Translate this page into:
Profile of Patients Opting for Palliative Care in India
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Understanding the profile of end users is a key input for designing a service. Centers that provide full-scale palliative care are few and far between in our country, and there is a need to open more centers to extend the services to a larger percentage of patients.
Methods:
Patient data from the inception of the center till January 2016 have been stored in a database. The data were mined, exported to Excel, and analyzed.
Results:
The data of 11,258 patients revealed the profile of patients, including their age, gender distribution, marital status, symptomology, and outcome. The present paper describes the profile of patients opting for palliative care in our country.
Conclusions:
The profile of patients registered at this center validates certain assumptions while debunking others. It is hoped that this profile gives some guidance to those desirous of setting up palliative care services.
Keywords
Demographics
palliative care
patient profile
survival
symptoms
INTRODUCTION
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”[1]
This care is required by patients suffering from a variety of chronic diseases[2] but has been most commonly used for cancer patients. The concept of palliative care existed far back in the history but has seen a revival in the past 50 years.[3] In India, palliative care is still an emerging discipline and faces many challenges that need to be addressed.[4]
Earliest reports of cancer came from Egypt about 3500 years ago and the treatment then described was cautery and palliation.[5] With the advent of curative therapy, palliation was almost forgotten, till Dame Cicely Saunders brought it to the fore. The movement, which began with the setup of hospices for end-of-life care soon broadened to palliation from diagnosis to beyond bereavement for the family.[6] Since pain was the single debilitating symptom of advanced cancer, the use of effective analgesics became the mainstay of palliation, to which other modalities were subsequently added.[7]
India has a high load of cancer and it is rising[8] in 2015, the incidence of cancer in the country was estimated to be 1,148,691, which is likely to go up to 1,320,928 cases by the year 2020.[9] The overall growth rate works out to 14.9%, and the compound annual growth rate works out to 2.83%. It is estimated that the prevalence of cancer in the country currently is approximately 3.25 million. While the need of palliative care is high in India, its delivery will be guided by socioeconomic conditions in the country.[10] Proper development of this emerging discipline must be guided by evidence that is sadly lacking.[11] There are a large number of palliative care centers but they are distributed in a skewed fashion and 214 of the 380 centers are in a small state - Kerala, whereas a large state like Uttar Pradesh has only 4.[12] Many of the centers in Kerala are just single-room units, nonetheless almost all patients in the states are able to access palliative services.
One of the important factors guiding the set of any services is a thorough understanding of the user profile. This is lacking in India. Literature from India does not include any data on patients opting for palliative care in India; this is a major impediment to those planning to setup palliative services in the country. In the absence of such information, facilities are made available on an ad hoc basis, to be augmented or curtailed depending on need. This is one of the main problems for those desiring to set up a palliative care center.
The profile of Indian patients opting for palliative care reported here was built from data that have been stored over the past 20 years. The data are of patients registered at a full-service palliative care center that was set up in 1997. This is one of the few comprehensive palliative care centers in the country, offering inpatient, outpatient, and home care services. Untill January 1, 2016, the center had 11,258 registrations from patients. Data of all patients were initially noted on paper; in 2005, the data were transferred to a custom-made software. Data were extracted from this software and analyzed to build a profile of patients who opt for palliative care in India. This profile may help organizations and authorities to make provisions for more palliative care facilities in the country.
RESULTS
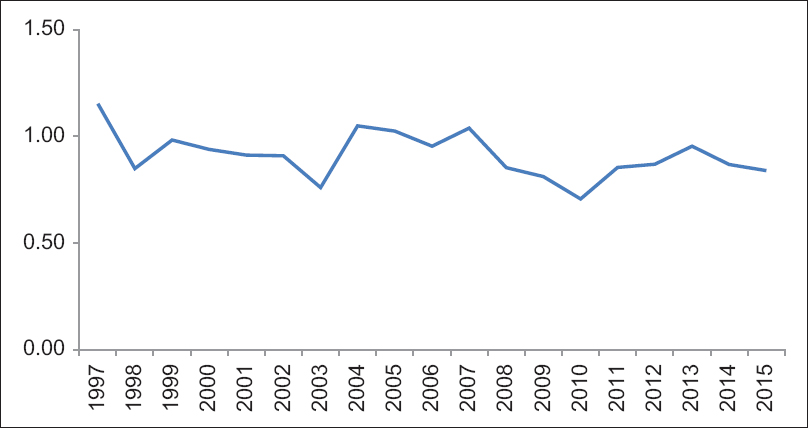
The annual registration of patients has grown steadily growing and reached a four-digit number in 2016. The registrations showed a dip between 2005 and 2010, but the phase appears to have passed and the numbers have risen again. A graphic representation of registrations is given in Figure 1.

- Annual registrations of patients at the center
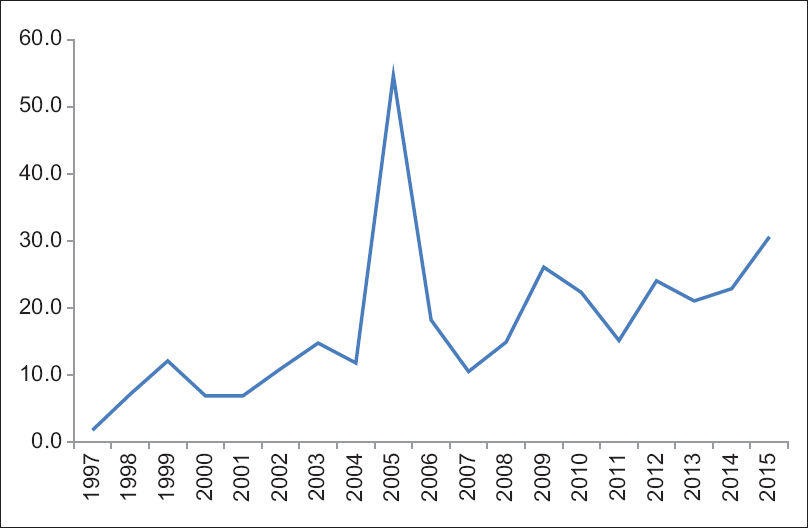
The gender-wise breakup was analyzed, and male-to-female ratio was calculated; this is presented in Figure 2. As can be seen, the ratio hovers around 1.0 in the past 10 years, but the ratio has been consistently below 1.0, suggesting that more women are registering for palliative care. The survival of patients by gender was also calculated and it was observed that the mean survival for females = 78.88 (standard deviation [SD] 16.3) days and for males = 74.38 (SD 17.9) days.
- Male-to-female ratio in registration
Patients at the center sometimes take discharge but may subsequently return to the center. Thus, there are new admissions and readmissions in the center. Figure 3 shows the distribution of patients in terms of this criterion. The data were analyzed for total number of patients discharged from the center. This is shown in Figure 4, there is a sudden rise in discharges from the center and a peaking of discharges in 2005. The rising number of discharges over the years may not mean much since the number of total admissions to the center is also on the rise, it was therefore considered essential to calculate the discharges as a percent of the admissions, which is shown in Figure 5.

- New admission and repeat admissions at the center

- Discharge of patients from the center
- Patients discharged as a percentage of total registrations
The data were sorted by the age of patients at registration; this is shown in Figure 6. Table 1 shows the distribution of patients on the basis of marital status. Figure 7 shows the presence or absence of metastases in the patients.

- Age-wise distribution of patients

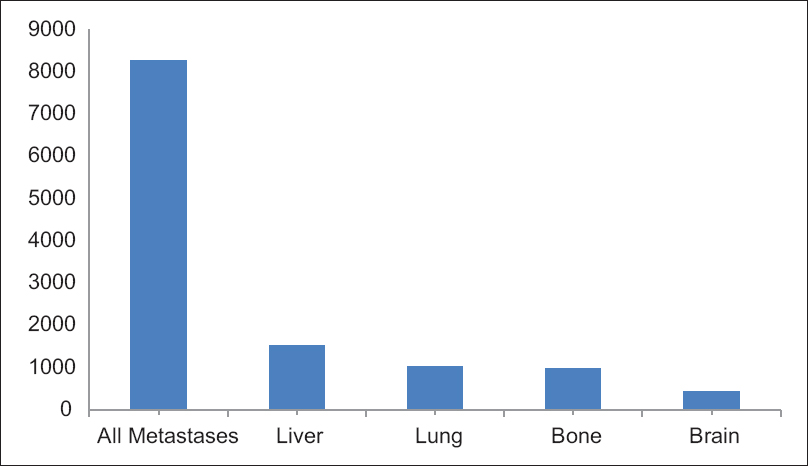
- Distribution of metastases in patients
An attempt was also made to analyze the data for survival of patients by the type of cancer diagnosed. The results are shown in Table 2.

Finally, the symptoms of the patients were studied. Most patients reported more than one symptoms, and hence, the number of patients reporting different symptoms exceed 11,258, whose symptoms were studied. Overall in the software, 22 different symptoms reported by patients were noted. Figure 8 shows the details of top ten symptoms.

- Problems/symptoms reported by patients
DISCUSSION
In the 18 years of functioning, 11,258 registrations took place at the center. Starting with only 114 in the first year, the figure for 2015 is 1023. It must be emphasized that this does not represent bed occupancy at the center since patients' stay at the center is variable and only depends on their need. The steady rise in registrations saw a dip between 2005 and 2010, but as stated the figures have risen subsequently. The dip in figures could be due to a variety of factors, change of guard, and staffing could be the main factors.
In 2015, the registrations at the center were at an all-time high. However, the total number of registrations was just 1023. This is against the prevalence of cancer in the city estimated to be about 15,000. The center has a capacity of 50 beds and the total number of beds in the city do not touch 100, thus even assuming that only half of the city's patients come to this center, not more than 15% of the patients in the city have access to palliative care. In this regard, the city of Pune is better than most cities in the country outside Kerala.
The need of palliative care in different countries, mainly European, has been estimated.[13] By this standard, the needs in India are very high. Considering the size of the Indian population and prevalence of cancer, it is clear that palliative services have a long way to go. Kerala has certainly set an example,[14] and the country should follow, not necessarily using the same model but at least emulating the spread.[15]
There has been a doubt in the minds of some of our staff that whether there exists a gender bias in patients opting for palliation. A bias has been demonstrated in resource allocation on the basis of gender and ethnic groups.[16] Given the known gender inequalities in the country, it is possible that women are diverted to palliation while men continue on curative therapy. Examination of the data does not seem to support this. In the past 10 years, there are consistently more women coming for palliation compared to men; the differences are too small to reflect a true gender bias. The reason for higher number of women coming to the center could be due to the fact that the incidence of cancer among women is higher than that in males in India. The ratio of cancers (male to female for all sites) for 2010, 2015, and 2020 (projected) is 0.89, 0.88, and 0.87, respectively.[17] Globocan 2012 also reported that the male-to-female ratio was 0.88 in 2012.[18]
There is no difference in the survival of female or male patients. This can be interpreted to mean that all patients are referred to or brought for palliative care at similar stage of the disease. Average survival of patients after reference to the center was low, suggesting that most patients came to the center only after all curative options had closed. Early introduction of palliative therapy has been demonstrated to improve the quality and quantity of life.[19] The advantage of early palliative care has been demonstrated to influence patient-related outcomes too.[20] However, this information does not seem to affect referral to palliative services in India.
There is a difference between a hospice and a palliative care center. While a hospice provides only end-of-life service, a palliative care center provides a larger spectrum of services from diagnosis to after the death of the patient. It is logical to expect that there would be very few, if any discharges from a hospice while they should be fairly common from a palliative care center. A center may label itself as a hospice or as a palliative care center, discharges from the center is a measure of how the society and patients perceive it.
When patients are admitted in a hospice they are toward the end of their lives, hence new admissions are high but readmissions are low. In the early years of the center, new admissions dominated over readmissions, suggesting that the center was viewed as a hospice. Subsequently, readmissions rose [Figure 3] suggesting a shift in perception about the center.
With time, the discharges from the center increased. There was an unexplained peak in 2005, the cause of which is not clear. It could be due to some right actions taken by the center staff or an unknown factor. Leaving aside this unexplained peak, the absolute number of discharges from the center is on the rise but so is the total number of registrations at the center. To correct the discharge figures for the rising registrations, discharges were calculated as a percentage of total registrations and have been shown in Figure 6. Not only the total discharges from the center show a steady rise but also discharges as a percentage of registrations show a similar trend.
On studying the distribution of patients' age wise, it is noted that most patients were from the 51 to 60 age group. Most patients belonged to the higher age group and not many pediatric cases or young adults register here. It is a known phenomenon that the incidence of cancer rises dramatically at higher age.[21]
The peak incidence of cancer in India is also in this age group.[22]
Marital status has been reported to affect the trajectory of a number of diseases[23] including cancer.[24] This database contains details of 11,258 patients of which the marital status of 5812 patients is recorded. The analysis of data on the basis of marital status is more complicated and is still in progress and will be reported later.
On hearing of a diagnosis of cancer, the first question anyone has is how much time does the patient have. This question can never be answered satisfactorily since measurement of time, requires two points of reference. In cancer, the second point of reference is death, but there are many options for the first. For analysis of survival, the date of admission to the center has been used as the first point. This was because in India almost 70% of the patients are diagnosed in an advanced stage, primarily being due to lack of awareness among the patients and poor diagnostic facilities being available. While going through the data, it was seen that in most cases the date of diagnosis was quite close to the date of admission.
Assuming that patients come to palliative care after all therapeutic options have closed, then one could calculate survival from that point of time. The data show that pancreatic cancer is the most aggressive followed by Ewing's Sarcoma and hepatocellular cancer. This compares well with known 5-year survival rates reported in the UK and US.[25] Analysis of the data for comparative survival in different cancers is presently underway and further details will be presented later.
Sir William Osler (1849–1919) said “listen to your patient, he is telling you the diagnosis.” Patients in fact tell much more than diagnosis. A careful study of patients can help in understanding disease trajectories, expected complications, and even survival rates. What is required is to study a sufficiently large number of patients as thoroughly as possible. One of the main difficulties in doing so is the availability of accurate records of patients, and here databases come to our rescue. Building up a database is a long and arduous work, which gives no return until it achieves a critical mass. It is only after this that it starts yielding results.
CONCLUSIONS
The study of the profile of patients is useful for planning palliative services, more so in our country. It gives an idea about the problems that may be anticipated and the trajectories of the disease. Hopefully, this will help in expanding the base of palliative care and improve existing services.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- Palliative care in India: Successes and limitations. J Pain Palliat Care Pharmacother. 2003;17:121-8.
- [Google Scholar]
- History of cancer, ancient and modern treatment methods. J Cancer Sci Ther. 2009;1:1-4.
- [Google Scholar]
- Integrating palliative care into the trajectory of cancer care. Nat Rev Clin Oncol. 2016;13:159-71.
- [Google Scholar]
- Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489-538.
- [Google Scholar]
- Central Bureau of Health Intelligence. Projected Cases of Cancer at India Level for Selected Times and Selected Time Periods. Available from: http://www.cbhidghs.nic.in/writereaddata/mainlinkFile/NHP-2015.pdf
- [Google Scholar]
- Palliative care tailored towards the needs of the poor in India. Indian J Surg Oncol. 2015;6:227-31.
- [Google Scholar]
- Palliative care in South Asia: A systematic review of the evidence for care models, interventions, and outcomes. BMC Res Notes. 2015;8:172.
- [Google Scholar]
- Pallium India. Directory of Palliative Care Services. Available from: http://www.palliumindia.org/resources/clinics/
- [Google Scholar]
- Estimating the need for palliative care at the population level: A cross-national study in 12 countries. Palliat Med. 2017;31:526-36.
- [Google Scholar]
- Palliative care in Kerala, India: A model for resource-poor settings. Onkologie. 2004;27:138-42.
- [Google Scholar]
- Models of delivering palliative and end-of-life care in India. Curr Opin Support Palliat Care. 2013;7:216-22.
- [Google Scholar]
- Non-pharmacological cancer pain interventions in populations with social disparities: A systematic review and meta-analysis. Support Care Cancer. 2016;24:985-1000.
- [Google Scholar]
- Projections of number of cancer cases in India (2010-2020) by Cancer Groups. Asian Pac J Cancer Prev. 2010;11:1045-9.
- [Google Scholar]
- International Agency for Research on Cancer. Globocan 2012, Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Available from: http://www.globocan.iarc.fr/Default.aspx
- [Google Scholar]
- Early palliative care for lung cancer: Improving quality of life and increasing survival. Int J Palliat Nurs. 2010;16:420-3.
- [Google Scholar]
- Integration of early specialist palliative care in cancer care and patient related outcomes: A critical review of evidence. Indian J Palliat Care. 2016;22:252-7.
- [Google Scholar]
- How ageing increases cancer susceptibility: A tale of two opposing yet synergistic views. Genes Dis. 2016;3:105-9.
- [Google Scholar]
- Major sites of cancer occurrence among men and women in Gandhinagar district, India. Indian J Community Med. 2015;40:56-61.
- [Google Scholar]
- Marital status and survival in patients with cancer. J Clin Oncol. 2013;31:3869-76.
- [Google Scholar]
- One, Five and Ten Year Survival for Common Cancers. Available from: http://www.cancerresearchuk.org/






