Translate this page into:
Patients with End-stage Oncologic and Nononcologic Disease in Emergency Service of an Urban Tertiary Hospital
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
In the last decades, patients with chronic terminal diseases have had more frequent visits to emergency services.
Aims:
This study aims to determine the proportion of terminal illness in patients readmitted to emergency room, to evaluate the use of this service and rate of death.
Settings and Design:
A cross-sectional study in a tertiary hospital with 120 stretchers which annually reports 160 thousand attentions and 22 thousand admissions.
Subjects and Methods:
Included 18-year-old patients or older who were readmitted to emergency room. Patient and/or caregiver were interviewed; medical record was reviewed and made 1-year follow-up. Terminal cancer was determined by histologically confirmation in Stage IV and nononcologic terminal disease by total functional dependence (Katz index) or severe cognitive impairment (Pfeiffer questionnaire) in addition of advanced organ failure.
Statistical Analysis Used:
Fisher's exact and U of Mann–Whitney tests for two independent samples.
Results:
Ninety-two (26%) of 349 were readmissions; 29 (36.7%) of 79 evaluated patients were identifying with terminal disease. Eleven (38%) of them had cancer (genitourinary in 64%). Nononcologic terminal disease was identified in 18 cases (62%) (Neurodegenerative involvement in 50%). More frequent symptoms were dyspnea 41%, mental confusion 24%, and pain 21%. Terminal patients had 6.2 (standard deviation 8.2) emergency visits at last year, being admitted 48,6% of these visits. Six-month mortality rate was 73 and 61% in oncologic and nononcolgic patients, respectively (P < 0.05).
Conclusions:
End-stage disease is frequent in readmitted patients to emergency, more of nononcologic kind. These patients use frequently emergency service, with high mortality (more elevated in oncologic).
Keywords
Emergency service
palliative care
terminally ill
INTRODUCTION
Epidemiological transition and technological advancement not only have increased life expectancy but also increases the frequency and coexistence of complex chronic diseases (oncological and nononcologic). In the last decades, criteria for terminal stage of these diseases have been clearly defined, where the best curative treatments that exist, are not effective and even increase the suffering of the patient. Proposing mechanisms of early detection and use of palliative care to improve the quality of life of the patient and his family, with savings of scarce and expensive resources.[12345678]
In North America, Europe, and Oceania, there are reports that show effective interventions in this group of patients, decreasing hospital stay, and admissions, including the detection and early application of palliative care from the emergency service. Oncological diseases have been better studied and present higher mortality; however, nononcological diseases are more frequent and have greater survival, with the same needs as oncological ones.[591011]
There is an increase number of patients with advanced chronic diseases who attend to emergency services, producing bed saturation, prolonged hospital stay, even in intensive care rooms and high rates of in-hospital death, often in inadequate conditions. However, there are no adequate reports worldwide.[2101112131415]
In Latin America, there is a few data on this subject and a lack of knowledge about palliative care, with worse situation in urban tertiary hospitals, coupled with problems at the primary health care. In Peru, the situation is similar, and the main social security hospitals are almost collapsed due to patient overload, many of them with terminal illnesses.[1314] We set as objectives: To determine the proportion of terminal illness in patients readmitted to emergency room, to evaluate the use frequency of this service and the rate of death in terminal patients.
SUBJECTS AND METHODS
A cross-sectional study took place between May 15 and 21 of 2016. Included 18-year-old patients or older who were readmitted to the emergency room of a tertiary hospital; psychiatry and obstetrics patients were excluded. Readmission was considered as to two or more admissions in the last year. This social security hospital had 1500 beds and 93 medical specialties, its adult emergency service had 120 stretchers and annually reports 160 thousand attentions and 22 thousand admissions. Patient and/or caregiver were interviewed; medical history was reviewed and made followed up by 1 year. For cancer was considered histologically confirmation, stage IV and multiple brain, lung, or liver metastases. Was considered as a nononcologic end stage disease: Total functional dependence (Katz index) or severe cognitive impairment (Pfeiffer questionnaire) in addition of advanced neurological disease, glomerular filtration rate < 30%, Child-Pugh Stage C liver cirrhosis, permanent home oxygen therapy or Left ventricular ejection fraction < 20%. To determinate significant difference for patients with terminal illness in the oncological and nononcological group were used Fisher exact test and U of Mann-Whitney test by two independent samples, considering a significant P < 0.05. Statistical program SPSS 21.00 (IBM, SPSS Stat 21) was used.
RESULTS
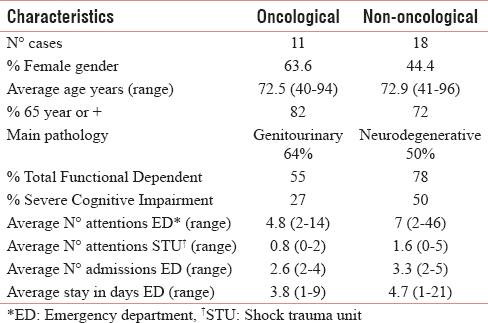
Of 349 admissions in the study week, 92 (26%) were readmissions. It was not possible to evaluate 13 cases (seven lost, four incomplete, one deceased, and one readmitted). Seventy-nine patients entered the study, 29 (36, 7%) were identifying with terminal disease. Eleven (38%) of them had cancer (breast two, prostate two, kidney two, endometrium one, hepatic one, pancreas one, lung one, and lymphoma one). Nononcologic terminal disease was identified in 18 cases (62%) (Stroke disability four, dementia three, renal failure three, liver cirrhosis two, pulmonary fibrosis two, heart failure one, sequelae of traumatic brain injury one, sequelae of meningitis one, and myelodysplasia one). Reasons for admission were encephalopathy 28%, respiratory failure 21%, and sepsis 14% (P > 0.05 for oncological and nononcological groups); more frequent symptoms were dyspnea 41%, mental confusion 24%, and pain 21%. Terminal patients had an average of 6.2 (standard deviation 8.2) emergency visits in the last year (range 2–46), being admitted 48.6% of these visits (P > 0.05 for oncological and nononcological groups). Table 1 presents characteristics according to oncological and nononcological groups, not finding significant differences (P > 0.05) and Figure 1 shows the mortality rate, with P < 0.05.
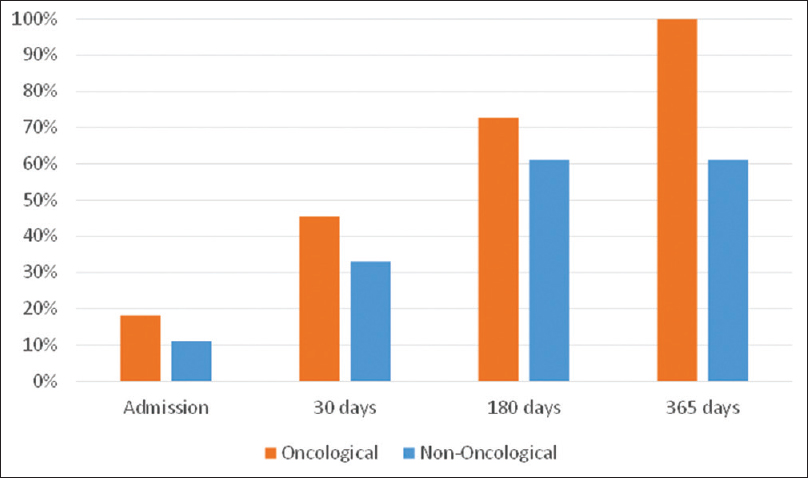
- The rate mortality at 1-year follow-up of patients
DISCUSSION
The readmission rate was similar to 2012 for the same service.[13] More than 35% of patients readmitted to emergency suffer from the end-stage disease, similar to reports from Europe and North America; where there are better-structured health systems. The patients had inadequate control of symptoms, dyspnea predominated instead of pain, different from that reported in other countries. Age was similar in both groups, with female gender predominance in oncological and male gender in nononcological. Unlike reports from Europe and North America, genitourinary cancer 64% was the most frequent, with low frequency of lung cancer.[491016]
Similar to international reports, chronic nononcologic illnesses were common, with frequent neurodegenerative involvement (50%) but a low frequency of cardiopulmonary disease compared to Glajchen et al. The varied pathology of this group makes identification and prognosis difficult, but produces greater symptomatology, functional dependence and cognitive impairment.[11718]
It is evidenced that terminal ill patients frequently use the emergency service, for consultations, admissions and also the shock-trauma unit, with more frequency of nononcological group. There is an extended stay in emergency, more than 3 days on average, this being higher than international reports (where it is < 24 h). This is due to deficiencies in the health system, more at the primary level of care.[10]
The mortality of emergency terminal patients was high, dying often in inadequate conditions for the patient and the family. The cancer group has the highest mortality and the highest survival rate for noncancer patients is in agreement with the poor prediction reported. The lack of clear legislation for end-of-life situations (anticipated will or nonresuscitation order) and the poor training of health personnel on this issue contribute to prolonged agony and suffering. The application of multidisciplinary palliative care is necessary.[9101417]
The ethical conflict for cataloguing the patient as a terminal still persists, but its purpose is to provide better care and quality of life. Limiting factors are sample size, selection period, and establishment evaluated, and selection criteria in noncancer patients are also questionable. However, the study shows the existing reality, poorly studied in Latin America, and suggests further research, especially in advanced nononcologic disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A rapid two-stage screening protocol for palliative care in the emergency department: A quality improvement initiative. J Pain Symptom Manage. 2011;42:657-62.
- [Google Scholar]
- What is the incidence of patients with palliative care needs presenting to the emergency department? A critical review. Palliat Med. 2014;28:1197-205.
- [Google Scholar]
- Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17:1253-7.
- [Google Scholar]
- Palliative care screening and assessment in the emergency department: A Systematic review. J Pain Symptom Manage. 2016;51:108-900.
- [Google Scholar]
- What tools are available to identify patients with palliative care needs in primary care: A systematic literature review and survey of European practice. BMJ Support Palliat Care. 2013;3:444-51.
- [Google Scholar]
- Palliative care symptom assessment for patients with cancer in the emergency department: Validation of the screen for palliative and end-of-life care needs in the emergency department instrument. J Palliat Med. 2011;14:757-64.
- [Google Scholar]
- WHO. Global Atlas of Palliative Care at the End of Life. World Health Organization. 2014
- [Google Scholar]
- How common are palliative care needs among older people who die in the emergency department? Emerg Med J. 2011;28:491-5.
- [Google Scholar]
- Emergency department attendance by patients with cancer in their last month of life: A systematic review and meta-analysis. J Clin Oncol. 2015;33:370-6.
- [Google Scholar]
- Palliative care for patients who died in emergency departments: Analysis of a multicentre cross-sectional survey. Emerg Med J. 2012;29:795-7.
- [Google Scholar]
- Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage. 2010;39:972-81.
- [Google Scholar]
- Atlas de Cuidados Paliativos en Latinoamérica (1st ed). Houston: Press; 2012.
- Frequently patient readmission at the emergency service to adults of the terciarity hospital. Lima-Peru 2012. Rev Soc Peru Med Int. 2015;28:153-7.
- [Google Scholar]
- Characteristics of the last hospital stay in terminal patients at an acute care hospital in Colombia. Am J Hosp Palliat Care. 2010;27:402-6.
- [Google Scholar]
- Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidability. Am J Hosp Palliat Care. 2016;33:658-62.
- [Google Scholar]
- A hospice and palliative care bed dedicated to patients admitted to the emergency department for end-of-life care. Am J Hosp Palliat Care. 2016;33:403-6.
- [Google Scholar]
- Criterios de seleccion de pacientes con enfermedades no oncologicas en programas y/o servicios de cuidados paliativos. Med Paliativa. 2010;17:161-71.
- [Google Scholar]
- Initiating palliative care consults for advanced dementia patients in the emergency department. J Palliat Med. 2014;17:346-50.
- [Google Scholar]






