Translate this page into:
Prevalence and Severity of Sleep Disturbances among Patients with Early Breast Cancer
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Data regarding health-related quality of life in breast cancer patients in the Middle East are limited with fatigue and sleep disturbance being the most distressing symptoms reported by patients treated for early breast cancer.
Aims:
The aim of this study was to examine the prevalence and incidence of insomnia among patients with early-stage breast cancer patients treated with chemotherapy.
Subjects and Methods:
This was a prospective cohort study. We enrolled patients with stage I-III breast cancer patients treated with chemotherapy at the American University of Beirut Medical Center. At three different time points (prior to, during, and following chemotherapy), we assessed the severity of sleep disturbances using the Pittsburgh Sleep Quality Index and the Insomnia Severity Index. The Institution Review Board approved the study.
Results:
Fifty-two patients were recruited. There was a significant increase in sleep disturbances during chemotherapy which improved to below baseline levels on completion of therapy. Prior to chemotherapy, 36% of patients reported poor sleep versus 58% during chemotherapy. The percentage of patients reporting clinical insomnia rose from 11% pretreatment to 36% during chemotherapy reflecting a significant symptomatic burden that is poorly documented and managed in routine clinical practice.
Conclusions:
Patients with nonmetastatic breast cancer experience an increase in sleep disturbances during the treatment phase. Physicians should be aware of the need to routinely screen for sleep disturbance in breast cancer patients undergoing chemotherapy.
Keywords
Breast cancer
insomnia
Insomnia Severity Index
Pittsburgh Sleep Quality Index
INTRODUCTION
The diagnosis of cancer and its treatment are associated with high levels of psychological distress. Insomnia is defined as the difficulty to initiate or maintain sleep for at least 1 month causing clinically significant distress and/or social and occupational impairment.[1] Insomnia is aggravated by cancer treatments and their side effects, and therefore should be proactively managed.[2] The burden of insomnia is multifaceted and affects several aspects of patient's quality of life. Patients suffering from insomnia are prone to fatigue, mood disturbances, poor performance at work, and dependence on sleeping pills.[3] The study of insomnia sheds light on an important underrecognized aspect of suffering among cancer patients.[4] In a Middle-Eastern society, the diagnosis of cancer remains a taboo and cancer patients are prone to an amplified burden of psychological distress associated with cancer diagnosis.[56] Breast cancer is the most common cancer diagnosis among women in the Middle East.[7] With a median age of diagnosis of 50 years, breast cancer affects both younger and older segments of the population in Lebanon. Data regarding insomnia or health-related quality of life in breast cancer patients in the Middle East are scarce. Two cross-sectional studies from Bahrain and Jordan have shown that fatigue and sleep disturbances are the most distressing symptoms reported by women treated for early breast cancer.[89] Another cross-sectional study from Jordan showed that fatigue was among the most distressing symptoms in female cancer patients receiving chemotherapy.[10] The aim of this study was to examine the prevalence and incidence of insomnia in early stage breast cancer patients.
PATIENTS AND METHODS
Study design and patients
This is a prospective cohort study of breast cancer patients referred for adjuvant or neoadjuvant chemotherapy at the Naef K. Basile Cancer Institute of the American University of Beirut Medical Center. The institution review board approved the study protocol. Patients were approached to participate in the period ranging between October 2013 and April 2014. A written informed consent was obtained. The inclusion criteria were (1) female patients, (2) above 18 years of age, and (3) planned for chemotherapy treatment for nonmetastatic breast cancer (Stages I–III). The exclusion criteria consisted of (1) significant psychiatric or noncancer medical illness, (2) concurrent use of medications known to affect sleep, and (3) night-shift employment. Demographic- and treatment-related information were collected prior to the first chemotherapy session. The Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI) were administered at 3-time points: Immediately prior to the first cycle of chemotherapy, during chemotherapy (between 2 and 3 months after starting treatment), and 1 month following the completion of chemotherapy. Our institution's institutional review board approved this study.
Questionnaires
The PSQI was used to assess subjective sleep quality over the month preceding the date of the interview. It is composed of 19 questions grouped into seven components sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, the use of sleeping medications, and daytime dysfunction.[1] Each question is scored from 1 to 4 depending on the frequency of the symptom during the past month, 1 – Never, 2 – less than once a week, 3 – once or twice a week, and 4 – three or more times a week. Scores were calculated for each patient according to a formula as per the PSQI scale. A total PSQI score of ≥5 indicates poor sleep quality.
The ISI was used to assess the subjective symptoms of insomnia as well as the distress caused by these symptoms over the previous month. It contains seven questions to assess sleep onset and sleep maintenance difficulties, satisfaction of current sleep pattern, interference with daily functioning, the ability of others to notice those problems, and the degree of distress or concern caused by these symptoms. Patients were asked to respond for each item on a scale of 0 (not at all) to 4 (very much) based on the extent at which they experience each problem during the last month.[11] A total ISI score of ≥7 indicates clinical insomnia. Both questionnaires were administered in the validated Arabic version.[12]
Statistical analysis
Descriptive statistics were performed. Paired sample t-tests were used to compare the means of the sleep scores at the three different time points of the study (prior to, during, and after chemotherapy). The P < 0.05 was considered the cutoff for statistical significance. All analyses were conducted using SPSS version 20 (IBM, NY, USA).
RESULTS
Patient characteristics
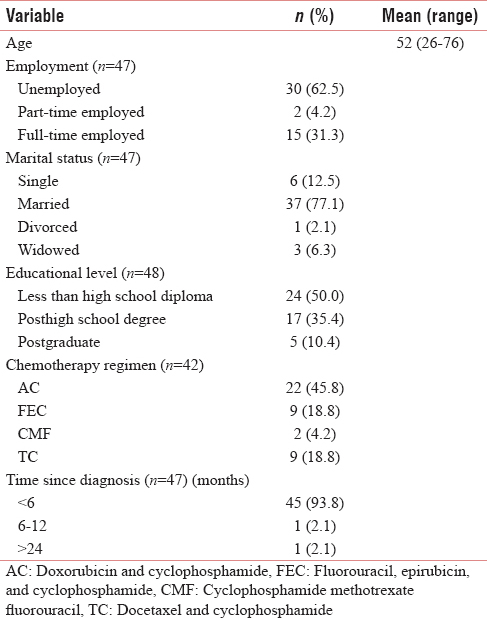
Fifty-two patients participated in the study; four patients did not complete the three-point interviews required by the study protocol and were subsequently excluded from the final analysis. The mean age of patients was 50.8 years (range: 26–76 years) [Table 1]. About 62.5% of the patients were unemployed while 31.3% were full-time employed and 4% were part-time employed. The majority of patients were married (77.1%). Half the patients (50.0%) had less than a high school diploma as their highest level of formal education. The majority of patients (93.8%) were diagnosed within 6 months of study enrollment. About 45.8% of patients were treated with adriamycin and cyclophosphamide, 18.8% with 5-fluorouracil, epirubicin, and cyclophosphamide, 18.8% with TC (docetaxel and cyclophosphamide), and 2.1% with other regimens.
Insomnia scores
Using the PSQI, the prevalence of poor quality sleep was 36.4% at baseline before starting chemotherapy and increased to 58.3% during treatment. It decreased to 32.1% (below the baseline level) 1 month after the end of chemotherapy. The mean PSQI scores mid-treatment and after treatment were significantly different from the baseline values (P < 0.05): 4.96 ± 3.82 at baseline, 7.81 ± 5.10 during chemotherapy, and 3.78 ± 3.81 after treatment [Table 2].

According to the ISI scores, the prevalence of clinical insomnia among patients increased from 11.1% before starting chemotherapy to 36.1% during treatment. Consistently with the PSQI results, the prevalence of clinical insomnia dropped back to 6.3% one month after finishing chemotherapy in this cohort. The mean ISI scores followed a similar pattern to the PSQI scores with statistically significant deviation from baseline values (P < 0.05): 0.40 ± 0.75 at baseline, 1.06 ± 1.12 during treatment, and 0.28 ± 0.58 following completion of therapy [Table 3].

DISCUSSION
Our study showed a significant increase in sleep disturbance in early breast cancer patients on chemotherapy and that subsequently improved to below baseline levels on completion of therapy. Prior to chemotherapy, 36% of patients reported poor sleep, and during chemotherapy, the prevalence rose to 58%. The percentage of patients reporting clinical insomnia increased from 11% pretreatment to 36% during chemotherapy reflecting a significant symptomatic burden that is poorly documented and managed in routine clinical practice. The median age of patients in our cohort was 50.8 years, consistent with previous data from the region.[7]
Our results are consistent with the previous studies where higher levels of sleep disturbance have been observed in women undergoing chemotherapy.[91314151617] However, a recent longitudinal study carried out in North America found a higher prevalence of sleep disturbance among female patients undergoing adjuvant chemotherapy for breast cancer: 48.5%–65.8% of patients had PSQI scores ≥5.[18]
In the Middle East, a cross-sectional study of breast cancer survivors in Bahrain reported significant sleep disturbances in 17.6% of women, ranking second after fatigue as the most distressing symptom assessed.[8] Similar results were obtained in a study from Jordan where 13.5% of breast cancer survivors reported clinically significant sleep disturbance, ranking second after fatigue.[9]
Our study is the first prospective study in the Middle East to assess sleep quality and the incidence of clinical insomnia in early-stage breast cancer patients using validated tools. Limitations include the small sample size and lack of additional measures such as the health-related quality of life (HRQOL). In another study, HRQOL measured by the Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire was found to be negatively correlated with global PSQI scores at each time point.[18] Despite these limitations, even in this relatively small cohort of women, chemotherapy treatment was shown to be associated with a significant increase in clinically significant insomnia.
Sleep disturbances in patients with breast cancer undergoing treatment are multifactorial. The direct psychological impact of the disease, cytotoxic chemotherapy, and concurrent medications such as corticosteroids have all been reported as potential contributors.[19] A systematic review of sleep disorders in cancer patients concluded that the prevalence of particular types of sleep disorders in cancer patients is difficult to assess, this is likely due to the primary focus on studying symptoms of poor sleep and not characterizing the underlying sleep disorders in cancer patients and survivors.[20] Thus, identification of the causative factor (s) behind sleep disturbances is crucial to treat insomnia. Psychological interventions, particularly cognitive behavioral therapy, have been of clinical benefit to insomnia patients in randomized clinical trials.[21] However, access to these psychological therapies is currently limited in our region. Yoga has shown improvement in insomnia symptoms among patients with cancer.[22] Acupuncture can also effectively reduce malignant-related depression, improve sleep quality, and help to improve the quality of life of cancer patients.[2324]
CONCLUSIONS
We have shown that patients with non-metastatic breast cancer experience an increase in insomnia and sleep disturbances during the treatment phase. Physicians should be aware of the need to routinely screen for sleep disturbance in breast cancer patients undergoing chemotherapy, with the purpose of minimizing the disease burden on the patients as early as possible. Further studies are required to develop novel strategies for prevention and treatment of insomnia amongst breast cancer patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [Google Scholar]
- Cancer treatments and their side effects are associated with aggravation of insomnia: Results of a longitudinal study. Cancer. 2015;121:1703-11.
- [Google Scholar]
- Insomnia in the Context of Cancer: A Review of a Neglected Problem. J Clin Oncol. 2001;19:895-908.
- [Google Scholar]
- Sleep disturbances in cancer patients: Underrecognized and undertreated. Cleve Clin J Med. 2013;80:722-32.
- [Google Scholar]
- The taboo of cancer: The experiences of cancer disclosure by Iranian patients, their family members and physicians. Psychooncology. 2013;22:396-402.
- [Google Scholar]
- Breast cancer in low-and middle-income countries: An emerging and challenging epidemic. J Oncol 2010 2010
- [Google Scholar]
- Trends in epidemiology and management of breast cancer in developing Arab countries: A literature and registry analysis. Int J Surg. 2007;5:225-33.
- [Google Scholar]
- Quality of life of Bahraini women with breast cancer: A cross sectional study. BMC Cancer. 2013;13:212.
- [Google Scholar]
- Quality of life and psychological well-being of breast cancer survivors in Jordan. Asian Pac J Cancer Prev. 2014;15:5927-36.
- [Google Scholar]
- Physical symptom profile for adult cancer inpatients at a Lebanese cancer unit. Eur J Intern Med. 2012;23:e185-9.
- [Google Scholar]
- Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155-73.
- [Google Scholar]
- Translating the Pittsburgh Sleep Quality Index into Arabic. West J Nurs Res. 2010;32:250-68.
- [Google Scholar]
- Impact of breast cancer treatments on sleep disturbances - A systematic review. Breast (Edinburgh, Scotland) . 2014;23:697-709.
- [Google Scholar]
- Trajectories of sleep disturbance and daytime sleepiness in women before and after surgery for breast cancer. J Pain Symptom Manage. 2013;45:244-60.
- [Google Scholar]
- Inflammation and behavioral symptoms after breast cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517-22.
- [Google Scholar]
- Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med. 2008;4:441-9.
- [Google Scholar]
- The relative importance of specific risk factors for insomnia in women treated for early-stage breast cancer. Psycho-oncology. 2008;17:9-18.
- [Google Scholar]
- Longitudinal prospective assessment of sleep quality: Before, during, and after adjuvant chemotherapy for breast cancer. Support Care Cancer. 2013;21:959-67.
- [Google Scholar]
- Insomnia in Cancer-Associations and Implications. Asian Pacific journal of cancer prevention: APJCP. 2015;16:6711-4.
- [Google Scholar]
- Systematic review of sleep disorders in cancer patients: Can the prevalence of sleep disorders be ascertained? Cancer Med. 2015;4:183-200.
- [Google Scholar]
- Sleep disturbance in adults with cancer: A systematic review of evidence for best practices in assessment and management for clinical practice. Ann Oncol. 2014;25:791-800.
- [Google Scholar]
- Yoga for the Treatment of Insomnia among Cancer Patients: Evidence, Mechanisms of Action, and Clinical Recommendations. Oncol Hematol Rev. 2014;10:164-8.
- [Google Scholar]
- Acupuncture for Managing Cancer-Related Insomnia: A Systematic Review of Randomized Clinical Trials. Integr Cancer Ther. 2017;16:135-46.
- [Google Scholar]
- Clinical research of acupuncture on malignant tumor patients for improving depression and sleep quality. J Tradit Chin Med. 2011;31:199-202.
- [Google Scholar]






