer? Please share with me, those problems |
| Probes: |
| Timeliness of medical attendance |
| Behavior of hospital staff |
| Transportation |
| Hospital stay |
| Financial problem |
| Promptness of treatment |
| How did you cope up with the changes? |
| Probes: From where did you get the support? |
Study settings
The study participants were the residents of both urban and rural community development block in a district in Central India, which has two medical colleges with Cancer wings. First author who is well trained in qualitative methods conducted all the interviews. The interviews were conducted in the houses of the participants. All the interviews were conducted in Hindi, which the study participants understood. Each of the IDI continued for around 40–60 min. Interviews were taken till there was saturation of information, and no new information came up. Many of the interviews were audio recorded, and the others were noted down, as the study participants did not give permission for using recorder. While carrying out the interviews, concern was taken to ask the questions in private that is keeping the other family members secluded, though it was not possible all the time.
Data analysis
The audio recording of IDIs was transcribed and translated into English. Recurring ideas, words or phrases, and patterns of belief were identified and organized in codes; and based on these salient themes and subthemes were defined. Following this, the investigator went through each transcribed document of IDI and did content analysis using the themes and subthemes that link people and circumstances. Efforts were made to analyze how the distribution of ideas, words or phrases under different subthemes, and themes differ across the categories enumerated above. ATLAS ti[7] was used to facilitate the content analysis.
Ethics
The study was conducted after getting approval from the Institutional Ethics Committee. Written informed consent was taken from each of the study participants before starting the interview.
RESULTS
After analyzing the transcripts, we could point out four major themes as regards to the concerns of the oral cancer patients regarding the diseases, treatment, and its ill effects. Those were concerns for their quality of life, social constraints, financial security, and feeding problem. Each of the themes was explained by means of further subthemes.
Theme 1: Quality of life concerns
-
The concerns regarding the quality of life of the patients themselves were described under the following subthemes.
Emotional distress
“All the time I think about myself and the disease” said P1. In a similar depressive note P2 acclaimed, “From the day of diagnosis, the question remains, why me?” Depression and anxiety were commonly observed in almost all participants during interview. A few of them also got irritable while speaking of the disease. While talking, an old man who was receiving palliative treatment (P 11) got very emotional and said “my sons no more listen to me.” Many of the patients (P 2, 7,11, 15, 16) expressed their emotional strain associated with the frequent hospital treatment and follow-ups. “My treatment was completed 2 months back, but I still have to come to this hospital regularly, which is quite far away from my home.”
Physical symptom burden
This was the most important problem faced by almost all individuals who took part in our study. They frequently had pain in their mouth that incapacitated them. Many of them had to take morphine on regular basis for pain. Apart from pain in mouth and jaw, they had difficulty in swallowing and soreness in oral cavity. “I cannot open my mouth wide open after my cancer treatment and so I cannot eat solid food”, said a 65-year study participant (P 12). Another patient (P 18) said, “I have sticky saliva that drools from my mouth all the time”. Apart from the physical problems related to oral cavity and eating food, many of them also had problem in talking to other people. One of them (P19) also complained, “I cannot perceive smell since I have undergone surgery.”
Concerns for appearance
Surgery, including total mandibulectomy and partial maxillectomy, was commonly preformed in oral cancer spreading to bones. In these cases, disfigurement of face was a major concern to the patient, irrespective of their age and sex. Many of them kept their faces covered all the time, even at home. A post mandibulectomy patient (P 15) on palliative treatment said, “I keep my face covered, as I think it's quite horrible to see.”
Apart from disfigurement of the face, there were also cases of hair fall as a result of chemotherapy and scar mark in face and neck. Radiation darkened their skin area, and it was also a matter of concern for a female participant who had cancer of buccal mucosa.
Change in daily activities
“I am having two small school going kids and old mother, but as a result of this disease (cancer tongue), I am bed ridden for last 6 months and now though I go to field, but I feel very weak and cannot work like before,” said a 35 years old study participant (P 17), who previously used to work as a daily laborer. Like him, there were a few more oral cancer patients who were very concerned regarding their inability to perform like before. In addition to frequent medical appointments, some participants characterized their inability to work as a major change in their daily routine. Whereas some of the participants described the feelings of boredom associated with job loss, others noted a profound shift in their self-confidence.
One of them was also concerned regarding the increasing burden on his wife after he got the disease. The 58-year-old postchemotherapy and post radiotherapy patient of alveolar cancer (P 15) said, “As I am unable to work now, my wife has to go to field”. This patient was also very much concerned about her future.
Feeling blamed
Many of the patients of oral cancer described that they are blamed for the causation of the disease. They said that it is not only by their neighbors or relatives but also by their own family and sometimes also treating physician. One of the participants (P 10) said, his primary care physician had blamed him for his disease, “(my doctor said), did you know that you are solely responsible for your health conditions (oral cancer)? As you were used to chewing kharra (a form of oral tobacco taken with lime, which is prevalent in Central India), since you were a child, it priced you this disease.” Most of them have agreed that they were habituated to chewing oral tobacco since last 20 to 30 years or more and understood that tobacco was responsible for causing cancer, but the way people blamed them for that was “somewhat undeserving” (P 9). Another individual (P 21) said that, “when I started taking kharra, no one knew that it caused cancer. At that time, this was a common and acceptable practice in the community.”
Experiencing surprise about survival
It's a common understanding among almost all the participants that cancer does not have any treatment and therefore, many of them did not come to hospital in early stage of the disease. One of the participants was diagnosed 2 years back and had completed treatment few months back. He was surprised that he was still alive.
Some of them were also worried about their death. One of them (P 21) said, “I want to be there to see my two daughters get married and have children. I want to hold my grandchildren some day but I am afraid as I may not be able to do so.”
Acceptance of the disease
There were very few participants who were positive about the outcome of treatment, regularly visited hospital for their follow-up and listened to what their doctors advised them. One of them said, “What can I do, if I am having cancer? There are good treatment options available now and I have stopped taking ghutka (a form of oral tobacco) now and have completed my treatment 3 months ago.” Another young participant (P 23) added, “I have to earn for my family and I don’t have time to think about the consequences.”
A few of them also mentioned that they have become more spiritual after suffering from cancer. “It was God's wish that I should have the disease and it is He who will make me well”, said a middle-aged man suffering from lip cancer. They had some sense of relief after praying and worshipping. One of the female participants (P 24) added “all of us have a limited time span in this world, I got an advance notice, and therefore, I must utilize rest of my life worshipping God.”
Theme 2: Experiencing social constraints
There were quite a few study subjects who described social constraints on disclosure of cancer-related concerns. Specifically, participants stated that close relatives denied the severity of their illness and treatment, avoided discussing the illness and showed discomfort when discussing the illness.
Denial
A few of the study participants stated that some of the family members and friends had difficulty in accepting their diagnosis. A middle-aged man (P 3) suffering from Stage IV alveolar cancer reported that his wife left him after he was diagnosed with cancer. He did not have anyone to look after him, though his neighbors took him to hospital occasionally. A woman (P 6) suffering from the disease shared an experience with a friend who asked her, “Do you really have cancer?”
A few of them also stated that the close relatives denied understanding the severity of the cancer treatment. One man (P 22) shared, “when I told my friend regarding my disease, he said, Cancer is Ok, you will just need to take some chemo (chemotherapy)”. Statements like these resulted in a loss of emotional intimacy in their relationships.
Avoidance
Few of the participants reported that the close relatives avoided discussing the illness and prognosis. “My friend started avoiding me after I was diagnosed with cancer, maybe he thinks I will ask for money for my treatment”, said one of the cancer patients.
Many of the participants tried to avoid their illness-related disclosure to their near and dear ones in an effort to protect their close ones from emotional stress. One of the participants (P 22) said, “I do not want to make my wife upset regarding my illness, so, I pretend to be alright most of the time, though, I suffer from pain and other problems.”
Discomfort
A few of the participants stated that many of their family members were not comfortable discussing issues of their illness to other people and this very attitude of near and dear ones caused them (the patients) discomfort in expressing their own views and sharing their current health status with family and friends. One of the participants expressed her frustration and loneliness following awkward conversations with family and friends regarding her illness.
Felt stigmatized
A 65-year-old male (P 23) who was suffering from Stage IV oral cancer said that he was suffering from oral ulceration for quite a long time and his village doctor had told that it may be a harmful disease like cancer and he should consult a specialist without any delay, but he was stigmatized if he should visit a specialist for this and what will people and his family think if it was really oral cancer. As a result of which, he did not visit a doctor and presented to the hospital in advanced stage of the disease, when all options for treatment were over, and palliative care was the only option left.
Theme 3: Concern regarding financial security and public support
Cancer is a disease that demands for huge out of pocket expenditure for all the phases of the disease, starting from the diagnosis to the follow-ups. “Though we got the benefit of Rajiv Gandhi Jeevandayee Yojna (at present known as Mahatma Jyotiba Phule Jan Arogya Yojana[8]), but I had to spend more than one lakh (Rupees) on my treatment, for which I had to take loan from the local money lender at high interest”, said a cancer patient (P 24) on follow-up therapy. Similar views were also shared by most of the patients of oral cancer.
Awareness regarding the availability of treatment of oral cancer is still lacking. People are still not aware regarding where they can get treatment. Most of them are of opinion that it is only the big hospitals like Tata Institute, Mumbai, where cancer treatment is available. This resulted in lack of confidence in the allopathic treatment of cancer; many patients reported visiting different places for indigenous treatment of cancer.
Theme 4: Concern regarding eating
Eating is a fundamental aspect of our life, and it has been found to be greatly affected by oral cancer. It is not only that they do not get taste to the food; they cannot chew it and swallow it. Few of the included study participants were on ryles tube feeding through which they were fed with liquid food and fruit juices. One of the patients (P7) also said that,” I don’t feel the urge to eat now…. It does not only increase my pain while chewing and swallowing, but also causes embarrassment in front of others”. Sticky saliva, drooling, and dry mouth are the other common complains of oral cancer patients that they experienced after their treatment was completed.
The findings of the qualitative study on the oral cancer patients are further illustrated in the concept map on the psychosocial impact of oral cancer on the patients as shown in Figure 1.
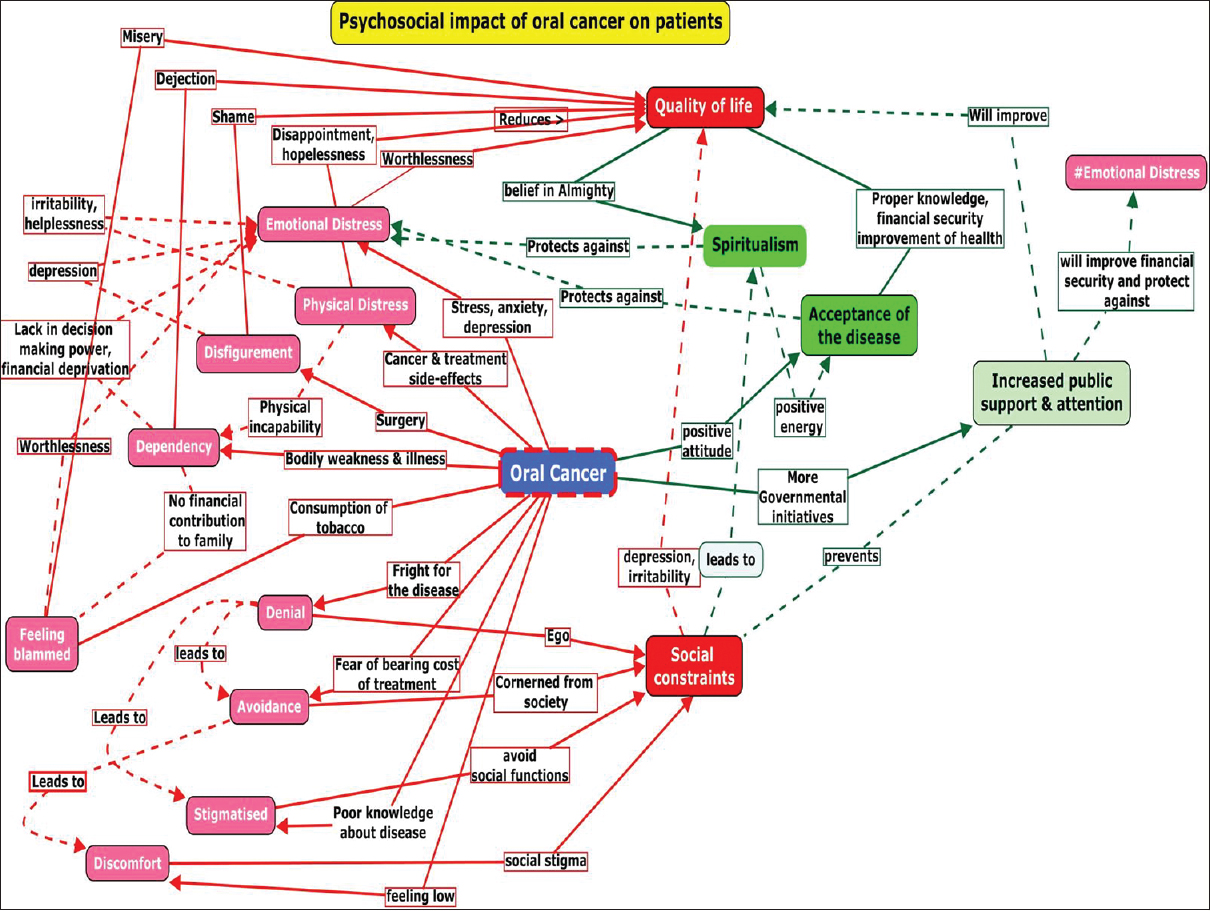
- Concept Map showing the psychosocial impact of oral cancer on patients. Color code: Red (box and arrow): Negative theme, Green (box and arrow): Positive theme, Pink (box): Negative sub-theme, Bold arrow: Direct association, Broken arrow: Indirect association
DISCUSSION
Our study came up with a variety of experiences shared by patients of oral cancer. The experiences included their physical problems, psychosocial implications of the disease, and organizational areas of life. At the time of interviews, most of the patients opened up in sharing their vivid experiences, some of which were positive while many were the negative experiences. This study was concerned with psychosocial impact of oral cancer on the cancer survivors and to help in suggesting recommendations for improvement of the impact.
First, patients expressed their worry regarding disfigurement in the face, for which they kept their face covered most of the time apart form avoiding any social gathering. Arunachalam et al.[5] had similar findings where they found visible disfigurements had a profound psychosocial impact on the patients. Disfigurement also has a negative impact on self-esteem, body image, and quality of life of the individual concerned. These findings were supported by studies conducted by Vidhubala et al.[4] and Chaturvedi et al.[9] Few of the participants, especially the females had shown their concern regarding hair fall and graying of hair following chemotherapy. Further, radiation therapy also resulted in burning of exposed skin of face and neck and made them permanently black. Van Der Donk et al.[10] did a detailed study on the change in quality of life in female patients as a result of hair loss, and they found a significant association between hair loss and negative impact on the quality of life of women.
Second, we found that oral cancer patients were also concerend regarding their inability to eat properly. Apart from increasing the cosmetic importance of face, oral cavity, and mouth are concerened with a number of important functions such as eating, chewing, swallowing, and talking. Patients of oral cancer who have undergone surgery suffer from a significant functional disability. They get embarrassed, as they cannot eat normally. Hence, many of them avoid community programs and stayed indoor mostly. Difficulty in eating food might be due to stiffness in the mouth as a result of fibrosis following radiation or surgical manipulations, or it might be due to the pain in the mouth or the jaw as a result of the diseases per se Many a times, teeth had to be extracted for treatment purpose making the oral cancer patients incapacitated to chew foods. Problems in swallowing could be mild to severe, where few people might eat solid food to few of them taking only liquid diet that too with ryles tube.[11] Improper diet often resulted in malnutrition and further deteriorated the health of patients. Gellrich et al.[12] shared similar opinion. They stated that malnutrition in oral cancer patients as a result of deficient diet resulted in a negative impact in the quality of life of the individuals.
Third, patients who had undergone treatment and were still suffering from its squeal were in stress and many of them were the undiagnosed cases of depression and anxiety. They were cut from the society, as they could not mix with people as they used to do previously. There had been reported cases of divorce after the individual was diagnosed with cancer. More over, most of the oral cancer patients were elderly who were already suffering from one or the other comorbid conditions. This ultimately increased the emotional distress. Dropkin[13] and Wu et al.[14] got similar observation as regards to anxiety and depression in head-and-neck cancer patients. Wu et al.[14] stated that cancer patients suffered from anxiety and depression in the first 6 months of their treatment and the different physical inabilities such as dysfunction in salivation, eating problem, and problems in maintaining social relationship increased the emotional stress in them.
Fourth, financial insecurity was found to be another major concern that came up from the IDIs. Oral cancers occur mostly among the male population in Indian scenario[15] and they are the prime bread earners of the families. This disease and its complications make them incapacitated for earning their livelihood resulting in cutting down of important routine family expenses such as postponement of marriages, change of schools of the kids, and change of profession. The elderly participants complained of the burden of dependency on their children as a result of the disease. All these factors acting together have a negative role to play in the life of the patients. Sharp and Timmons[16] found in their study that the cost of cancer treatment was huge. Wissinger et al.[17] did a systematic review on the economic burden of head-and-neck cancer to evaluate the evidence existing on the association of resource use and cost of the diagnosis and treatment of head-and-neck cancer. They have included 77 studies in their systematic review, where Wissinger et al.[16] found that treatment costs for head-and-neck cancers are generally high for cancers with advanced stages. Shankaran[18] in her study in financial impact on Cancer care found that cost for cancer care starts from the time of its diagnosis. A battery of important investigations has to be done after someone is diagnosed to have a cancerous growth. Chakrabarty et al.[19] in their study on the economic impact of oral cancer stated that in low- and middle-income countries like ours, where the most common mode of financing healthcare is out-of-pocket, causes a great pressure on household consumption level, and along with that the income loss due to sickness or death have impact on households finances.
Surprisingly, many of the patients came up with positive outlook regarding the occurrence of the disease and its consequences. More inclination to spiritualism, increased understanding of the pathology of the disease and acceptance of the disease helped the patients suffering from this deadly disease to cope up with all the consequences of oral cancer and its treatment. Kandasamy et al.[20] concluded in their article that spiritual well-being is a vital component of quality of life of the advanced cancer patients and was closely related to their psychological and physical distress. They have also recommended integrating spirituality into the management strategy of cancer, especially during palliation.
CONCLUSION
Treatment of oral cancer is beyond pharmacological and surgical interventions. The experiences of the study clearly points out the huge psychosocial and financial impact of the disease on the individuals that need to be addressed along with the continuum of care.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The global burden of cancer 2013. 2015. JAMA Oncol. 1:505. Available from: http://www.oncology.jamanetwork.com/article.aspx?doi=10.1001/jamaoncol.2015.0735
- [Google Scholar]
- Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-86.
- [Google Scholar]
- Pain complaint as the first symptom of oral cancer: A descriptive study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:56-61.
- [Google Scholar]
- Coping preferences of head and neck cancer patients – Indian context. Indian J Cancer. 2006;43:6-11.
- [Google Scholar]
- Quality of life in cancer patients with disfigurement due to cancer and its treatments. Indian J Palliat Care. 2011;17:184-90.
- [Google Scholar]
- Using reference data on quality of life – The importance of adjusting for age and gender, exemplified by the EORTC QLQ-C30 (+3) Eur J Cancer. 1998;34:1381-9.
- [Google Scholar]
- Scientific Sofware Development. ATLAS.ti 8 Berlin. :1-8. Available from: http://www.atlasti.com
- Government of Maharashtra. Mahatma Jyotiba Phule Jan Arogya Yojana: Government of Maharashtra 2012:47.
- Concerns, coping and quality of life in head and neck cancer patients. Support Care Cancer. 1996;4:186-90.
- [Google Scholar]
- Quality of life and maladjustment associated with hair loss in women with alopecia androgenetica. Soc Sci Med. 1994;38:159-63.
- [Google Scholar]
- Oral cancer malnutrition impacts weight and quality of life. Nutrients. 2015;7:2145-60.
- [Google Scholar]
- Anxiety, coping strategies, and coping behaviors in patients undergoing head and neck cancer surgery. Cancer Nurs. 2001;24:143-8.
- [Google Scholar]
- Anxiety and depression in patients with head and neck cancer: 6-month follow-up study. Neuropsychiatr Dis Treat. 2016;12:1029-36.
- [Google Scholar]
- Indian Council of Medical Research. Consolidated Report of Hospital Based Cancer Registries An Assessment of the Burden and Care of Cancer Patients: 2012-14. 2013. Available from: http://www.ncrpindia.org/
- [Google Scholar]
- The economic burden of head and neck cancer: A systematic literature review. Pharmacoeconomics. 2014;32:865-82.
- [Google Scholar]
- The Financial impact of cancer care : Implications and potential solutions. Am J Manag Care. 2015;21(SP16):SP547-SP550).
- [Google Scholar]
- Economic burden of cancer in India. 2017. Indian J Public Health Res Dev. 8:137. Available from: http://www.indianjournals.com/ijor.aspx?target=ijor:ijphrd&volume=8&issue=3&article=026
- [Google Scholar]
- Spirituality, distress, depression, anxiety, and quality of life in patients with advanced cancer. Indian J Cancer. 2011;48:55-9.
- [Google Scholar]






