Translate this page into:
Comparison of Two Intervention Strategies on Prevention of Bedsores among the Bedridden Patients: A Quasi Experimental Community-based Trial
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
More than 80% of bedridden patients develop bedsores in home care settings. Training of informal caregivers can significantly affect the quality of care to these patients.
Objective:
The objective of this study is to compare the effectiveness of two caregiver training strategies on prevention of bedsores among bedridden patients.
Methods:
The study was carried out in Chandigarh. The study center was at PGIMER, Chandigarh. Seventy-eight bedridden patients being taken care in their homes were identified. These were randomly allocated into two groups. Group A received Prevention Package I, i.e., self-instruction Manual (SIM), training, and counseling. Group B received Prevention Package 2, i.e., only SIM. All these patients were followed up periodically for 1 year. During each follow-up, patients were observed for bedsore development. Braden scale was used to assess the risk factors of bedsores. Katz scale was used to evaluate the level of functional dependence of patients. Descriptive statistics was used to analyze the data.
Results:
The percentage reduction of number of patients at risk of bedsore development as per various domains of Braden Scale was more in Group A as compared to Group B on each successive visit. There was 100% improvement in mobility level in the patients who were totally dependent in both the groups. However, in moderately dependant patients, the improvement in mobility level was more (87%) in Group A as compared to Group B (75%). All the caregivers complied fully with instructions postintervention.
Conclusion:
Training of caregivers for the prevention of bedsores among the bedridden patients was effective in improving the practices of the caregivers and also in reducing the risk factors of bedsores. One-to-one training with SIM distribution yielded better results than the use of only SIM.
Keywords
Bedridden patients
bedsores
caregivers
home care
training
INTRODUCTION
The elderly population in India is increasing as the average life expectancy has improved beyond 65 years. By 2026, the number of elderly people would raise to 173 million.[1] As the age advances, there is decline in physical functions. The person becomes susceptible to various health problems. Many remain bedridden in the last years of their lives. Apart from this, many young people also become bedridden due to various problems such as posttraumatic paralysis.
Bedsores are the most prevalent wound among the bedridden patients. These are caused by unrelieved pressure over the bony prominences.[2] More than 80% of the bedridden patients ever develop bedsores.[3] The incidence varies from 0.4% to 38% in hospitals and 2.2%–23% in long-term care settings.[4] Bedsores are one of the most costly and physically debilitating complications.[56]
Because of the scarcity of hospital beds, many bedridden patients are provided care by the family caregivers in their home care settings. Although the disabled enjoy a better quality of life when they are cared for at home, however, the quality of care provided by the informal caregivers is questionable. They are usually untrained and unprepared to new roles and responsibilities and lack basic knowledge about care provision. Hence, they are constantly challenged to solve problems and make decisions as per the needs of the patients.
The extent of the problem can be minimized if the family caregivers are trained on simple measures to prevent and manage bedsores. Pressure-induced injuries start developing within 1–2 h of pressure exposure. Repositioning the patient every 2 h and making use of various comfort devices such as pillows, hand rolls, cotton rings, the alternating air mattresses, etc., have been shown to reduce the development of bedsores. Majority of the studies regarding the prevention of bedsores have been carried out in hospital settings.[7891011121314]
No study is available on the efficacy and impact of home-based care of bedridden cases on the incidence and natural history of bedsores in India. Against this background, the present study was conducted to see how the training of the caregivers on home-based care of bedridden cases affects the prevention of bedsores.
METHODS
The study was carried out in a north Indian city. The study center was a tertiary care hospital. The patients within its 30 km radius were included in this study.
Subjects
A bedridden patient was defined as a patient above 12 years of age who had been confined to bed for 15 days or more, for 90% of the time during the day and who was unable to get out of the bed without assistance or change position in bed at its own. The person in the family who is primarily responsible for the care of the bedridden patient was considered as the caregiver.
Sample size
The calculated sample size as per α = 0.05; β = 0.20; P = 0.80 was thirty patients in each group. Taking into consideration the drop outs, it was planned to enroll fifty patients in each group. However, we could include 39 patients in each group.
Study instruments
Apart from documenting the sociodemographic profile of the patients, the following instruments were used in the study.
Katz index of Independence in activities of daily living
It was used to evaluate the level of functional dependence of patients in their various activities of daily life, namely, bathing, dressing, going to the toilet, transferring, continence, and feeding. It is a six-point scale. For each domain, score zero indicates complete dependence, and score one depicts independence for that particular domain. The score between one and five categorized the patients as moderately dependent.[15]
Braden scale of proneness to bedsore development
It was used to assess the risk factors for the formation of bedsores among the bedridden patients. It involves the assessment of the patient on six parameters, i.e., "sensory perception," "moisture," "activity," "mobility," "nutrition," and "friction and shear." The maximum score is 23, and the minimum score is 6. The patient is considered to be "at risk" of developing bedsore if the score is between15 and 18, at "moderate risk" if the score is 13–14, at "high risk" if the score is 10–12 and at "very high risk" if the score is 9 or less.[16]
Self-instructional manual on prevention of bedsore
A self-instructional manual (SIM) in two languages (English and Hindi) containing the information regarding the prevention of bedsore was developed after reviewing the appropriate literature. It included the information regarding the definition of bedsore, how it develops, the common sites of bedsores, early warning signs of development of bedsores, the stages of bedsore, the risk factors facilitating the development of bedsores, proper positioning and repositioning techniques, skin care, preventing friction injury, preventing contractures, information regarding diet, and taking care of the wheel chair bound patient, the hemiplegic or paraplegic or quadriplegic patient. This manual was distributed to the respondent for self-reading.
Enrollment of the patients
The various sources tapped to enroll the patients included media (press conferences, newspaper coverage), Govt. hospitals, and the private hospitals. A face book page on the website of the institute was developed. Posters showing the information regarding the project were displayed in various hospitals of the city. Snow ball technique was also adopted.
Intervention
All the cases in stage 0 and 1, i.e., with no bedsores but were at the risk of developing bedsore ware included in the trial. A total of 78 patients were enrolled in the study as per the inclusion criteria discussed previously under the heading subjects. These were randomly allocated by a faculty into two groups. Following this, the prevention plan was discussed with the caregivers and implemented. The patients included in Group A received Prevention Package I (PP1), i.e., SIM, training, and counseling. The various components involved in training included positioning the patient, changing the posture of the patient, changing the bed sheet and clothes of the patient, feeding the patient, etc. The caregivers were counseled and encouraged regarding the need of regular care of the patient. The patients included in Group B received Prevention Package 2 (PP2), i.e., only the SIM.
The caregivers were advised to change the bed sheet of the patient daily, to perform the range of motion active and passive exercises at least twice in a day, and to change the position of the patient every two to three hourly.
Follow-up
All the patients and the caregivers were informed regarding the frequency of follow-up visits at the time of enrollments. The follow-up was weekly for 1 month, fortnightly for 3 months, monthly for 6 months, and after every 2 months for 1 year. During each follow-up visit, the patients were observed for bedsore development. The details were noted on the pro forma. The practices of the caregivers were observed. Each patient thus had 22 follow-up visits. Retraining was also done as per the need during follow-up in Group A. A field worker, and a Junior Research Fellow were involved in the follow-up activity. Before starting data collection, everyone was trained regarding various aspects of intervention and the use of scales as well.
Ethical aspects
Clearance was obtained from the ethics committee of the institute. Written informed consent was sought from the patients/caregivers. They were assured regarding the confidentiality of the data.
Trial registration
The trial was registered with trial registry of the Indian Council of Medical research.(CTRI/2011/09/002002).
Statistical analysis
SPSS version 21 (Armonk, New York) was used for statistical analysis. Descriptive statistics (mean, standard deviation, and percentage) was used to analyze the data.
RESULTS
Follow-up status of the patients
Out of 78 patients, 28% patients became mobile in Group A, and 33% of the cases turned mobile in Prevention package B, 13% expired in each group. More number of patients (13%) got migrated in Group B. At the end of follow-up, 13% were moderately dependent in Group A, and 26% were in Group B. In Group A, 4 (10%), two patients each at 11th and 17th follow visits and in Group B, only 1 (3%) patient at 11th visit developed Grade 1 bedsore. None of the patients in any of the group had bedsore at the last follow-up visit.
The details regarding the status of the patient at each follow-up visit shown in Figure 1.
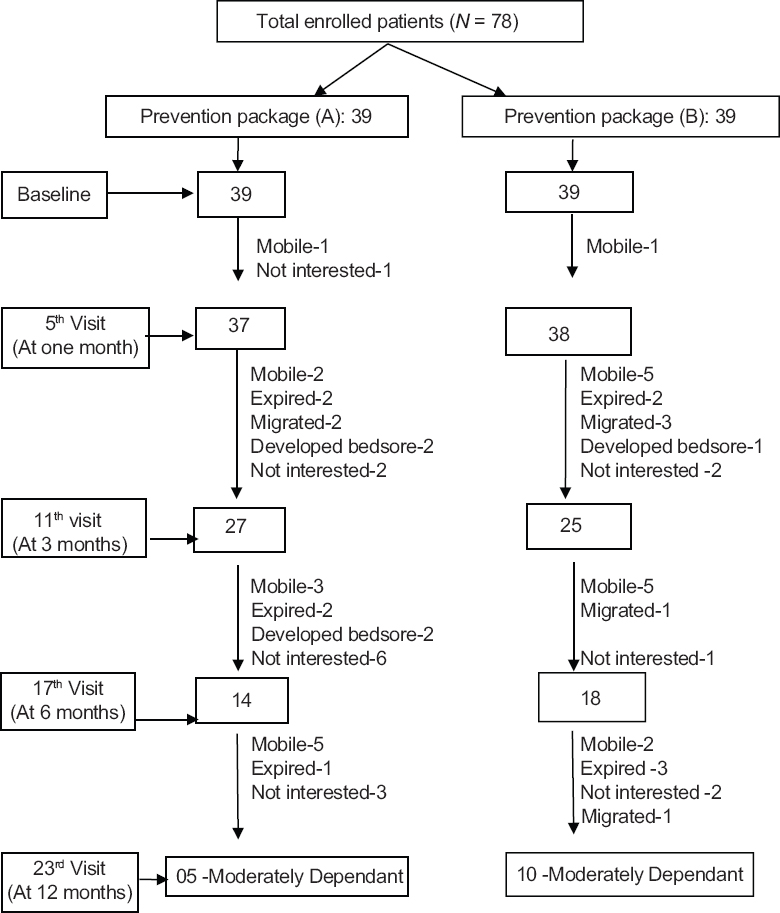
- Regarding the status of the patient at each follow. Group A: Self-Instruction Manual (SIM), Training and Counseling; Group B: Self-Instruction Manual only
Sociodemographic profile of the patients
Mean age of the subjects was 51.7 ± 21.7 with the range of 19–95 in Group A. It was 54.2 ± 24.4 with the range of 13–97 in Group B. There were more male patients in both the groups. As per educational status around one-third were graduates. Majority in both the groups were not working [Table 1].

Risk of developing bedsore as per Braden scale score among the patients
The patients were categorized as having high and low risk of developing bedsores as per the Braden score of ≤9 and ≥10, respectively. As per the domains on "sensory perception," "moisture," and "nutrition," there were very few patients in both the groups at very high risk of development of bedsore with Braden score of < 9. However, as per the other domains, "activity," "mobility" and "friction and sheer" more patients were at risk of developing bedsore with Braden scale score of < 9. However, as summarized in Table 2, the percentage reduction of number of patients in all these domains was more in Group A as compared to Group B on each successive visit. Even at the last follow-up visit, none of the patients had Braden score of < 9 as per the domains on "activity" and "mobility" in Group A, however, there were 40% and 10% patients, respectively, in both these domains with score < 9 in Group B.

Independence in activities of daily living as per Katz scale score
Table 3 shows the distribution of the patients as per their activity at each successive visit in various domains of Katz index. At the baseline, majority of the patients in both the groups were completely dependent in all the domains, i.e., bathing, dressing, toileting, transferring, and continence with zero score in all the domains except feeding. At the last follow-up visit, in Group A, more number of patients became completely independent though for transfer, continence, and feeding, there were patients in Group B who became completely independent.

Domains of Katz index among the patients
Table 4 shows the dependency level of the patients between the first and last follow-up visit. There was 100% improvement in mobility level the patients who were totally dependent in both the groups. In moderately dependent patients, the improvement in mobility level was in 87% of the subjects in Group A and it was 75% in Group B.

Compliance with preventive measures of bedsores
The caregivers complied fully with the instructions regarding the proper positioning of patients with bedsores, providing active and passive exercises, regular inspection of bony prominences, and gently massaging at the bony prominences post intervention. There was increase in the percentage of caregivers complying with the instructions at each follow-up.
DISCUSSION
Development of bedsores is considered as one of the most common problems among the bedridden patients. Once developed, these could be difficult to treat. They often result in pain, disfigurement, prolonged hospitalization, and additional costs. In such patients, mortality is considerably high due to complications if these are not managed timely and effectively. Hence, prevention of bedsores is always better than treating the complications associated with it. Prevention is a key intervention that is neither novel nor expensive. However, it is still ignored in the most clinical settings as evidenced by approximately 10% incidence of bedsore reported in bedridden patients admitted in top ranking hospital.[1014] Basic nursing care has a definite potential to save the thousands of patients and the caregivers from unnecessary harm.
In Indian settings, the majority of the stable bedridden patients are managed in the homes only. Hence, the informal caregivers have an important role to play in the care provision to such type of patients. It increases the responsibility of the family caregivers. They have to spend a significant amount of time in providing care and interacting with their patients. A wide range of activities is to be undertaken by them. An analysis of knowledge, attitude, and perception of the caregivers regarding care of bedridden patients in the home care settings will help in devising strategies to improve the care of such patients. There is very little research on this issue. One important concern is lack of training of caregivers on proper care practices for bedridden patients. Although they provide extraordinary uncompensated care to the bedridden, they often feel untrained and unprepared to carry out the task of care giving.[17] As such, hardly, there is any caregiver training programs to train the caregivers. Thus, a need was felt to prepare an educational intervention package to enhance the knowledge and skills of the caregivers regarding proper care provision for prevention and management of bedsores.
Assessment of risk factors among the bedridden patients is one of the important strategies to prevent the development of bedsores. If the patients are assessed for the risk of development of bedsore, its incidence can be reduced.[18] In the current study, Braden scale was used to assess the risk factors of bedsores among the patients. The patients were categorized as having high risk of developing bedsores and low risk of developing bedsores as per the Braden score of ≤9 and ≥ 10, respectively. The high-risk patients turned independent (mobile) in their activities of daily living (ADL) postintervention and reduced in number from baseline to the end line visit. Although the intervention was training of the caregivers regarding prevention of bedsores, the purpose of using Braden scale was to objectively assess the risk factors of development of bedsores among the bedridden patients included in the study.
In moderately dependent patients, the improvement in mobility level was in more number of patients in Group A than Group B, i.e., 87% versus 75%, respectively. However, at 11th follow-up visit of the patients in Group A, it was observed that more number of patients had "impaired" mobility with Braden Score < 9. That could have been the probable reason for more number of the patients in Group A who developed Grade I bedsore as compared to Group B. At the last follow-up visit, none of the patients in either group had bedsore.
Position change in the bedridden patients is recommended after 2–3 h.[19] In fact, the prolonged pressure on an area for more than 2–3 h causes disturbances in the nerve impulses and causes decreases in blood supply. It diminishes the nutrition to that particular part which leads to necrosis and ulcerations. The caregivers in the current study were trained in all the domains such as providing active and passive exercises, proper positioning of the patients, regular inspection of the bony prominences, providing high protein diet, and gently massaging over the bony prominences. They complied fully with all these instructions postintervention. The results are supported by similar other type of studies carried out in other countries.
A randomized controlled trial (RCT) was carried out by Moya and Morisonto see the effectiveness of home-based educational program in reducing the incidence of pressure ulcers in adults with progressive neurological conditions. The sample constituted 100 caregivers of these clients. There was a reduction in the incidence of pressure ulcer from 7% before educational program to 5% posteducation.[20] Another study was carried out by Eljedi et al. to determine the effectiveness of an educational program on a family caregiver's prevention and management of pressure ulcers of bedridden patients after discharge from hospital. The study revealed effectiveness of this educational-training program in managing and preventing pressure ulcers for bedridden patients by caregivers at their homes. It was recommended that application of this preventive program should be extended to cover all the rehabilitative and governmental hospitals of the region to reduce the burden of pressure ulcers on the families and the health-care system.[21]
Alhosis et al. have also emphasized that the implementation of the educational program for caregivers showed a remarkable increase and improvements of the caregivers’ knowledge regarding preventive measures of pressure ulcers. The various preventive measures were skin care, positions, nutrition, and exercises.[22] Farrell and Dempsey[23] point toward that written prevention protocols for education of patients, family, and health-care personnel are crucial to reduce or eliminate factors contributing to the development of pressure ulcer. The study of Wilson and Williams.[24] approved the benefit of the patients’ educational materials such as pamphlets and brochures to teach patients about the prevention and care of skin and pressure ulcers in urban hospitals, home care agencies, and public clinics in the Midwest in the United Kingdom. Bours et al.[25] recommended the use of guidelines for prevention and treatment of pressure ulcers as importance of changing position every 2 h, well-balanced nutrition, use of support surfaces, and effective implementation of these guides to prevent pressure ulcers. Tetterton et al.[26] evaluated the effectiveness of delivering high-quality, easily accessible geriatric education, and training program for direct care providers and other practitioners to prevent and treat pressure ulcers. Evaluation of the program revealed a significant reduction in the incidence of pressure ulcers from 1996 to 2000. Another RCT has shown that the use of alternating-air mattress or a water bed lowers the incidence of pressure ulcers by more than half among the hospitalized patients.[27]
Both the interventions in the current study were effective in improving the ADL of the patients. Before intervention, the majority of the patients had limitation specifically in activities such as bathing, toileting, and transferring in both the groups. In our study, comparatively more number of patients became independent in Group A, the caregivers of whom were given the personal training along with self-care manual. Hands on training usually have a better and a long-lasting effect. The dependency level of the patients in Group B also improved as the caregivers of these patients too was given the self-care manual, and the regular follow-ups might also have its own contribution in improving the health status of the patients. This indicates the need for training of caregivers for homecare of bedridden patients.
Our results signify that two types of efforts are needed for the training of caregivers, i.e., preparation of SIM, and one-to-one training. Here, package A is more labor intense as it involved one-to-one training and counseling in addition of distribution of SIM. Package B involving the distribution of SIM only was also reasonably effective. Hence, health-care administrators may decide as per the resources available to adopt a particular type of strategy.
It is recommended that various educational interventions regarding care of bedridden patients should be planned and implemented in the hospital itself to be taught to all the caregivers of bedridden patients to minimize the incidence of bedsores in the home care settings.
The current study has a limitation that there was no control group with the routine care. It is further recommended that three group designs may be taken up in the future research.
Financial support and sponsorship
Indian Council of Medical Research, New Delhi.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- National Institute of Social Defence. Ministry of Social Justice and Empowerment Government of India; January 2008:1.
- Pattern of quality of life of long term care for the bedridden patients in Chandigarh, North India. Int J Geriatrics Geronotol. 2005;2:1-14.
- [Google Scholar]
- Incidence, prevention and treatment of pressure ulcers in intensive care patients: A longitudinal study. Int J Nurs Stud. 2009;46:413-21.
- [Google Scholar]
- Heel ulcers in critical care units: A major pressure problem. Crit Care Nurs Q. 2002;25:41-53.
- [Google Scholar]
- Home–Based Long-Term Care. Technical Report Series No. 898. Geneva: World Health Organization; 2000.
- The effect of various combinations of turning and pressure reducing devices on the incidence of pressure ulcers. Int J Nurs Stud. 2005;42:37-46.
- [Google Scholar]
- Point prevalence of bedsore among the admitted patients in a tertiary care hospital. J Acad Hosp Adm. 2012;23:18-24.
- [Google Scholar]
- Impact of structured educational interventions on prevention of pressure ulcers in bedridden orthopedic patients – A randomized controlled trial. Eur Wound Manag Assoc J. 2013;13:40.
- [Google Scholar]
- Effect of comfort measures and repositioning on prevention of pressure ulcers in bedridden children. Nurs Midwifery Res J. 2013;9:99-107.
- [Google Scholar]
- Does an educational program for patient bystanders reduce the incidence and complications of bedsores in the medical emergency?: A quasi experimental study. J Adv Res Nurs Sci. 2014;1:1-6.
- [Google Scholar]
- Incidence of bedsore among the admitted patients in a tertiary care hospital. PGMER. 2015;49:26-31.
- [Google Scholar]
- Effect of caregiver perception of preparedness on burden in an oncology population. Oncol Nurs Forum. 2002;29:E70-6.
- [Google Scholar]
- Impact of staff education on pressure sore development in elderly hospitalized patients. Arch Intern Med. 1988;148:2241-3.
- [Google Scholar]
- The Prevention and Treatment of Pressure Ulcers. Edinburgh, UK: Mosby Company; 2001.
- Effect of an educational program on a family caregiver's prevention and management of pressure ulcers in bedridden patients after discharge from hospitals in Palestine. Int J Med Sci Public Health. 2015;4:600-6.
- [Google Scholar]
- Effect of designed pressure ulcer prevention program on caregivers’ knowledge of immobilized patients. J Am Sci. 2012;8:939-48.
- [Google Scholar]
- Smeltzer and Bare's Textbook of Medical-Surgical Nursing (2nd ed). Sidney: Wolters Kluwer/Lippincott Williams Wilkins; 2011.
- Assessing the readability of skin care and pressure ulcer patient education materials. J Wound Ostomy Continence Nurs. 2003;30:224-30.
- [Google Scholar]
- Prevalence, prevention, and treatment of pressure ulcers: Descriptive study in 89 institutions in the Netherlands. Res Nurs Health. 2002;25:99-110.
- [Google Scholar]
- The development of an educational collaborative to address comprehensive pressure ulcer prevention and treatment. Gerontol Geriatr Educ. 2004;24:53-65.
- [Google Scholar]
- Decubitus prophylaxis: A prospective trial on the efficiency of alternating-pressure air-mattresses and water-mattresses. Acta Derm Venereol. 1983;63:227-30.
- [Google Scholar]






