Translate this page into:
Specialized Palliative Care and the Quality of Life for Hospitalized Cancer Patients at a Low-Resource Hospital in India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
This study aimed to compare the quality of life (QoL) of cancer patients, with an Eastern Cooperative Oncology Group (ECOG) performance of 3–4, in contact with or without contact, with a specialized palliative care unit (PCU) at a low-resource governmental cancer hospital, as well as studying the impact of this contact on the QoL in their caregivers.
Materials and Methods:
Hospitalized patients with an ECOG performance of 3 or 4 and their primary caregiver were asked to participate in this observational study. Patients in contact with the specialized PCU and their closest caregivers formed Group A, while patients and families without this contact formed Group B. Contact was mainly one consultation. The patients were asked to complete the Palliative Care Outcome Scale (POS), and the caregivers were asked to complete the Hospital Anxiety and Depression Scale (HADS) and the distress thermometer (DT).
Results:
There was no statistically significant difference between the median POS values of the patient groups, neither regarding the total sum nor per any item. There were also no statistically significant differences between the median HADS values and median DT values when comparing the caregivers to Group A and B.
Conclusion:
Consultation with a specialized PCU at this tertiary referral center did not alter the QoL of patients with an ECOG performance of 3–4 nor did it affect the psychological well-being of their caregivers. We argue that monitoring prescribed treatment and follow-up is a necessary component of PC.
Keywords
Eastern Cooperative Oncology Group
Hospital Anxiety and Depression Scale
palliative care
Palliative Care Outcome Scale
quality of life
INTRODUCTION
Quality of life (QoL) for cancer patients, most often called health-related QoL, is a broad term defining the different values in life.[12] It includes physical and psychological health, as well as existential issues and social concerns. Several methods to assess QoL in health care have been developed and validated. One example is the Palliative Care Outcome Scale (POS) that has been designed to assess QoL of patients in palliative care (PC). POS contains the different aspects of QoL including physical symptoms, psychological well-being, spiritual concerns, and psychosocial and practical considerations.[3456]
PC is defined as medical, psychological, and social support that improves the QoL of patients with a life-threatening illness, with entailing support to the family members.[7] The need for specialized PC can arise at any time point during the trajectory of a life-threatening disease. In the care of a cancer patient, pain management and symptom relief from disease-related issues as well as treatment side effects may be warranted alongside tumor-specific therapy given with a curative or life-prolonging intent. When oncological treatment is terminated or given with a palliative intent to decrease disease-specific symptoms, the care should focus on diminish suffering as well as support to the patient to enable a life as active as possible lived with dignity.[891011] Temel et al. showed that integrating early PC with standardized oncological treatment compared to standard oncological treatment alone among patients diagnosed with advanced lung cancer improved QoL and also prolonged survival in this group. In the study, the PC group had also less depressive symptoms measured by Hospital Anxiety and Depression Scale (HADS) compared to the standard care group.[12]
In India, nearly 1 million new patients are diagnosed with cancer annually and approximately 80% of the cancer patients will present at a late stage of their disease.[13] The public health-care system in India has limited resources and cannot provide PC to all patients in need of symptom relief.[1415] Although the Federal Republic of India has proclaimed that opioids should be provided in the management of cancer pain, many states in India lag behind, and there is, in general, a restricted access to legal opioids. This study focused on how PC is provided at a public tertiary cancer hospital in India.[16] Annually 10,000 new patients are admitted to the hospital and 110,000 patients come for follow-ups. The hospital services include radiotherapy, surgery, chemotherapy, pediatric oncology, and PC.[17] The PC unit provides medical treatment, nursing care, and counseling and has 90–120 patient appointments every day, whereof 30–40 inpatients and the remaining outpatients. In addition, patients can be admitted into a home-care program or to a separate hospice. This governmental cancer hospital is one of the few institutions in India to have been accepted by governmental drug controllers to supply opioid medication such as oral and intravenous morphine and fentanyl patches, and these medications are provided through the PC unit at the hospital.[18]
An earlier study at this hospital[19] found that, in 50% of the deceased in-house patients, there had been a contact with the PC unit for the treatment of symptoms. Hypothetically, there might have been a difference in the QoL of in-house patients depending on whether they have had contact with the PC unit or not. This study is a continuation of the above-mentioned study from 2017 with the objective to studying how contact with the PC unit affects the QoL of cancer patients with an Eastern Cooperative Oncology Group (ECOG) performance of 3–4, as well as the psychological well-being of their caregivers. The ECOG performance of 3–4 is defined as a patient that is bedridden more than 50% of the awaken hours and with a limited self-care capacity (ECOG 3), and patients confined to bed all day and without self-care capacity (ECOG 4).[20]
Aim
The aim of this study was to analyze the QoL of cancer patients admitted to the wards with a poor ECOG performance (3–4). Comparison was made between two groups of patients, those in contact with the specialized PC unit and patients without this contact. The second aim was to compare the psychological well-being of the caregivers to the patients in the two groups.
MATERIALS AND METHODS
The study was conducted in the spring of 2017, with data collected from February 24 to March 18. Participating patients were admitted to the hospital due to treatment or symptoms of advanced malignancies. Data were collected from five of the six adult oncology wards at the hospital the sixth was excluded because of denial to participate in the study. Patients included in the study were in-house cancer patients with an age of 18 years or older and an ECOG performance of 3–4. Tumor stage was not defined in the medical records in the majority of patients and could thus not serve as inclusion criteria.
The primary caregiver to every patient was also asked to participate in the study. All participants signed an informed consent.
Information regarding demographics, diagnosis, and medical treatment was collected from the patients. The patients were asked to complete the POS, and the caregivers were asked to complete the HADS and the distress thermometer (DT), addressing the psychological well-being. As there were high rates of illiteracy and low education among the study population, the questionnaires were read out load by a social worker. All interviews were held at the bedside of the patients, with the caregiver present.
The study population was divided into two separate groups: Group A without contact with the PC unit and Group B in contact with the PC unit. The PC unit resides in one appointment room at the hospital, with consultations for outpatients as well as for inpatients. Specialists in PC asses the need for symptomatic treatment and prescribe medication for pain and symptom relief, including opioids such as oral and intravenous morphine and fentanyl patches, as well as antidepressive and anxiolytic treatment. Patients are also offered counseling with social workers concerning existential and practical issues. However, follow-ups of the consultations are not possible due to the large number of patients. Thus, the patients themselves must initiate any further contact with the PC unit. The number of days since the last consultation as well as the medications prescribed for the patients in contact with the PC unit was documented in this study.
Palliative Care Outcome Scale
In the POS, the ten first items address physical symptoms, emotional and spiritual issues as well as psychosocial and practical matters.[721] Every item has five different answering alternatives, rated in a Likert scale from 0 to 4 [Appendix 1]. The ten items can be summarized to generate the maximum score of 40, with a higher score indicating less satisfaction with one's own overall condition and received health care.[21] The 11th item is an open question about the three main problems that the patient has experienced during the past 3 days. POS used in this study had previously been translated into Telugu and translated back into English by a third party to prove its accuracy, but it had not been validated in a larger study.
Hospital Anxiety and Depression Scale
HADS contains 14 items with two subscales for anxiety and depression [Appendix 2]. Every item has answering alternatives in a Likert scale of 0–3, and higher values indicate more symptoms of anxiety or depression. The maximum score per subscale is 21 and a score of 11 or above suggests clinically significant anxiety or depression.[2223] The HADS used in this study was translated into Telugu by a PC specialist at the hospital fluent in both Telugu and English.
Distress thermometer
The DT is a scale of 0–10 grading how much distress the person has felt during the past week [Appendix 3]. A score of 4 or above suggests clinically significant distress.[24] The DT used in this study was translated into Telugu by a PC specialist fluent in both Telugu and English. The DT was used in addition to HADS, as it is a simpler screening tool for psychological illness, to evaluate whether the results from the translated versions of the DT and HADS to Telugu would be congruent when comparing caregivers to Group A versus B.
Statistics
Statistical analyses were performed using the SAS Enterprise Guide Version 6.1 (SAS Institute, Cary, NC, USA). Statistical calculations found that the assumed true mean difference from POS between the two groups of participants was 3 units and the assumed pooled standard deviation were 6 units. Using these calculations, the sample size had to contain 128 participants to be able to reject the null hypothesis that the two groups would have equal POS results with 80% power. The probability of alpha error associated with this test would be 5%.
Results were presented using median values, and P values from the Mann–Whitney U-test, as the data in this study were not normally distributed. The two-sample t-test was used when calculating the age difference between the patient groups and the Chi-square test was used when calculating the difference in gender distribution between the patient groups. Graphs were performed by SPSS version 24 (IBM corporation, Armonk, NY, USA).
Ethical approval
Ethical approval was granted by the local Ethics Committee at the hospital. All participants signed their consent before participating in the study.
RESULTS
From a total of 500 in-house patients screened during the study period, 117 were older than 18 years and had an ECOG performance of 3–4. Out of the 117 patients, 41 declined participation, whereas 76 patients accepted and gave consent to participate [Figure 1]. Out of the 76 participants, Out of the 76 participants, 38 patients without any contact with the PC unit formed Group A, while the remaining 38 patients, who had contact with the PC unit formed Group B. Of the total 76 patients, three patients (two in Group A and one in Group B) were unable to be interviewed due to speech deterioration, and thus their caregivers were included in the study, as interpreters for the patients. Demographic data of the patients are shown in Table 1.
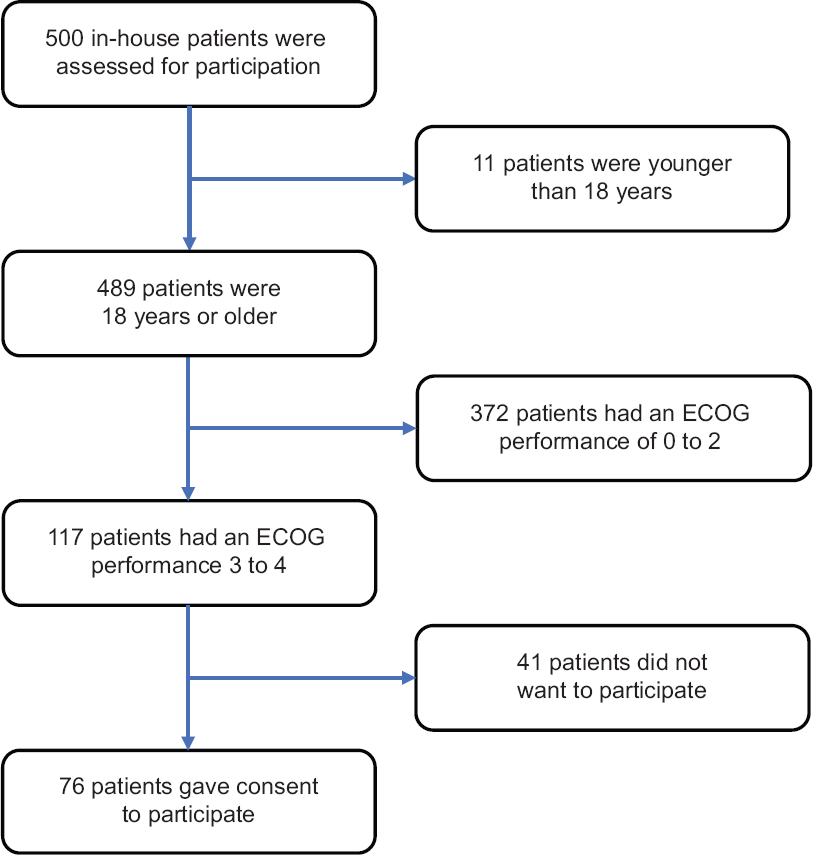
- Flow chart of the selection of the study population

For 74 of the 76 patients, a caregiver was present at the hospital and participated in the study. One of the caregivers did only complete the DT and not the HADS due to language difficulties. Out of the 74 caregivers, 34 were partners, 22 were children, 8 were parents, 6 were daughters-in-law, 2 were siblings, and 2 were brothers-in-law, to the patients. Demographic data of the caregivers are shown in Table 2.

The median number of days of the current hospitalization was 3 (range 1–60) days. Out of the 76 patients, 63 patients were aware of their diagnosis. In total, 66 of the 76 patients received tumor-specific treatment, and for 33 of the 76 patients, this treatment was documented as a palliative. For the remaining 43 patients, the medical records did not show whether the treatment was given with a curative or palliative intention. The median number of days since the last contact with the PC unit in Group B was 10 (range 1–111) days. There were no statistically significant differences between patients in Group A and B regarding age, gender, and knowledge of diagnosis nor ECOG performance [Table 1].
In Group A, one of the 38 patients had prescriptions for opioid analgesics and 10 of the 38% patients (26%) had prescriptions for nonopioid analgesics, compared to Group B where 19 of the 38 patients (50%) had prescriptions for opioids and 14 patients (37%) had prescriptions for nonopioid analgesics [Figure 2]. In Group A, no anxiolytics or antidepressants were prescribed to the patients. In Group B, 6 patients (16%) had prescriptions of amitriptyline as antidepressant and 8 patients (21%) had prescriptions of lorazepam against anxiety.

- Number of patients with various prescribed analgesics in Group A versus Group B
Palliative Care Outcome Scale
The median POS sum for Group A was 16.5 compared to 16.0 for Group B [Figure 3]. There was no statistically significant difference between the groups (P = 0.873). Pain was the main problem for patients in both Group A and B, in 81% and 86%, respectively [Figure 4]. No statistically significant differences were found between the groups when analyzing the median values of each item in POS individually [Figure 5].

- The Palliative Care Outcome Scale values in a box plot for Group A (no contact) versus Group B (in contact with the palliative care unit)

- Percent of patients in Group A (no contact with the palliative care) versus B (contact with the palliative care unit) stating the below-listed symptoms as their main problems during the past 3 days

- The median values of the Palliative Care Outcome Scale items for Group A (no contact with the palliative care unit) versus Group B (contact with the dipalmitoylphosphatidylcholine). Palliative Care Outcome Scale explores aspects of 1: The level of pain, 2: Other discomforting symptoms, 3: Anxiousness, 4: The family level of anxiousness, 5: Given information, 6: Sharing feelings with family or friends, 7: If life is worthwhile, 8: Self-esteem, 9: Time spent on health care without value, 10: Attentions on practical matters, respectively. See Appendix 1 for the items in palliative care outcome scale
Hospital Anxiety and Depression Scale
The median sum of the HADS depression subscale for caregivers to Group A was 14 compared to 13 for caregivers to Group B, [Figure 6]. There was no statistically significant difference between the groups (P = 0.286). In 58 of the 73 caregivers, a HADS score of 11 or above was found, which indicates a clinically significant depression.

- The Hospital Anxiety and Depression Scale values for caregivers to Group A versus Group B in a box plot
The median sum of the HADS anxiety subscale for caregivers to Group A was 12 compared to 11 for caregivers to Group B [Figure 6]. There was no statistically significant difference between the groups (P = 0.603). In 45 of the 73 caregivers, a HADS score of 11 or above was found, which indicates clinically significant anxiety.
Distress thermometer
The median DT value for caregivers to Group A was 8 compared to 7 for caregivers to Group B [Figure 7]. There was no statistically significant difference between the groups (P = 0.960). In 73 of the 74 caregivers, a score of 4 or above was found, indicating clinically significant distress.

- The distress thermometer values for caregivers to Group A versus Group B in a box plot
DISCUSSION
In the present study, we could not find any difference in the QoL among patients who had had a contact with the PC unit compared to patients without any contact with this unit. Furthermore, there was no statistically significant difference in the psychological well-being of caregivers to patients in contact with the PC unit compared to caregivers to patients with no contact with this unit. As anticipated, we found a variation in the prescription of opioid analgesics between the two groups, where patients who had contact with the PC unit to a higher extent had prescriptions of opioids compared to patients without contact. Accordingly, anxiolytic medications and antidepressants were only prescribed to the group in contact with the PC unit. Albeit this, no differences in QoL were seen between the two study groups.
There were no statistically significant differences among any of the items in POS between the patient groups. Pain is an important part of the POS score, albeit these patients who were in contact with the PC had an equal amount of pain as patients without this contact. This is surprising taken into account the differences in opioid prescription between the groups, as mentioned above. One explanation could be a selection bias, as this was not a randomized study, as has been discussed by Higginson and Evans advocating that selection bias might influence the data in nonrandomized control trials studying the effects of PC.[9] In the current study, we postulate that a bias in selection of patients to the PC unit might have modified the results as there might have been a difference in the severity of symptoms between the groups, and the group that was referred to the PC unit might have consisted of the patients with more pain than in the noninterference group. The interventions of the PC unit may have improved these patients’ QoL, but since we did not have any baseline information on the levels of pain before contact with the PC unit for this group, this was not possible to evaluate. Another, and plausible, explanation is that the prescriptions of medications, analgesics, and anxiolytics were not followed. Patients and families might not have understood the instructions, misconceptions or fear of opioids could hinder the proper use of medicines. To bear in mind, the majority of the patients in this study were illiterate. The complicated matters on the necessity of medicating regularly to achieve effect, as well as monitoring side-effects are demanding, in any setting, and require close follow-up and a high grade of availability, which was not possible to offer at the time of this study.
There was no statistically significant difference in the psychological well-being between the two caregiver groups, and this might be attributed to the absence of difference in QoL between the two patient groups. Fleming et al. found the mental health of caregivers to be positively correlated with the psychological well-being of the patients.[25] Importantly, in the present study, we have found that more than half of the caregivers had clinically significant levels of anxiety and depression, in concordance with a study showing that partners to lung cancer patients are under higher risk of developing symptoms of depression and anxiety compared to the general population.[26] In PC, it is regarded as important to assess the psychological well-being of the caregivers and to provide sufficient support to them in addition to the care provided for the patients.
Although we did not reach the planned number of included participants, thus leaving the study underpowered, there was no trend toward differences in any of the parameters studied and it is unlikely that any difference between the groups would have emerged even if the study would have included the planned number of patients. We thus find it likely that there is no difference to be found. Our results are in contrast with other studies where referral to PC was shown to improve the QoL and mood of advanced-stage cancer patients.[1327] The conflicting results between other studies and the present study is of importance. The needs for symptom-relief and PC are large and obvious in low- and middle-income countries (LMIC), and these results must be closely scrutinized. The ways in which symptom-relief is managed are as important as the access to necessary drugs. A follow-up of treatment adherence as well as monitoring of the effects and side effects of the prescribed medications is a key to obtain patients’ trust and to succeed with the treatment. Understandably, this will take time, resources, and requires a trained staff, all of which there is a shortage in the studied setting, in a LMIC. The need for medication is probably long-standing and patients can run out of drugs without having new prescriptions and further, patients need to be informed and educated on the necessity to follow prescriptions. The follow-ups of patients by the PC unit could thus be regarded as inadequate as some in-house patients had no prescribed pain medications during the present admission although they had had contact with the PC unit during an earlier hospital stay. More than 80% of the patients, in both groups, reported pain as their main problem during the last days before being interviewed. Although the World Health Organization has advocated the necessity of access to legal opioids to decrease the suffering from cancer pain, there is clearly a need of improvement in the treatment, not least in LMIC.[8] Overall, it has been estimated that only 3% of cancer patients in India receive adequate pain management.[28] The PC in India is at an early stage of development and is often hampered by limited access to morphine and other effective medication, as well as a lack of education in pain management.[1629]
There were some important strengths in this study. All participants were interviewed by the same person. Age, gender, ECOG performance, knowledge of diagnosis, education level, mean monthly income, and home settings were matched between the patient groups which eliminated any demographic differences between the groups that could have influenced the results. The translated versions of the DT and the HADS to the local language Telugu showed congruent results when comparing caregivers to Group A with caregivers to Group B. Limitations are obvious in this study due to the low-resourced setting. All patients and caregivers were interviewed bedside in crowded wards. Moreover, the translated versions of POS, HADS, and DT to Telugu had not been validated in larger studies.
We acknowledge that it is a challenge to provide PC to a large group of patients in a low-resource setting. The results in this study, with the limitations in the methods of evaluation, urge further activity. To establish regular consultations from the PC unit in the wards with follow-ups and adjustment of medications would raise the consciousness of the needs for PC and symptom relief, in general, at the hospital, as in other hospitals in the same situation, with underprivileged patients. This is a challenge in an already understaffed setting but is probably an essential part of the PC.
We also acknowledge the uncertainty of using QoL measurement tools originally constructed in high-income countries, with a different population. The used scales, HADS and POS, can, on the other hand, be viewed as global in their choices of subjects and are validated in large populations worldwide. There is a problem with illiteracy and unfamiliarity to the terms of the questionnaires, and even though forms were translated to the local language and in-house personnel took care of the questioning, there can be a problem for the patients to understand, during the interview. In addition, interviews were held at the busy wards, without guaranteed privacy, adding the problem of violating the integrity of the patients. On the other hand, this is the existing situation for the majority of patients in the world and must not hinder the development and progress. Small changes as repeated follow-ups of medication doses, information on effects and side effects, and repeated assessment of pain and associated symptoms, all to build a trustworthy relationship between caregivers and patients is one step ahead. As there is a lack of trained medical personnel, this prompts the training of paramedical assistants such as social workers already involved in counseling in many low-resource hospitals in LMIC.
CONCLUSION
The results from this observational study, with no effect on the QoL, are in contrast with other studies where referral to PC has shown to improve the QoL and mood in advanced-stage cancer patients and should be interpreted as a need for the development of the management of PC in the current setting. Alongside with the widespread lack of access to proper medications in LMIC, resources for training and education of staff are highly warranted. Raising awareness and knowledge amongst all involved in the PC is crucial to achieve treatment results. Our results highlight the importance of establishing routines for monitoring and follow-ups, as the core, of the care provided by a PC unit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to thank MNJIORCC, Hyderabad, for providing resources, and the patients and families participating in the study, making this work possible in the interest of future patients and families.
REFERENCES
- Definitions and conceptual models of quality of life. In: Lipscomb J, Gotay CC, Snyder C, eds. Outcomes Assessment in Cancer. Cambridge, England: Cambridge University; 2005. p. :14-30.
- [Google Scholar]
- Quality of life in patients with advanced cancer at the end of life as measured by the McGill quality of life questionnaire: A survey in China. J Pain Symptom Manage. 2014;48:893-902.
- [Google Scholar]
- The palliative outcome scale (POS) applied to clinical practice and research: An integrative review. Rev Lat Am Enfermagem. 2016;24:e2764.
- [Google Scholar]
- 2008. King's College London. Questionnaires and Tools: POS-Palliative Outcome Scale. United Kingdom: King's College London; Available from: http://www.kcl.ac.uk/lsm/research/divisions/cicelysaunders/resources/tools/pos.aspx
- 2012. POS Development Team. Palliative Care Outcome Scale. Cicely Saunders Institute. Avaialble from: https://www.pos.pal.org/
- Euroimpact. How should we manage information needs, family anxiety, depression, and breathlessness for those affected by advanced disease: Development of a Clinical Decision Support Tool using a Delphi design. BMC Med. 2015;13:263.
- [Google Scholar]
- 2002. World Health Organization. National Cancer Control Programmes: Polices and Management Guidelines. Geneva: World Health Organisation; Available from: http://www.apps.who.int/iris/bitstream/10665/42494/1/9241545577.pdf
- What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J. 2010;16:423-35.
- [Google Scholar]
- The effect of chemotherapy on health-related quality of life in mesothelioma: Results from the SWAMP trial. Br J Cancer. 2015;112:1183-9.
- [Google Scholar]
- Palliative chemotherapy: Oxymoron or misunderstanding? BMC Palliat Care. 2016;15:33.
- [Google Scholar]
- Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733-42.
- [Google Scholar]
- Development of palliative care in India: An overview. Int J Nurs Pract. 2006;12:241-6.
- [Google Scholar]
- Palliative care in India: Current progress and future needs. Indian J Palliat Care. 2012;18:149-54.
- [Google Scholar]
- Hospice and palliative care development in India: A multimethod review of services and experiences. J Pain Symptom Manage. 2008;35:583-93.
- [Google Scholar]
- 2007. MNJ Institute of Oncology. About MNJ. MNJ Institute of Oncology. Available from: http://www.mnjiorcc.in/
- Annual Report 2015-Activities of Department of Palliative Medicine, MNJIO&RCC. 2015. MNJ Institute of Oncology. Available from: http://www.mnjiorcc.in/
- [Google Scholar]
- Cancer treatment and end-of-life care. 2018. J Palliat Med. Available from: https://doi.org/10.1089/jpm.2017.0695
- [Google Scholar]
- ECOG-ACRIN Cancer Research Group. ECOG Performance Status. ECOG-ACRIN Cancer Research Group. 2016. Available from: http://www.ecog-acrin.org/resources/ecog-performance-status
- [Google Scholar]
- User's Guide to the Palliative Care Outcome Scale. 2002. Great Britain, London: Palliative Care and Policy Publications; Available from: https://www.pos-pal.org/maix/resources.php
- [Google Scholar]
- The hospital anxiety and depression scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14.
- [Google Scholar]
- The translation and evaluation of an urdu version of the hospital anxiety and depression scale. Acta Psychiatr Scand. 1991;83:81-5.
- [Google Scholar]
- Validation of the distress thermometer worldwide: State of the science. Psychooncology. 2014;23:241-50.
- [Google Scholar]
- Caregiving at the end of life: Perceptions of health care quality and quality of life among patients and caregivers. J Pain Symptom Manage. 2006;31:407-20.
- [Google Scholar]
- Depression, anxiety and disease-related distress in couples affected by advanced lung cancer. Lung Cancer. 2014;86:274-80.
- [Google Scholar]
- Determinants of quality of life in patients with advanced cancer. Support Care Cancer. 2011;19:621-9.
- [Google Scholar]
- Palliative cancer care ethics: Principles and challenges in the Indian setting. Indian J Palliat Care. 2010;16:107-10.
- [Google Scholar]
Appendix 1: Palliative care Outcome Scale

PATIENT QUESTIONNAIRE (version 1)
Patient name: ------------ Assessment date: ------------
Date of birth: ------------ Assessment no: ------------
Care setting: -------------------------
Please answer the following questions by ticking the box next to the answer that is most true for you. Your answers will help us to keep improving your care and the care of others.
Thank you.
Over the past 3 days, have you been affected by pain?
0 Not at all, no effect 1 Slightly - but not bothered to be rid of it 2 Moderately - pain limits some activity 3 Severely - activities or concentration markedly affected 4 Overwhelmingly - unable to think of anything else Over the past 3 days, have other symptoms e.g. nausea, coughing or constipation seemed to be affecting how you feel?
0 No, not at all 1 Slightly 2 Moderately 3 Severely 4 Overwhelmingly Over the past 3 days, have you been feeling anxious or worried about your illness or treatment?
0 No, not at all 1 Occasionally 2 Sometimes - affects my concentration now and then 3 Most of the time - often affects my concentration 4 Can’t think of anything else - completely pre-occupied by worry and anxiety Over the past 3 days, have any of your family or friends been anxious or worried about you?
0 No, not at all 1 Occasionally 2 Sometimes – it seems to affect their concentration 3 Most of the time 4 Yes, always preoccupied with worry about me Over the past 3 days, how much information have you and your family or friends been given?
0 Full information or as much as wanted – always feel free to ask 1 Information given but hard to understand 2 Information given on request but would have liked more 3 Very little given and some questions were avoided 4 None at all – when we wanted information Over the past 3 days, have you been able to share how you are feeling with your family or friends?
0 Yes, as much as I wanted to 1 Most of the time 2 Sometimes 3 Occasionally 4 No, not at all with anyone Over the past 3 days, have you felt that life was worthwhile?
0 Yes, all the time 1 Most of the time 2 Sometimes 3 Occasionally 4 No, not at all Over the past 3 days, have you felt good about yourself as person?
0 Yes, all the time 1 Most of the time 2 Sometimes 3 Occasionally 4 No, not at all Over the past 3 days, how much time do you feel has been wasted on appointments relating to your healthcare, e.g. waiting around for transport or repeating tests?
0 None at all 2 Up to half a day wasted 4 More than half a day wasted Over the past 3 days, have any practical matters resulting from your illness, either financial or personal, been addressed?
0 Practical problems have been addressed and my affairs are as up to date as I would wish 2 Practical problems are in the process of being addressed 4 Practical problems exist which were not addressed 0 I have had had no practical problems If any, what have been your main problems in the last 3 days?
------------------------------------------------------------ ------------------------------------------------------------ How did you complete this questionnaire?
0 On my own 1 With the help of a friend or relative 2 With the help from a member of staff
Appendix 2: Hospital Anxiety and Depression Scale

Appendix 3: National Comprehensive Cancer Network (NCCN) distress thermometer and problem list for patients







