Translate this page into:
Evaluation of Supportive Care Management Outcomes in Cancer Chemotherapy: A Prospective Observational Study in a Tertiary Care Teaching Hospital in South India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
Evaluation of supportive care management of cancer patients experiencing drug-related problems (DRPs) is a challenge because it might increase the cost due to additional therapy. The main objectives of this study were to estimate chemotherapy-associated drug-related hospital admissions in the department of medical oncology and to estimate the cost of managing chemotherapy-associated DRPs.
Settings and Design:
This study is a prospective observational study.
Subjects and Methods:
Patients with chemotherapy-related DRPs were prospectively identified from the patient's medical records. The contribution of DRPs and cost incurred due to each hospitalization was assessed.
Statistical Analysis Used:
Data were analyzed using SPSS® 20.0 version.
Results:
Out of 55 patients analyzed for DRPs, 25 (45.5%) patients in the age group of 51–60 years experienced DRPs most frequently. Most commonly occurring DRP was adverse drug reactions 42 (76.4%), which were more frequent in females. DRPs were maximum with alkylating agents 15 (27.3%) and the least with hormonal agents 1 (1.8%). The mean length of hospitalization was 9.6 ± 6.5 days. The total direct medical cost was Rs. 31,540 ± 42,476, of which medicine cost accounted for Rs. 16,550 ± 25,404, constituting a major share of the total medical costs.
Conclusions:
Pharmacists can provide better patient care by identifying and preventing DRPs and reducing drug-related morbidity and mortality.
Keywords
Adverse drug reactions
chemotherapy
drug-related problems
supportive care
INTRODUCTION
The World Health Organization (2015) survey reports cancer as the second leading cause of death in the world.[1] The Indian Council of Medical Research (ICMR) reports have estimated that the number of new cancer cases in India will rise to 17.3 lakhs by 2020 as against 14.5 lakhs cases in 2016.[2] Multimodal treatments available for cancer include chemotherapy, radiation therapy, surgery, hormonal therapy, immunotherapy, stem cell transplantation, targeted therapy, and more recently, precision medicines. While some receive a single mode of therapy, others require a combination of treatments such as surgery with chemotherapy or radiation therapy.[3] The goal of cancer chemotherapy is to improve disease-free survival or overall survival because adverse effects of anticancer medications can make patients extremely ill, uncomfortable, and compromise the quality of life. In addition, adverse events such as severe nausea and vomiting and neutropenia can postpone the next cycle of chemotherapy, lead to dose changes, resulting in poor clinical outcomes. Drug-related problems (DRPs) can significantly increase health-care cost.[4] Therefore, in cancer patients, supportive care is just as important as the treatment itself.
The National Cancer Institute (NCI), USA, defines supportive care as the care given to improve the quality of life of patients who with serious or life-threatening diseases. The ultimate goal of supportive care is to prevent or treat disease symptoms and also treat side effects related to its treatment.[5] Patients on anticancer chemotherapy may experience DRPs due to complications of polypharmacy and the toxicity of anticancer medications. Adverse drug reactions, drug–drug interactions, medication errors, and nonadherence are the most frequently reported DRPs and can be classified accordingly.[6]
The impact of DRPs can range from mild to fatal. Although DRPs are a major concern in cancer chemotherapy, most of the published studies on the incidence and economic impact of DRPs are not cancer-specific. Hospital admissions due to DRPs add to the already significant and ever-increasing cost of treating cancer. Unfortunately, the lack of research data on the incidence and economic impact of drug-related hospital admissions in cancer patients make it difficult for health-care providers to understand the extent of the problem.[7] Based on the aforementioned background, we carried out a study on chemotherapy-associated DRPs and hospital admissions in a tertiary care teaching hospital. We also estimated the cost of managing chemotherapy-associated DRPs, about which information is scanty, especially in India.
SUBJECTS AND METHODS
This was a prospective observational study conducted for 7 months (September 2016–March 2017) at a tertiary care teaching cancer hospital in Udupi District, Karnataka, India. Ethical permission was obtained from the Hospital Ethics Committee before the commencement of the study. We included patients of either gender admitted for supportive care management of chemotherapy-associated DRPs during the study period. Patients admitted for a course (cycle) of chemotherapy, radiation, surgical adverse events, psychosocial problems, adverse events due to nonchemotherapy medications, and patient's unwillingness to participate were excluded from the study. All the necessary and relevant data were obtained from patient's the medical records, including demography (age and sex), past medical-medication history, number of drugs prescribed, current diagnosis, vital signs, types of adverse effects, laboratory values, current medications information, cost of therapy, and length of hospital stay. Further information was gathered by interviewing the patient. Participant information sheet and informed consent forms were prepared in English and local languages (Kannada) for recording data. DRPs were identified by cross-checking the collected data with the standard established treatment protocol. ADRs and drug interactions were checked using Micromedex and Medscape. DRPs were classified and identified as per Pharmaceutical Care Network Europe (PCNE) (system version 5.0). The reported ADRs were assessed using Naranjo and WHO Causality Assessment Scale. The contribution of DRPs and cost of associated hospitalization were assessed. Direct medical cost was collected from the finance department of Kasturba hospital. Direct nonmedical expenses, such as cost of transportation and food, were gathered from the patient. Data were analyzed using SPSS® 20.0 version, IBM corporation, Armonk, New York, USA.
RESULTS
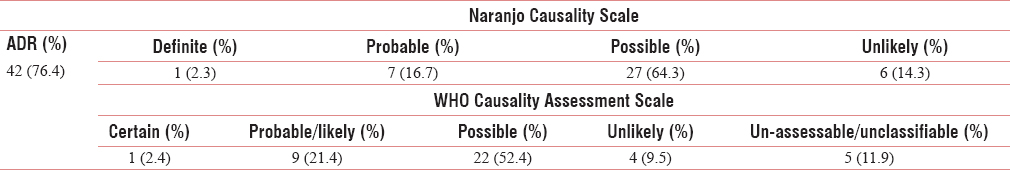
A total of 55 patients with DRPs were included in the study. Demographics of patients hospitalized for DRPs in cancer chemotherapy is shown in Table 1. Among the study population, 28 (50.9%) were male. The mean age of the study population was 51.1 ± 14.1 (mean ± standard deviation [SD]) years. DRPs were more frequent (25 [45.5%]) in the age group of 51–60 years compared to other age groups. The mean length of hospitalization was 9.6 ± 6.5 days (mean ± SD). Classification of DRPs versus gender is represented in Table 2. The incidence of ADRs (22 [52.4%]) and drug–drug interactions (2 [100%]) was more common in females. Unnecessary drug therapy was common in males and females (1 [50%]) as shown in Table 2. Disease characteristics of patients hospitalized for DRPs are reported in Table 3. There were 7 (12.7%) cases of breast and colon cancer. DRPs were reported more frequently in Stage II of cancer (22 [40%]) than stage I of cancer (4 [7.3%]). Cancer staging, under a broad-based category, irrespective of the clinical stage of disease, is depicted in Table 3. Types of comorbidities present in the study population are represented in Figure 1. Out of 55 patients identified with DRP's (30 [54.5%]) had comorbidities. Diabetes (10 [18.2%]) was the main comorbidity and paralytic ileus, intestinal obstruction, retroviral illness, and liver hemangioma were the least observed (1 [1.8%]). Complaints on the admission of the study population are depicted in Figure 2. The most commonly reported complaint on admission was fever (14 [25.5%]). Causality assessment of ADRs is done in our study population as represented in Table 4. ADRs (42 [76.4%]) were the most commonly reported DRPs in our study. Naranjo's ADR probability scale showed 27 (64.3%) were possible and 7 (16.7%) were probable. The WHO Causality Assessment Scale showed 22 (52.4%) were possible and 9 (21.4%) were probable. Chemotherapy cycles and anticancer drugs causing DRPs is represented in Table 5. Maximum DRPs were caused by alkylating agents (15 [27.3%]) and the least by hormonal agents (1 [1.8%]). Less than 3 chemotherapeutic agents were prescribed in 14 (25.5%) of patients and more than 3 in 41 (74.5%) patients. The mean length of hospitalization was 9.6 ± 6.5 days. In Table 6, total direct medical cost and total direct nonmedical cost were performed. The total direct medical cost was Rs. 31,540 ± 42,476. Medicine costs (Rs. 16,550 ± 25,404) accounted for a major portion of the total direct medical costs. The total direct nonmedical cost was found to be Rs. 750 ± 1780, in which transportation cost was Rs. 600 ± 1730 and daily food cost was Rs. 150 ± 100.




- Types of comorbidities present in the study population

- Complaints on admission of the study population


DISCUSSION
Supportive care is indicated when a patient is suffering from unresolved symptoms of the disease, severe side effects of therapy, or results in frequent hospitalization. In our study, the mean age of the population was 51.1 ± 14.1 years. Age group of 51–60 years developed more DRPs compared to other age groups. A study in Naïve Hospital in Northern Sweden reports higher age as one of the reasons for DRPs.[8] Female patients experienced more ADRs, drug–drug interactions, and inappropriate drug therapy. Hormonal changes in females are risk factors for ADRs.[9] Our study shows that both males and females are equally susceptible to DRPs. This contradicts a Study by Singh et al.[10] in India, showing females at higher risk for DRPs; 148 (52.3%). The variation between results could be due to the smaller sample size in our study population. In our patients, DRPs were higher in patients with carcinoma (32 [58.2%]) and least in sarcoma (2 [3.6%]). This is due to the variation in the treatment approach in its management. In carcinoma, chemotherapy or radiation therapy is the initial treatment, which is followed by surgery.[11] In sarcoma, the initial therapy is surgery followed radiation or chemotherapy.[12] In our study, DRPs were more frequent in stage II of cancer and least in stage I. While Type II diabetes (10 [8.2%]) was the most common comorbidity, in our study population, paralytic ileus, intestinal obstruction, retroviral illness, and liver hemangioma (1 [1.8%]) were encountered least. A study by Ayalew Sisay [13] in Ethiopia showed that 69 (88.5%) had comorbidities and the most commonly observed comorbidities were type 2 diabetics, HTN, and retroviral illness.[13]
The most commonly reported complaints on admission in our study were fever (14 [25.5%]) followed by GI disturbance (8 [14.5%]), abdominal pain (7 [12.7%]), and the least was shortness of breath (1 [1.8%]). A similar study done in Turkey by Gurbuz et al.[14] reported abdominal pain 344 (17.7%) as the most frequent complaint on admission followed by shortness of breath (273 [14%]), fatigue (194 [10%]), and fever (137 [7%]).[14] ADRs were the most commonly reported DRPs in our study. Causality assessment by Naranjo Causality Scale showed that 1 (2.3%) were definite, 7 (16.7%) were probable, 27 (64.3%) were possible, and 6 (14.3%) were unlikely. The WHO Causality Assessment Scale showed that 1 (2.4%) was certain, 9 (21.4%) were probable/likely, 22 (52.4%) were possible, and 4 (9.5%) were unlikely. A further 5 (11.9%) were unassessable/unclassifiable. Cancer patients often experience drug-related hospitalization owing to ADRs, with an average of 2.7 ADRs per admission. In addition to this, drug interactions were also reported as per a published study done in Brazil by.[15] Alkylating agents (15 [27.3%]) caused most of the DRPs and the least by hormonal agents (1 [1.8%]). A similar result was observed in a study done in India by Singh et al.[10] where DRPs were caused mostly by alkylating agents (40%). Less than three chemotherapeutic agents were prescribed in 14 (25.5%) patients and more than three chemotherapeutic agents were prescribed in 41 (74.5%). A similar study conducted in Singapore revealed that an increase in the number of prescribed drugs increases the chances of DRPs.[7] The total direct medical and nonmedical costs were also estimated. The mean length of hospitalization period was 9.6 ± 6.5 days. The total direct medical cost was Rs. 31,540 ± 42476, of which medicine costs of Rs. 16,550 ± 25,404 accounted for the major share. The total direct nonmedical cost was Rs. 750 ± 1780, of which transportation cost Rs. 600 ± 1730 and daily food cost Rs. 150 ± 100. A similar study conducted in Singapore highlighted the direct mean cost and length of stay per drug-related admission as Singapore Dollar 4747 and 6.1 days, respectively. Another study by Ko et al.[7] correlates longer hospital stay with greater probability of DRPs.[7]
CONCLUSIONS
Supportive care management for drug-related hospitalization is a challenge to our health-care system because it increases the cost burden to cancer patients. Our study revealed that DRPs are high among the elderly and with breast cancer. ADR were the most common problem among the DRPs and were higher in females. The presence of comorbidities in cancer patients increases the chance of adverse drug reactions. Medicine charges accounted for a major portion of direct medical cost. Direct nonmedical charges such as transportation and food add to the financial burden of cancer chemotherapy. Early detection of DRPs and providing suitable treatment for DRPs in cancer patients can improve patient care. Clinical pharmacists, who rarely participate in the health-care setup in India, can provide better patient care by identifying and preventing DRPs and reducing drug-related morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors of this article thank Department of Medical Oncology and Department of Finance, Manipal Academy of higher education, for providing required facilities to carry out this research work.
REFERENCES
- 2017. Cancer. World Health Organization. Available from: http://www.who.int/mediacentre/factsheets/fs297/en/.
- 2017. NCI Dictionary of Cancer Terms. National Cancer Institute. Available from: https://www.cancer.gov/publications/dictionaries/cancertermscdrid=46609.
- The costs of adverse drug events in hospitalized patients. Adverse drug events prevention study group. JAMA. 1997;277:307-11.
- [Google Scholar]
- 2017. Types of Cancer Treatment. National Cancer Institute. Available from: https://www.cancer.gov/about-cancer/treatment/types.
- Minimising treatment-associated risks in systemic cancer therapy. Pharm World Sci. 2008;30:161-8.
- [Google Scholar]
- Costs and length of stay of drug-related hospital admissions in cancer patients. Clin Ther. 2014;36:588-92.
- [Google Scholar]
- Characterisation of drug-related problems and associated factors at a clinical pharmacist service-naïve hospital in Northern Sweden. Drugs Real World Outcomes. 2017;4:97-107.
- [Google Scholar]
- Factors affecting the development of adverse drug reactions (Review article) Saudi Pharm J. 2014;22:83-94.
- [Google Scholar]
- Exploring troublesome symptom and problems experienced by cancer patients undergoing chemotherapy. J Young Pharm. 2016;8:220-4.
- [Google Scholar]
- 2017. Treating Squamous Cell Carcinoma of the Skin. Cancer.org. Available from: https://www.cancer.org/cancer/basal-and-squamous-cellskincancer/treating/squamousl-cell-carcinoma.html
- Preoperative, intraoperative, and postoperative radiation in the treatment of primary soft tissue sarcoma. Cancer. 1985;55:2659-67.
- [Google Scholar]
- Drug related problems in chemotherapy of cancer patients. J Cancer Sci Ther. 2015;7:55-9.
- [Google Scholar]
- Clinical analysis of the cancer patients who admitted to the emergency room. Biomed Res. 2016;27:641-4.
- [Google Scholar]
- Adverse drug reactions and drug interactions as causes of hospital admission in oncology. J Pain Symptom Manage. 2011;42:342-53.
- [Google Scholar]






