Translate this page into:
The PEP Project - Synergistic Community Based Action in Prevention, Early Detection and Palliative Care, to Impact the Cancer Burden in India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
With unprecedented surge in the incidence and prevalence of cancer in India, it has become imperative to strengthen the workforce for all the domains of cancer care. A large proportion of the activity required for prevention as well as for palliation, lie outside of tertiary institutions, in the community. Palliative care (PC) as a field is expanding exponentially across the country and the service providers often engage and work actively within the local community in their region. This article describes the scope for reducing the cancer burden in the community, through capacity building of community based PC healthcare functionaries in the domains of Prevention, and Early detection of common cancers along with Palliative care – the PEP domains. It suggests aligning and enhancing the workforce already active within the community for PC, for screening, and if feasible, for early detection of common cancers. The article describes possibilities of initiating PEP activities and offers a set of screening questionnaire that may be used when engaged with family/ community setting. The aim is to integrate the activities done, to detect the need for palliative care in a family / community, with that required to detect need for evaluation of most common cancers- oral, breast and cervix. The PEP concept may be adapted to different levels, based on the team presence in the communities, degree of engagement, and availability of trainers and healthcare personnel.
Keywords
Prevention
early detection
palliative
comprehensive care
community palliative care
cancer burden
INTRODUCTION
In India, the estimated burden of cancer was over 1 million in 2012. This is projected to increase to 1.7 million by 2035.[1] The projected deaths due to cancer by then is 1.2 million.[2] In the Million Deaths Study, 71% cancer deaths occurred in people aged 30–69 years. About 80% of cancer patients present at tertiary cancer center with advanced disease,[3] not amenable to curative interventions. This was the disastrous consequence of cancer control policies that emphasized mainly to escalate the capacity for cure alone, without adequate strengthening of public health measures for screening and early detection of common cancers.
The field of palliative care (PC) developed largely to improve the quality of life of patients with advanced cancer, who suffer from an array of complex symptoms including severe pain, breathlessness, delirium, and psychosocial distress that require access to good quality care services within the community they live in. Yet, with just under 1000 PC centres, mostly spread outside the cancer hospitals, 96% of those who need PC in India do not have access to it even when they reach tertiary cancer centers seeking help.[4] Identifying these distressed patients in the community, aligning and providing them access to good pain relief and PC services, is a critical component for ensuring comprehensive cancer care and reducing the burden due to cancer.[5]
While the PC community focuses efforts to improve access to PC services for patients in advanced stages of cancer, it is important to remember that these patients could have been cured if only they had the opportunity to reach the cancer care facility earlier. By convention, the need for contributing to early detection of common cancers early, has not been perceived as a direct responsibility by the PC teams. This article suggests simple interventions to align our ongoing efforts in the community for improving access to PC, with the crucial efforts needed at the other end of the spectrum, i.e., early detection.
The three most common cancers in India – breast, uterine cervix, and oral cavity have well-developed interventions for early detection and have clear precancerous stages that are amenable to secondary prevention.[6] Therefore, screening and early detection of these three cancers would markedly reduce the cancer burden in India.[7] It is by strengthening the capacity of local communities in understanding and addressing concerns at both ends of the spectrum that a reduction of the public health burden due to cancers becomes possible.
We hypothesize that activating and empowering healthcare functionaries working in the community, with skills in Prevention, Early detection along with PC- the PEP areas, would reduce the cancer burden of the nation in general and that of the region in particular.
The logistics and skills for surveying and detection of cancers of oral cavity, cervix, and breast are easily trainable. There are ready modules and mentoring processes, including online facilities, for early detection of the three identified common cancers in India.[8] Furthermore, screening, early detection as well as palliation, require activities within the community, outside of oncology centers. Several state health departments in India are currently engaged in activating processes to strengthen the capacities for early detection as well as palliation in their regions, but through processes that are unconnected to each other.
This article describes the scope for reducing the cancer burden in the community, through capacity building of sets of community-based PC professionals in the PEP areas [Figure 1].
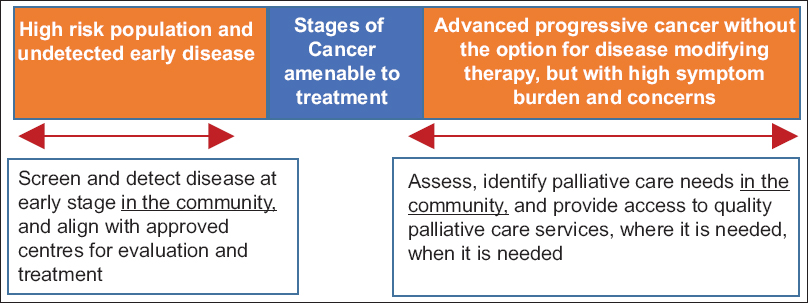
- The scope of the prevention early detection palliative care project
How does a palliative care organization venture into strengthening PEP capacity?
Any organization that is currently engaged in PC work, with community engagement and home visits being a part of their mandates, may consider expanding their scope of work by integrating PEP. The first step would be deciding the degree of involvement.
Activating community-based healthcare functionaries of existing PC centers, be it multipurpose healthcare workers or trained volunteers, and expanding their scope of work to administer screening and early detection questionnaire in the communities they serve, is a simple and valuable strategy with immediate tangible results. This requires a very brief training to help the community health workers understand the relevance and approach to administering the questions and the process for submitting the reports. A sample questionnaire is attached as Appendix 1.
To ensure that those identified from the community get access to appropriate evaluation and follow-up, the PC center should maintain the list of institutions in the region engaged in early detection work, and guide the persons identified from community, requiring further evaluation for early disease, to the appropriate services.
What are the other, deeper ways of integrating the PEP concept?
PC centers with adequate staff and greater presence in the community can consider incorporation of screening and facilitating early detection to strengthen their core mandate – that is averting suffering, by preventing people from reaching the PC stage. This level of involvement would require upgrading of the knowledge-skill base of their core team members through a bridge training in screening and early detection so that their community-based activities are conducted with a renewed PEP focus.
The contents of training would at the outset include knowledge and skills required for screening and early detection of the most prevalent cancers (oral cavity, cervix, and breast), in addition to the core principles of PC- Appendix 2.
PC centers in India often conduct training as an integral activity, where in-service doctors and nurses from many parts of the country come to learn the skills for providing PC. Such centers could consider inclusion of modules on prevention and early detection within their academic curriculum. This could be yet another level of PEP integration. The trainees in turn would get empowered in a wider spectrum of competence and reflect it as PEP activities in their own regions.
STRENGTHS AND OPPORTUNITIES OF THE PROJECT
The core PEP activities are in the community, with multidomain, yet simple interventions. After a brief training, the same set of healthcare functionaries who are already working within the community, would implement this valuable spectrum of activities. Institutional and technology support feature-in later, only once persons are identified to be at risk with suspicious history or lesions. Combining the concepts of prevention, early detection, and palliation together makes the learning comprehensive, relevant, practical, and interesting to the healthcare functionaries. Furthermore, regular PEP training sessions establishes new sets of functionaries, with a useful range of cancer-related skill set within the healthcare system.
PEP implementation for any center that is currently involved only in PC would require strategies at three levels - Box 1.

This project requires acceptance, planning, training, implementation, monitoring, and a modest budget allocation to succeed.
CHALLENGES AND LIMITATIONS OF THE PROJECT
The frontline workers in both preventive and palliative aspects are few and far. Even the minimal training required for expanding their work to the extra PEP areas poses several challenges: (i) by convention, the two areas have worked independently, (ii) the trainers for the newer PE dimension may not be accessible within the same region, (iii) integration would lead to increased workload of the field staff and intensified monitoring, and (iv) resistance to change the established ways of functioning may also be expected. Lastly, due to the limited number of approved centers and professionals trained in evaluating and treating the suspected precancerous lesions in our country, aligning early diagnosed persons with the appropriate therapy, is another important challenge.
Yet, the principles of proactive care, reaching out to the community and reducing the potential and/or actual suffering that drive the two fields, are in total alignment. Simultaneous field implementation of PEP activities can be the right force for reducing the cancer burden in our communities. The survey and educational contents that are shown in the appendices require to undergo the Delphi process for appropriateness for widespread application and to officialize their relevance.
What may be the impact of PEP based intervention?
The expected outcomes of PEP interventions are (i) improved primary and secondary level prevention, (ii) timely detection and early referrals for cure along with (iii) reduction of cancer burden in the region. Once the teams with ‘preventive’ focus align with the concept and begin to incorporate PEP activities, the palliative care needs in the community they serve, would emerge. This can lead to initiation of new PC services and serve to enhance access to this essential component of care.
Training in the PEP areas would strengthen the practitioner's existing skills and knowledge at both ends of the cancer spectrum for the most relevant cancers. They would be screening for early disease, while simultaneously evaluating for the supportive care needs of patients in their communities. For the grass root functionaries, PEP activity would help enhance their professional profile in the community. It would also address the unfamiliarity aspects of cancer care among community based professionals and improve interim care of patients with diagnosed disease. The level of professional satisfaction is very likely to increase.
The information and education provided as part of the PEP project can be expected to improve the overall cancer awareness amongst the public, and could eventually help reduce the epidemic of cancer. It is possible that the PEP questionnaire and/or contents of training get incorporated into the curriculum of community-based organizations working on any one of the elements of cancer control – be it screening, prevention, rehabilitation, or palliation, and eventually into the undergraduate curricula of medical and nursing professionals across the country. As the percentage detected early and accessing curative treatment improves, the trend of late detection and high prevalence of incurable disease would reverse. As earlier interventions are simpler and economical, the economic burden due to cancer may be expected to reduce.
WAY FORWARD
Considering the symptom load and the sufferings of patients with advanced disease and their families, it is the collective responsibility of providers engaged in preventive, curative, and/or PC activities, to join forces to stop and reverse the trend of late detection.
Integrating PEP is a feasible activity for every PC center that already provides home-based care and has an established presence in the community. The center could strengthen their own team's capacity in screening for cancer and facilitate early detection. A modest contribution from every PC team within their own territories could go a long way in reducing the cancer burden in the country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Dr Max Watson, Visiting Professor University of Ulster for the early encouragement on the PEP concept that helped us to develop the idea into a possible project for field application.
REFERENCES
- GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide. IARC Cancer Base No. 11. 2013. Lyon, France: International Agency for Research on Cancer; Available from: http://www.globocan.iarc.fr
- [Google Scholar]
- Prospective study of one million deaths in India: Rationale, design, and validation results. PLoS Med. 2006;3:e18.
- [Google Scholar]
- Improving cancer care in India: Prospects and challenges. Asian Pac J Cancer Prev. 2004;5:226-8.
- [Google Scholar]
- Predictors and prevalence of pain and its management in four regional cancer hospitals in India. J Glob Oncol. 2017;4:1-9.
- [Google Scholar]
- Civil society-driven drug policy reform for health and human welfare-India. J Pain Symptom Manage. 2017;53:518-32.
- [Google Scholar]
- Recommendations for screening and early detection of common cancers in India. Lancet Oncol. 2015;16:e352-61.
- [Google Scholar]
- 2016. Ministry of Health and Family Welfare, Government of India. Operational Framework. Management of Common Cancers. Available from: http://cancerindia.org.in/wp-content/uploads/2017/11/Operational_Framework_Management_of_Common_Cancers.pdf
- Cancer screening program using technology assisted learning. J Global Oncol. 2016;3(Suppl):23s.
- [Google Scholar]
Appendix 1: PEP Survey questions – The name of the Center
Name of the interviewer:
Country State
District:: Village:: House No:
Part 1- Palliative care Questionnaire
1. Is anyone in your family, suffering due to any illness since more than 3 months?
2. Is anyone in your family, unable to look after their own personal needs, due to a prolonged illness?
3. Is anyone in your family, unable to do regular work due to a prolonged illness?
4. Is there anyone in your family, who is mostly bed bound due to a prolonged illness?
If the answer to any of the above-mentioned questions is YES?
Is it because she/he is suffering from any of the following problems?
Breathlessness □ Pain □
Paralysis □ Confusion □
Vomiting □ Diarrhea □
Swelling □ Wound □
Bleeding □ Cough □
Constipation □ Difficulty in swallowing □
Unconsciousness □ Fits □
Old age-related weakness □ Fever □
Others □
Do you know the diagnosis of his/her problem?
Yes □
No □
Is she/he suffering from any of the following illnesses?
Heart disease □ Lung disease □
Paralysis □ Cancer □
Kidney disease □ Old age/loss of memory □
Neurological/brain disease □ HIV & AIDS □
Longstanding pain □ Congenital disease □
Mental illness □ Others □
What is the age and gender of the sick person/s?
<15 years □ 15–65 years □ >65 years □
Male □ Female □ Other □
Currently, where do you go for medical help?
Local Healthcare Worker/Primary Health Care/Vaidya/Private hospital/District hospital/Medical college/Cancer center/no help available
What kind of support are you looking for?
Medical/nursing advice and support □ Support to the family □ Emotional support □ Others …….………………
Part 2- Early detection of cancer questionnaire
Do we have permission to ask few health-related questions to each one of your adult family members? If YES
For all adults > 18 years
Ulcer in the oral cavity which is not healing but there for more than 3 weeks at the same site. □ White or red patch in the oral cavity □ Difficulty in tolerating spicy foods □ Sudden change is voice/hoarseness □ Difficulty in opening mouth □
For all women ≥ 30 years
Lump or thickening in the breast □ Constant pain in the breast or armpit □ Any change in the size of the breast □ Any change in the shape and position of the nipple □ Any retraction of the nipple □ Discharge from one or both nipples □ Puckering or dimpling of skin □ Swelling in the armpit □ Excessive bleeding during periods □ Bleeding between periods □ Postmenopausal bleeding □ Bleeding after intercourse □ Excessive/foul smelling vaginal discharge □
Appendix 2 – PEP Training Program contents
Learning Objectives
Contribute in preventing the disease within the community through information sharing, education, and encouraging lifestyle modification Use IEC material Incorporate skills to identify early disease, encourage, assist, and ensure that the patient accesses appropriate care. Focus on cancers with high prevalence, morbidity, and where reliable tools have been developed for screening/early detection – breast cancer, cancer cervix, oral cancers fulfill these criteria Maintain the basic approach and principles of providing supportive care for patients with cancers Be skilled to identify palliative care needs and continue to provide them at community-based settings
The contents of training
Prevention
Training on influencing habits, for example, tobacco, nutrition, exercise, and lifestyle Awareness on cost-effective vaccination and screening programs aimed at infection-related cancers such as cervical cancer (human papillomavirus).
Screening
To administer the survey questionnaire for screening the three cancers, and the next steps Database of early diagnostic centers from the region for utilizing for referrals Skills in clinical examination for detection of suspicious lesions – to detect leukoplakia, erythroplakia, submucous fibrosis, and clinical breast examination (CBE) for early detection of breast cancers.
Generalist Palliative Care – for trainee doctors and nurses
Communication skills – basics, breaking bad news, collusion Cancer pain management Managing common infections during disease-modifying therapy Symptom control in advanced disease – breathlessness, delirium Applying ethical framework in decision-making in advanced disease Managing end of life.






