Translate this page into:
Validation of Malayalam Version of National Comprehensive Cancer Network Distress Thermometer and its Feasibility in Oncology Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
This study was designed to translate and validate the National Comprehensive Cancer Network (NCCN) distress thermometer (DT) in regional language " Malayalam" and to see the feasibility of using it in our patients.
Aims:
(1) To translate and validate the NCCN DT. (2) To study the feasibility of using validated Malayalam translated DT in Malabar Cancer center.
Settings and Design:
This is a single-arm prospective observational study. The study was conducted at author's institution between December 8, 2015, and January 20, 2016 in the Department of Cancer Palliative Medicine.
Materials and Methods:
This was a prospective observational study carried out in two phases. In Phase 1, the linguistic validation of the NCCN DT was done. In Phase 2, the feasibility, face validity, and utility of the translated of NCCN DT in accordance with QQ-10 too was done.
Statistical Analysis Used:
SPSS version 16 (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.) was used for analysis.
Results:
Ten patients were enrolled in Phase 2. The median age was 51.5 years and 40% of patients were male. All patients had completed at least basic education up to the primary level. The primary site of cancer was heterogeneous. The NCCN DT completion rate was 100%. The face validity, utility, reliability, and feasibility were 100%, 100%, 100%, and 90%, respectively.
Conclusion:
It can be concluded that the Malayalam validated DT has high face validity, utility, and it is feasible for its use.
Keywords
Distress thermometer
feasibility
Malayalam
validation
INTRODUCTION
Distress is highly prevalent in all stages of cancer.[12] Distress can occur at diagnosis, during treatment or posttreatment. It is multifactorial and can occur due to emotional, social, physical, or psychological problems that occur at, during or after cancer treatment.[12] Occurrences of distress are usually undetected in cancer patients. Undetected and hence, untreated distress may lead to noncompliance of patients to treatment, poor quality of life, and possibly poor survival outcomes.[34] Detection of distress at the time of its occurrence and early interventions to resolve it might increase the treatment adherence rate, improve the quality of life and may improve the survival.
The National Comprehensive Cancer Network (NCCN) developed a distress thermometer (DT) as a quick screening tool to identify actionable distress in oncology patients.[2] The NCCN DT is a single-item, rapid-screening instrument which asks patients to rate their distress on a scale of 0 ("no distress") to 10 ("extreme distress").[2] On an accompanying problem list, patients are asked to indicate what has been a problem for them in the past week. NCCN DT is taken up in the Western population, but it still remains the neglected care in the Indian population. The reasons for nonimplementations might be limited healthcare professionals. In a study conducted by Dessai et al. showed the use of NCCN DT in current form the DT could be offered to only 84.21% of patients who attended the outpatient department. The primary reason for difficulty in administration of NCCN DT was unfavorable health professional to patient ratio.[5] The doctor–patient ratio in the study was 43 patients per doctor. The nurse to patient ratio was 85 patients per nurse, while the nursing assistant to patient ratio was 34 patients per nursing assistant.[5] The DT is in English language and had to be translated by healthcare professionals to all patients. Hence, this study was designed to translate and validate the NCCN DT in regional language "Malayalam" and to see the feasibility of using it in our patients.
MATERIALS AND METHODS
Study design and conduct
This is a single arm prospective observational study. The study was approved by institutional review board. All patients provided written informed consents before participating in the study. The study was conducted in accordance with good clinical practice guidelines and Declaration of Helsinki. There was no amendment in the study protocol during the conduct of the study.
Study settings
The study was conducted at author's institution between December 8, 2015 and January 20, 2016 in the Department of Cancer Palliative Medicine. This study was done in two phases. In the first phase, the Malayalam translation of NCCN DT was done. In the the second phase, the completion rate, face validity, and feasibility were captured.
Participants
Phase I: Not applicable
Phase 2: Adult patients (age ≥18 years) with histopathological proof of malignancy, Eastern cooperative oncology group performance status 0–2, willing to comply with study instructions and who knew English and Malayalam language fluently were included.
Methodology
Phase 1
NCCNDT was translated into local language with a forward– backward translation procedure. Initially, the NCCN DT pro forma in English was translated forwards to local language by two translators who were fluent in English as well as the native target language and who had never seen the NCCN DT pro forma. The differences between the translations were reconciled and merged into a single forward translation with inputs from both the translators. Then, the forward translation was back-translated from local language to English by two different translators both of whom had command over the native target language and English and had not seen the original questionnaire. The backward translations were also reconciled following the previous procedure to generate a final translation. This translation was compared against the original English questionnaire. After we obtained the agreement between the original and backward translations, the questionnaire was taken forward to Phase 2A.
Phase 2A
Postvalidation of the pro forma, a pilot study was carried out in 10 patients (subjected to the same eligibility criteria mentioned in the protocol) to study the feasibility, face validity, completion rates and to identify difficult questions in case of completion rate been below 80%. Malayalam validated DT was self-administered to 10 patients and returned on the same day. Following return of this pro forma, QQ10 questionnaire was filled by the patients.[6]
Completion rate for NCCN DT was considered when distress level was marked and if more than 80% of problem list was completed. The feasibility and face validity were captured by QQ-10 pro forma.
Decision: If completion rate of 80% or more is achieved then the same pro forma subjected to minor corrections would be used for the final study (Phase 3). If not, the study would go to Phase 2B.
Phase 2B
This phase was planned if we had obtained < 80% completion rate in Malayalam validated DT. In this phase, the questions unanswered would have undergone simplification and difficult questions identified by QQ-10 questionnaire would be modified. These simplifications and modifications would have been done by a linguistic expert. Postmodification by the expert again the procedure in phase 2A would have been repeated.
If completion rate of 80% or more is achieved, then the same pro forma subjected to minor corrections would be used for the final study (Phase 3). If not, the study would go to Phase 2B again.
Sample size
Phase I: Not applicable
Phase 2: As this is a phase 2 study, for evaluating the feasibility, no formal sample size calculation was done. A sample size of 10 patients was decided adequate.
Statistical consideration
Pro forma in which 80% or more of the questions were completed was considered as complete. The completion rate was calculated as Mean completion rate = (completion rate of each patient)/10.
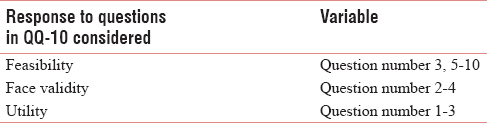
For consideration of feasibility face validity and utility the descriptive statistics of response to QQ-10 tool was done [Table 1].
RESULTS
Baseline demographics
The baseline demographic details of patients are shown in Table 2. As shown in Table 2, 40% of patients were male and 60% of female and had completed at least basic education up to the primary level. The primary site of cancer was heterogeneous. Sixty percent patients were unemployed and 20% were engaged in semi-skilled work and 20% in skilled work. Seventy percent of our patients were on curative intent treatment and 30% of patients on palliative intent treatment.

Completion rate of Malayalam validated National Comprehensive Cancer Network distress
Thermometer
The completion rate of Malayalam validated NCCN DT was 100%. All 10 patients completed >80% questions in the DT. The details of completion are shown in Tables 3 and 4.


Feasibility, face validity, and utility evaluation
The response to feasibility, face validity, and utility are shown in Figure 1. As can be seen from the figure, utility and face validity were 100% each and feasibility was 90%. All the patients (100%) considered the questionnaire relevant to their condition and covered all aspects of their condition. Similarly, all patients (100%) felt that it helped them communicate their problem with ease.

- Details of completion rate, utility, validity and feasibility
DISCUSSION
In the pilot study conducted in our institution, about the feasibility of using the NCCN DT in routine clinical practice, DT had identified actionable distress in 41.4% of patients.[5] It was noted in the study that DT not only identified the psychological issues but also the practical and physical problems leading to distress. However, due to the lack of manpower it was found not to be feasible to use NCCN DT in routine clinical practice. Similar circumstances exist in most of the cancer caring hospitals across low- and middle-income countries.[78] An increment in workforce seems the logical solution, but such increment has multiple logistic issues and do not easily happen in middle- and low-income countries. Hence, we considered the option of translating the NCCN DT in the native language. This we thought would enable us to self-administer the NCCN DT to the patients.
Self-administered Malayalam validated DT can be used to identify distress before the physician visit. It can be administered during the waiting period for physician appointment. This will save the physician time in a busy outpatients departments.
Distress can occur at various time points during the treatment or after completion of treatment. With a native language validated DT, distress can be measured at all timepoints during treatment and after it. The current study testifies the ease of use of such translated DT. The patient filled DT is to be immediately assessed by the treating physician to identify the actionable distress for appropriate referrals. This can be further simplified by using the electronic version which will score the patient's level of distress and physician can get the alert if the patient has got actionable distress. Timely interventions based on the type of distress may improve patients quality of life, treatment adherence, and the treatment outcomes.
The intervention of translating the NCCN DT in native language was based on the premise that NCCN DT will be socio culturally acceptable in India and the major factor behind its wide applicability is the low health professional to patients’ ratio. This assumption was based on the initial study conducted by the authors.[5] Although in that study specific questions considering culturally acceptability of NCCN DT was not tackled, health professionals were encouraged to report issues which they felt hampered the feasibility. Further in this study, none of the approached patients refused to fill the DT and in fact, they had indicated that they liked filling the NCCN DT. This information is important as this means that NCCN DT seems to be culturally acceptable by even non-English speaking population in India or across the world.
This study is not without limitations. The current study was carried out in the state of Kerala. The literacy rate of this state is nearly 100%. Hence, self administration of native translated DT was possible. In states with low literacy rate having an audio based questionnaire might be necessary for problem list. NCCN DT, however, might be useful for detection of distress on visual analog scale, as is the experience from scoring pain on visual analog scale.[9] The study had small sample size. The sample size was chosen according to convenience as the QQ-10 questionnaire used for validation required minimum 10 patients.[61011]
CONCLUSION
It can be concluded that the Malayalam validated DT has high face validity, utility, and it is feasible for its use.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank all staffs of Malabar Cancer Centre.
REFERENCES
- Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. 2003;1:344-74.
- [Google Scholar]
- Screening for distress can predict loss of follow-up and treatment in cancer patients: Results of development and validation of the distress inventory for cancer version 2. Psychooncology. 2009;18:524-33.
- [Google Scholar]
- Higher distress relates to poor quality of life in patients with head and neck cancer. Int J Oral Maxillofac Surg. 2009;38:955-9.
- [Google Scholar]
- Pilot study of single-day distress screening with the NCCN distress thermometer to evaluate the feasibility of routine distress screening in tertiary cancer center in rural India. Psychooncology. 2015;24:832-4.
- [Google Scholar]
- Development of an instrument to measure face validity, feasibility and utility of patient questionnaire use during health care: The QQ-10. Int J Qual Health Care. 2012;24:517-24.
- [Google Scholar]
- The global dissemination of psychological treatments: A road map for research and practice. Am J Psychiatry. 2014;171:495-8.
- [Google Scholar]
- Bridging the gap between financial distress and available resources for patients with cancer: A qualitative study. J Oncol Pract. 2014;10:e368-72.
- [Google Scholar]
- Utility of numerical and visual analog scales for evaluating the post-operative pain in rural patients. Indian J Anaesth. 2012;56:553-7.
- [Google Scholar]
- Assessment of the face validity, feasibility and utility of a patient-completed questionnaire for polymyalgia rheumatica: A postal survey using the QQ-10 questionnaire. Pilot Feasibility Stud. 2018;4:7.
- [Google Scholar]
- Development and validation of a questionnaire to measure preferences and expectations of patients undergoing palliative chemotherapy: EXPECT questionnaire. Indian J Cancer. 2016;53:339-44.
- [Google Scholar]






