Translate this page into:
Is Every Life Worth Saving: Does Religion and Religious Beliefs Influence Paramedic's End-of-Life Decision-making? A Prospective Questionnaire-based Investigation
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Paramedics, arriving on emergency cases first, have to make end-of-life decisions almost on a daily basis. Faith shapes attitudes toward the meaning and worth of life itself and therefore influences decision-making.
Objective:
The objective of this study was to detect whether or not religious and spiritual beliefs influence paramedics in their workday life concerning end-of-life decisions, and whether it is legally possible for them to act according to their conscience.
Methods and Design:
This is a literature review of prior surveys on the topic using five key words and questionnaire-based investigation using a self-administered online survey instrument.
Settings/Participants:
Paramedics all over Germany were given the opportunity to participate in this online questionnaire-based study.
Measurements:
Two databases were searched for prior studies for literature review. Participants were asked about their religiosity, how it affects their work, especially in end-of-life situations, how experienced they are, and whether or not they have any legal latitude to withhold resuscitation.
Results:
A total of 429 paramedics answered the questionnaire. Religious paramedics would rather hospitalize a patient holding an advance directive than leave him/her at home (P = 0.036) and think death is less a part of life than the nonreligious (P = 0.001). Otherwise, the Spearman's rho correlation was statistically insignificant for all tests regarding resuscitation.
Conclusions:
The paramedic's religiosity is not the prime factor in his/her decision-making regarding resuscitation.
Keywords
Emergency care
palliative care
palliative emergency
INTRODUCTION
Religious belief is a very personal matter, which affects our private and our workday life on a daily basis. Human life is sacred to most of all the world's religions, but nonetheless bears the inevitability of death. The manner of how and when one dies was believed to lie in the hands of God, at least concerning the Abrahamic traditions. In the realm of modern medicine, however, our power over life and death has increased. Opinions on how far one should go, concerning medical treatment, to preserve or to save a life may differ.[1] The strength of one's religious belief varies from one person to another and thus may affect one's views and opinions toward life and death itself, this including medical topics such as abortion, preimplantation diagnostics, palliative medicine, emergency medicine, and more. Our investigation focuses on the prehospital treatment of terminally ill patients by German paramedics, highlighting the influence of the paramedics’ religious beliefs and the judicial framework they have to work in.
There is no consent in Judaism, Islam, and Christianity nor Eastern traditions (e.g., Hinduism and Buddhism) nor indigenous faith systems on opposing suicide, physician-assisted suicide, and euthanasia, but abstaining from life-prolonging procedures is usually allowed by religious authorities.[12345] Some religious people, for example, evangelical Christians in the US, seem to ask for life-prolonging procedures more often than nonreligious people.[167] In addition, Protestants were found to agree to euthanasia more than Catholics.[45] Apparently to some devout people, "Four commonly invoked reasons are (1) hope for a miracle, (2) refusal to give up on the God of faith, (3) a conviction that every moment of life is a gift from God and is worth preserving at any cost, and (4) a belief that suffering can have redemptive value."[8]
Paramedics making an end-of-life decision may be influenced by their religious beliefs. Since 3%–5% of all prehospital emergencies concern outpatient palliative emergencies, every paramedic may find himself/herself in the situation having to make an end-of-life decision.[9] Prior surveys showed that religious belief does influence physicians in their decision-making, concerning withdrawal of life-sustaining treatment and prescribing life-shortening pain medication and euthanasia.[610111213141516171819]
What also must be considered is the fact that paramedics are prohibited from withholding resuscitation by German jurisdiction, and therefore are obligated to initiate full resuscitation of patients with no vital signs, although they can of course express their opinions toward the physician's decision-making, if a physician is present.[9] If there is no physician present but there is an advance directive or do not attempt resuscitation (DNAR) order on scene, paramedics enter a jurisdictional gray area because they may either put aside such mentioned orders, being under time pressure, not being able to fully verify the order's authenticity, or they may adhere to its content in good belief of its genuineness. Only the presence of severe injuries, which are not compatible with life and/or definite signs of death (e.g., livor mortis), legally absolve paramedics from withholding resuscitation. This problem has been solved in England and Wales where the so-called Mental Capacity Act (2005) allows people to draw up an "Advanced Decisions to Refuse Treatment," such as resuscitation. Paramedics there are required by statutory law to respect this:[20] their guidelines permit them to withhold resuscitation when a formal DNAR order is in place, the patient is terminally ill, death is imminent and unavoidable, and resuscitation would not be successful.[21]
Our research hypothesis was that paramedics are influenced by their religious belief. To determine whether or not a paramedic's decision-making in end-of-life situations is influenced by his/her religious beliefs, how they decide given the current judicial framework, and how they would decide were there legal certainty are the main objectives of this study.
METHODS
Two databases, PubMed® and Google Scholar®, were searched for relevant prior investigations exploring the influence of religious and spiritual (R/S) beliefs on end-of-life decision-making using five keywords: End-of-life decision, spirituality, religious belief, palliative care, and resuscitation.
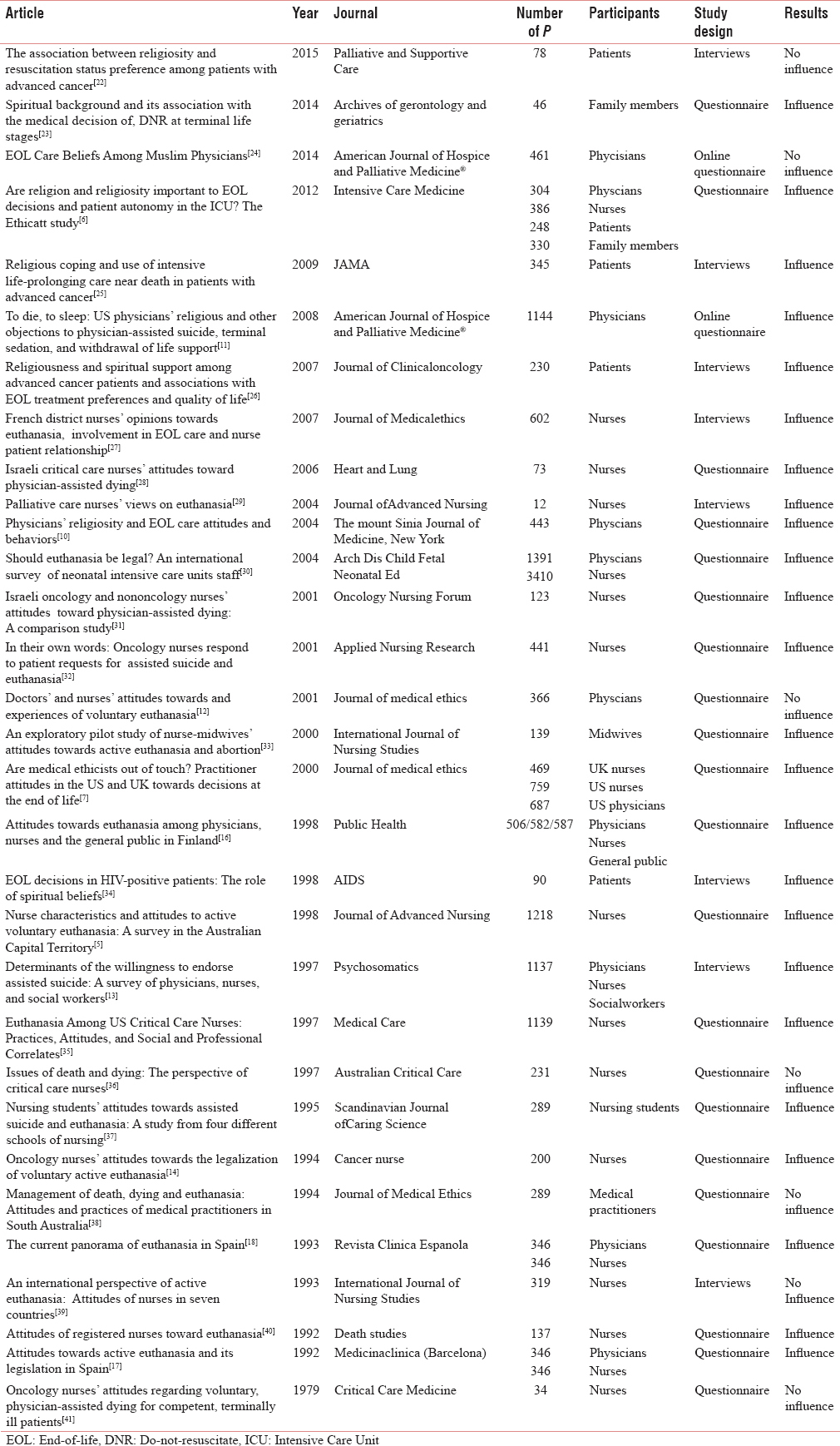
After duplicates were removed and the findings were screened according to abstract and title for their design and relevance to our study, 31 articles were included in the investigation [Table 1]. Two researchers, who took into account the number and type of participants, study design, and results, analyzed the papers found. The search was completed in May 2015.
A prospective questionnaire-based trial was used as the study design using the online tool “www.q-set.de.” In a pilot phase, the questionnaire was answered by 29 paramedics in written form, making sure the readability and appropriateness of the content. No modifications had to be made after the pilot testing. Afterward, the online questionnaire was accessible to paramedics all over Germany via links offered on the Malteser Hilfsdienst homepage (www.malteser.de), which is one of the big companies offering emergency services and on the Deutscher Berufsverband and Rettungsdienst. V. homepage (www.dbrd.de), which is the professional association of German paramedics, for 6 weeks (May 4, 2014). In this period of time, 400 paramedics answered the survey, the round number being sheer coincidence, ~7/day. The 29 written copies were included in the investigation for no changes had been made in the questionnaire. Participants who answered the written form were excluded from the online questionnaire to avoid double answers. Comments or a presentation were not given in advance to avoid bias mistakes. The information gathered in the questionnaire is summarized in Table 2.

Yes and no questions, free answers, and 11-point Likert scales were used for answers and tasks in the mixed methods questionnaire design. The Likert scales were interpreted as follows:
The median number of points plus/minus the standard deviation was interpreted as the average answers, the rest as extreme answers.
For example, with a median of 5 and standard deviation of 2, 7 people who answered 9–11 points on the question "Are you a religious person?" were rated as very religious and people who answered 1–2 points as not at all religious. The same interpretations were used for tasks, for example, 1–3 points as very insecure, 4–8 points as relatively confident, and 9–11 points as very confident.
Palliative care patients were defined as terminally ill patients with no hope of recovery, but who's symptoms and suffering can and must be alleviated and controlled (WHO Definition of Palliative Care).
Participants in the survey had to meet the following criteria: be an active member in an emergency ambulance service in Germany and participate in the investigation voluntarily. In accordance with the Declaration of Helsinki, all information was give anonymously.
IBM SPSS Statistics 22® (IBM Inc., Armonk, USA) and Microsoft® Excel® 2013 (Microsoft Inc. Redmond, USA) were used as software to analyze the gathered data. The Spearman's rho test was used to determine the association between two variables. P < 0.05 was considered statistically relevant for all tests. No Institutional Review Board approval was sought and obtained.
RESULTS
Twenty-seven studies investigated the influence of medical staff's R/S beliefs on their end-of-life decision-making concerning their patients. Five articles referred to patients,[622252634] two to family members,[623] one to social worker,[13] and one to the general public.[16] In none of them, or indeed in any other papers, did we find that paramedics had been questioned so that this is, to the best of our knowledge, the first investigative study of paramedics’ R/S beliefs and their influence on their work.
Eight articles used interviews, and 23 used questionnaires (two of them online) as the study design. The number of participants ranged from 12 to 4801, most of the investigations (20) had fewer than 500 participants. Seven studies showed no relevant influence of R/S beliefs on end-of-life decision-making[5122224363941] while the other 24 did indeed showed some.[576101113141617182325262728293132333435363740]
A total of 429 paramedics completed our survey. The median age was 31, the median work experience was 8 years, the median number of emergencies per years was 500 (5% of them being dying patients and 3% of them being palliative care emergencies), and the median number of resuscitations was ten per year. About 24.2% were not at all religious, 3.1% were very religious, and 72.7% were moderately religious [Table 3]. Nearly 25.3% of the participants rated themselves as nonbelievers, 10.1% as having strong religious beliefs, and 64.6% as moderately believing. Around 30.4% were not at all influenced, 20.1% were strongly influenced, and 49.5% were moderately influenced by religious values in their workday life.

Nearly 72.2% of the participants stated that palliative care had not been part of their training and 59.2% had not attended further education in palliative care medicine. Almost 42.4% had personal experience with a palliative care situation.
Altogether 59.9% doubted the sense of resuscitating a dying patient and 89% shared this view about resuscitating a dying palliative care patient. Nearly 77.7% considered it ethical not to resuscitate a dying patient and 91.8% not to resuscitate a dying palliative care patient.
A comparison between R/S beliefs (all categories included) and questions about the ethics of withholding resuscitation and the rationality of resuscitation and the hospitalization of palliative care patients produced two statistically relevant P values. Paramedics considering themselves to be religious (1) would rather hospitalize a patient holding an advanced directive than leaving him/her at home (P = 0.036) than nonreligious and (2) think that death is not a natural part of life itself (P < 0.001). Religiosity and strength of belief correlate with attitudes toward euthanasia. Religious and believing paramedics find (3) professionally- and (4) physician-assisted suicide unethical (P < 0.0001), as well as (5) institutions that offer it, for example, "Dignitas" from Switzerland (P < 0.0001), and (6) are against their introduction in Germany (P < 0.0001). There was no significant association between religiosity and the following questions: (7) "Is death a part of life?" (P = 0.072), (8) "Is every human life worth living, no matter the circumstances?" (P = 0.057), (9) "Would you resuscitate a patient who holds an advanced directive that clearly states he/she does not want to be resuscitated?" (P = 0.642), and (10) furthermore, there were no differences between the religious denominations and accordingly the nondenominational [Table 3].
There was a strong correlation between work experience and the following questions: (11) "Is death a part of life?" (P = 0.032), (12) "Is withholding resuscitation ethical?" (P = 0.048), (13) "Are you confident about treating palliative care patients medically?" (P = 0.026), (14) "Would you hospitalize a patient who holds an advanced directive?" (P = 0.001), (15) "Would you resuscitate a patient who holds a DNAR order?" (P = 0.002), (16) "Are you cognizant of how to handle advanced directives legally?" (P = 0.009), and (17) "Do you always act according to the law?" (P < 0.0001). More experienced paramedics think that death is more a part of life than the less experienced, furthermore they would not hospitalize a patient who holds an advanced directive, would not resuscitate a patient who holds a DNAR order, and think that they know the legalities of handling an advanced directive legally but at the same time do not always act according to the law.
Paramedics whose training included palliative care medicine or who attended further education in palliative care medicine were (18) more confident in handling advanced directives legally (P < 0.0001) and (19) were more competent in treating palliative care patients medically (P < 0.0001) and (20) psychologically (P < 0.0001) and (21) their relatives psychosocially (P = 0.008). Surprisingly, they found it more reasonable to resuscitate (22) dying patients and (23) palliative care patients (P = 0.003; P = 0.008) and (24) to withhold resuscitation less ethical. They also knew the local facilities for treating palliative care patients better than their colleagues (25), a fact that seems to be important because, the better the facilities are known to the paramedics, (26) the more confident they are in treating the patients medically (P = 0.021), (27) psychologically (P = 0.018), and (28) their relatives psychosocially (P < 0.001).
Paramedics who have personal experience with a palliative care patient in their private surroundings were (29) better equipped to treat patients’ relatives psychosocially (P = 0.027), but on the other hand (30) knew less of the local facilities (P = 0.002) and (31) had attended less further education on the topic (P = 0.001).
DISCUSSION
R/S beliefs can affect paramedics in judgment making, in our case concerning hospitalization, and can influence paramedics’ opinion on whether or not death is a part of life.
However, other factors impact the matter even more. The current law in Germany prohibits paramedics from withholding resuscitation (P < 0.001) even if there is a DNAR order on scene.[9] Similar results were discovered in a survey among Muslim physicians, where the country of origin and practice rather than R/S beliefs played the major role in end-of-life decision-making. The Sharia law in Saudi Arabia, for example, states that decision of DNR is left up to the treating physicians, whereas the law in the USA states that patient autonomy is the highest priority regardless of religion.[24] In our study, 76.6% of the paramedics stated that they had no legal latitude in withholding resuscitation in a dying and terminally ill patient. "Failure to render assistance," "legal uncertainty," "only a physician may declare someone dead, so I have to start," "fear of jurisdictional consequences," and similar reasons were given by the paramedics as to why they would start resuscitation. These answers were repeated throughout the survey. About 74.5% would not resuscitate a dying patient who has an advance directive or DNR order, were there given legal certainty.
Only 9.8% of the participants in our study think that they are competent to handle advanced directives in accordance with the law, a fact that correlates with their training in palliative care medicine (P < 0.0001), and 72.2% stated that they had not received any. Over half of the respondents in the survey on Muslim physicians did not receive training in palliative care medicine either.[24]
More experienced paramedics would not always act according to the law, for example, they would not hospitalize a patient holding an advanced directive, would not resuscitate a patient holding a DNAR order, and consider themselves competent in handling an advanced directive legally. Work experience must, therefore, also be seen as an influencing factor. These results differ from the survey on Muslim physicians, where no correlations between work experience and end-of-life decisions were found, but agree with the study of Younger's et al. conducted in the US, where a stronger correlation between professional background and attitudes toward euthanasia was found, and also Davis’ et al. study conducted in seven countries, where a negative correlation between work experience and holding to religious doctrines was found.[243941]
The paramedics’ abilities in treating palliative care patients medically and the patients’ relatives psychosocially depend on whether or not palliative care was part of the paramedics’ training and whether the paramedics attended further education and knew about the regional infrastructure for treating palliative care patients (P < 0.001; P = 0.021; 0.018; P < 0.001). The results of our research were absolutely comparable with those of the literature review. Study design, number and type of participants, and limitations were much the same as in the other investigations. Other studies, which showed influence of R/S beliefs, have in common that participants asked for more intensive treatment and more resuscitation and fewer life-shortening procedures for themselves or their patients.[6101123252634]
CONCLUSIONS
In summary, R/S beliefs can influence paramedics in their decision-making, but other factors, such as professional experience, professional background, special training, and legal frame work conditions, seem to have much greater significance.[243941] In Germany, the current law and the lack of training and knowledge in the ever-more important field of palliative care medicine are limiting factors. England and Wales could be examples for German jurisdiction, giving paramedics a legal frame work they can rely on, as a substitute to the current gray area.[20] In the training program for paramedics in Germany, which is currently being adapted, palliative care medicine, including the required knowledge of the law and local infrastructure, deserves, in our opinion, much greater consideration.
Availability of data and materials
All data and materials are available upon reasonable request. Please direct your request to Mr. Alexander Leibold via email: alexander.leibold@stud.uni-regensburg.de.
Limitations of the study
Reliability or validity testing was not applied to our survey study. Due to the unknown number of paramedics with access to the websites mentioned above, an accurate response rate could not be determined. As the survey completion was voluntary, bias may have affected the responses.
To increase the response rate, a game of chance was offered to participants with the opportunity of winning one out of three Amazon® vouchers. Participants could write their email address anonymously at the end of the questionnaire. www.random.org was used to determine the winners.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author would like to thank Mary Leibold for her language corrections and Frank Flake for providing access to the Malteser Hilfsdienst homepage (www.malteser.de) and the Deutscher Berufsverband and Rettungsdienst. V. homepage (www.dbrd.de).
REFERENCES
- An explanation and analysis of how world religions formulate their ethical decisions on withdrawing treatment and determining death. Philos Ethics Humanit Med. 2015;10:6.
- [Google Scholar]
- The world's major religions’ points of view on end-of-life decisions in the Intensive Care Unit. Intensive Care Med. 2008;34:423-30.
- [Google Scholar]
- ’There is a time to be born and a time to die’ (Ecclesiastes 3:2a): Jewish perspectives on euthanasia. J Relig Health. 2011;50:778-95.
- [Google Scholar]
- Nurse characteristics and attitudes to active voluntary euthanasia: A survey in the Australian Capital Territory. J Adv Nurs. 1998;28:70-6.
- [Google Scholar]
- Are religion and religiosity important to end-of-life decisions and patient autonomy in the ICU. The Ethicatt study? Intensive Care Med. 2012;38:1126-33.
- [Google Scholar]
- Are medical ethicists out of touch. Practitioner attitudes in the US and UK towards decisions at the end of life? J Med Ethics. 2000;26:254-60.
- [Google Scholar]
- "Inappropriate" treatment near the end of life: Conflict between religious convictions and clinical judgment. Arch Intern Med. 2003;163:1645-9.
- [Google Scholar]
- Paramedics experiences and expectations concerning advance directives: A prospective, questionnaire-based, bi-centre study. Palliat Med. 2012;26:908-16.
- [Google Scholar]
- Physicians’ religiosity and end-of-life care attitudes and behaviors. Mt Sinai J Med. 2004;71:335-43.
- [Google Scholar]
- To die, to sleep: US physicians’ religious and other objections to physician-assisted suicide, terminal sedation, and withdrawal of life support. Am J Hosp Palliat Care. 2008;25:112-20.
- [Google Scholar]
- Doctors’ and nurses’ attitudes towards and experiences of voluntary euthanasia: Survey of members of the Japanese Association of Palliative Medicine. J Med Ethics. 2001;27:324-30.
- [Google Scholar]
- Determinants of the willingness to endorse assisted suicide. A survey of physicians, nurses, and social workers. Psychosomatics. 1997;38:277-87.
- [Google Scholar]
- Oncology nurses’ attitudes toward the legalization of voluntary active euthanasia. Cancer Nurs. 1994;17:348-54.
- [Google Scholar]
- Attitudes of physicians, nurses and relatives towards end-of-life decisions concerning nursing home patients with dementia. Patient Educ Couns. 2006;61:372-80.
- [Google Scholar]
- Attitudes towards euthanasia among physicians, nurses and the general public in Finland. Public Health. 2002;116:322-31.
- [Google Scholar]
- Attitudes towards active euthanasia and its legislation in Spain. Med Clin (Barc). 1992;98:545-8.
- [Google Scholar]
- Oncology nurses’ attitudes regarding voluntary, physician-assisted dying for competent, terminally ill patients. Oncol Nurs Forum. 1993;20:445-51.
- [Google Scholar]
- Mental Capacity Act. Person who lack capacity. The Mental Capacity Act 2005:1-44.
- Joint Royal College of Ambulances Liaison Committee (JRCALC). UK Ambulance Service Clinical Practice Guidelines. Warwick: JRCALC; 2011.
- [Google Scholar]
- The association between religiosity and resuscitation status preference among patients with advanced cancer. Palliat Support Care. 2015;13:1435-9.
- [Google Scholar]
- Spiritual background and its association with the medical decision of, DNR at terminal life stages. Arch Gerontol Geriatr. 2014;58:25-9.
- [Google Scholar]
- End-of-life care beliefs among Muslim physicians. Am J Hosp Palliat Care. 2015;32:388-92.
- [Google Scholar]
- Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. JAMA. 2009;301:1140-7.
- [Google Scholar]
- Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol. 2007;25:555-60.
- [Google Scholar]
- French district nurses’ opinions towards euthanasia, involvement in end-of-life care and nurse patient relationship: A national phone survey. J Med Ethics. 2007;33:708-11.
- [Google Scholar]
- Israeli critical care nurses’ attitudes toward physician-assisted dying. Heart Lung. 2006;35:412-22.
- [Google Scholar]
- Should euthanasia be legal? An international survey of neonatal Intensive Care Units staff. Arch Dis Child Fetal Neonatal Ed. 2004;89:F19-24.
- [Google Scholar]
- Israeli oncology and nononcology nurses’ attitudes toward physician-assisted dying: A comparison study. Oncol Nurs Forum. 2001;28:50-7.
- [Google Scholar]
- In their own words: Oncology nurses respond to patient requests for assisted suicide and euthanasia. Appl Nurs Res. 2001;14:64-71.
- [Google Scholar]
- An exploratory pilot study of nurse-midwives’ attitudes toward active euthanasia and abortion. Int J Nurs Stud. 2000;37:505-12.
- [Google Scholar]
- End-of-life decisions in HIV-positive patients: The role of spiritual beliefs. AIDS. 1998;12:103-7.
- [Google Scholar]
- Euthanasia among US critical care nurses. Practices, attitudes, and social and professional correlates. Med Care. 1997;35:890-900.
- [Google Scholar]
- Issues of death and dying: The perspective of critical care nurses. Aust Crit Care. 1997;10:81-7.
- [Google Scholar]
- Nursing students’ attitudes towards assisted suicide and euthanasia: A study from four different schools of nursing. Scand J Caring Sci. 1995;9:119-22.
- [Google Scholar]
- Management of death, dying and euthanasia: Attitudes and practices of medical practitioners in South Australia. J Med Ethics. 1994;20:41-6.
- [Google Scholar]
- An international perspective of active euthanasia: Attitudes of nurses in seven countries. Int J Nurs Stud. 1993;30:301-10.
- [Google Scholar]
- Staff attitudes towards the care of the critically ill in the medical Intensive Care Unit. Crit Care Med. 1979;7:35-40.
- [Google Scholar]






