Translate this page into:
Estimation of Need for Palliative Care among Noncancer Patients Attending a Tertiary Care Hospital
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Palliative care services, until recently, were mainly restricted to cancer patients with incurable diseases. Hence, evaluative studies of palliative care are sparse in areas other than oncology.
Aims:
To estimate what proportion of patients attending the Departments of Neurology, Cardiology, and Nephrology of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, required palliative care and to identify the palliative care needs of those patients.
Settings and Design:
This was an exploratory descriptive study conducted in the three departments of JIPMER.
Materials and Method:
There was no predetermined sample size for the study. The participants were all adult inpatients and outpatients who were in need of palliative care in the departments of Cardiology, Nephrology, and Neurology on the day of study.
Statistical Analysis:
Percentage distribution was used to analyze the categorical variables such as education, gender, age, patients in need of palliative care, and their needs.
Results:
The study showed that one in ten non-cancer patients in tertiary care hospitals may require palliative care services. Apart from issues in physical domain, a substantial proportion of participants also had issues in the psychological, emotional, and financial domains.
Conclusion:
This study highlights the need for incorporation and initiation of palliative care services in other non-cancer specialties in tertiary care hospitals to ensure holistic management of such cases. Counseling service has also to be rendered as part of palliative care since a good share of the patients had psychological and emotional issues.
Keywords
Noncancer patients
palliative care
tertiary care hospital
INTRODUCTION
The need for palliative care is increasing at a rapid pace due to the world's aging population and increased incidence of cancer and other noncommunicable diseases. The highest proportion of adults in need of palliative care at the end of life is from low- and middle-income countries. Palliative care need of cancer patients is acknowledged worldwide. Recently, awareness regarding the need for palliative care for other chronic conditions such as Alzheimer's and other dementias, cardiac diseases (excluding sudden deaths), liver cirrhosis, chronic obstructive pulmonary disease, diabetes, HIV/AIDS, renal failure, multiple sclerosis, Parkinson's disease, rheumatoid arthritis, and drug-resistant tuberculosis has been increasing. Around 90% of the burden of end-of-life palliative care is constituted by those dying from noncommunicable diseases.[1]
Pioneering institutes and reputed organizations have tried to define palliative care. The most accepted and widely quoted definition is the World Health Organization (WHO) definition. WHO[2] defines palliative care “as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through prevention and relief of suffering by means of early identification, assessment, and treatment of pain, and other problems – physical, psychosocial, and spiritual.” The palliative care provides maximum quality of life to the patients and their families by alleviating pain and other symptoms, helping patients and their families cope with the emotional discomfort and practical issues, helping people deal with spiritual questions, and live as actively as possible and support family and friends in their bereavement. Palliative care initiated at the point of diagnosis continues throughout treatment and bereavement support will be offered to family after the patient's death.
Although palliative care is expanding in the developed world, in spite of myths and misunderstandings about its nature and purpose, it is only beginning to be available in the developing world where it has most needed. Many hurdles pose challenges to the development of palliative care. The development of palliative care has facilitated only by adopting a public health approach keeping in mind of such hurdles. Restrictions imposed on the procurement of essential medicines needed for palliative care, dearth of skilled palliative care providers, the absence of a federally run program for providing palliative care, and above all the absence of a clear policy have hindered the establishment of palliative care services.
An Expert Group of the Ministry of Health and Family Welfare constituted by the Government of India[3] to draft proposals for establishing palliative care services in India opined that, though the need of palliative care is increasing, the coverage of services in terms of availability, affordability, and accessibility is inadequate. It has been estimated that only 1% of patients who needs palliative care services receive it. Even though the WHO emphasizes that palliative care is an essential component of modern health-care system, it is available only in few tertiary care centers in India. There is an urgent need to introduce palliative care in primary, secondary, and tertiary health-care facilities. Palliative care services can be delivered in many different ways through hospitals as outpatient or inpatient basis or in the form of home-based care by primary and community teams. Certain studies clearly show that there is a constantly increasing need for including palliative care services in a hospital setting.[4567]
The wide variation in the prognosis of chronic diseases poses a challenge for identifying target population for palliative care delivery. The need for palliative care is increasing exponentially, but the palliative care service delivery has failed to keep pace. Palliative care has been heavily concentrated to the field of oncology and research evidences are from patients with cancer. Hitherto unexplored, understanding the need for palliative care in noncancer patients arriving at a tertiary care hospital will help in allocating scarce resources judiciously and assure every deserving patient of palliative care. It is imperative that the knowledge base in palliative care is enriched by information exchange between consultants in different specialties and a team approach to palliative care delivery should be initiated. It must be emphasized that palliative care which is quite often seen as an act of benevolence alone is the basic humanitarian right of any dying individual regardless of the cause of the plight he/she is in; be it cancer, AIDS, or any other chronic disease.
Palliative care services until recently were mainly restricted to cancer patients with incurable disease. It can be seen as end-of-life care for cancer patients and hence studies estimating the need for palliative care have mainly dealt with cancer patients. Evaluative studies of palliative care are sparse in areas other than oncology.
With this backlog, the present study aims to estimate what proportion of patients attending the Departments of Neurology, Cardiology, and Nephrology of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, require palliative care and to identify the palliative care needs of those patients.
MATERIALS AND METHODS
This study was designed as an exploratory descriptive one. The participants were all adult inpatients and outpatients who were in need of palliative care in the Departments of Cardiology, Nephrology, and Neurology on the day of study.
There was no predetermined sample size for the study. One day's outpatient department (OPD) attendance each and one day's inpatient admission each in the Departments of Cardiology, Nephrology, and Neurology constituted the study population.
Consent was obtained from the patients after informing them about the purpose of the study. Those data would be used only for research purposes and that confidentiality and anonymity of each patient would be maintained.
This study has been carried out on a single day in each of the inpatient and outpatient settings of the Departments of Neurology, Cardiology, and Nephrology. The Department of Preventive and Social Medicine, JIPMER, conducted a workshop on palliative care for orienting the health professionals in various departments of the hospital in rendering palliative care services. Following the conduct of workshop, with the help of doctors from Nephrology, Neurology, and Cardiology, the investigator identified patients requiring palliative care from among the outpatients attending and inpatients admitted in these departments from January 2015 to 2nd week of February 2015. The inpatients in the wards for a particular day alone were taken up for the study. After obtaining informed consent from the identified patients, their sociodemographic details and disease treatment details were collected using pretested patient questionnaire. To assess the needs of the patients requiring palliative care, the required information was collected through direct interview using the customized version of Need Assessment Tool for Progressive Disease (Waller et al., 2010).[8]
It is a multiple response type questionnaire. The need assessment questionnaire evaluates the following domains, namely, physical, psychological, financial, spiritual, concern with regard to medication and treatment, and issues in relationship with spouse. Physical domain was further evaluated by probing for the existence of nine cardinal symptoms including pain, breathlessness, sleeplessness, bowel and bladder dysfunction, loss of appetite, fatigue, nausea, edema, and cough.
EpiData software version 3.1 (Odense, Denmark) was used for data entry and analysis was done using IBM SPSS software version 22 (IBM). Percentage distribution was used to analyze the categorical variables such as education, gender, age, and patients in need of palliative care and their needs.
RESULTS
The Departments of Neurology, Cardiology, and Nephrology had a cumulative OPD attendance of 458 during the days of study, of which 47 patients were identified as in need of palliative care. The total number of inpatients admitted in 1 day in the wards of the three departments together was 53, of which five inpatients were identified as in need of palliative care. Hence, a total 52 patients were enrolled in the study, after obtaining their informed consent and are considered as study participants [Table 1].

Among the patients utilizing the outpatient services in the three departments, the percentage of patients requiring palliative care services in the Departments of Nephrology, Cardiology, and Neurology was, respectively, 12.86, 3.77, and 19.81. Similarly, among those utilizing the inpatient services of these departments, the percentage of them requiring palliative care was 15.38 in Nephrology and 20.00 in Neurology. None of the inpatients in Cardiology Department reported for palliative care services. Overall, the inpatients requiring palliative care services in the wards of the three departments was 9.38% and that of the outpatient wing of the three departments was 10.26%. In total, 52 patients (10.17%) required palliative care among the 511 patients who utilized the inpatient and outpatient services of the three departments at the time of the study [Table 1].
Nearly half of the study participants requiring palliative care (24/52, 46.15%) were suffering from neurological illness, mainly stroke. Cardiac illness accounts for less than one-fifth of the cases (15.39%) requiring palliative care and renal disease contributes about two-fifths of the total case (38.46%) requiring palliative care [Table 1].
Sociodemographic profile
The demographic characteristics of sex- and age-wise distribution of the patients requiring palliative care services show that, out of the 52 patients, 69.23% (36) were male and the remaining 30.77% (16) was female. Majority of them (63.46%) requiring palliative care were above 50 years of age, among them 22 were male participants (66.67%) and 11 were female participants (33.33%). The mean age of the respondents was 51.35 years [Table 2].
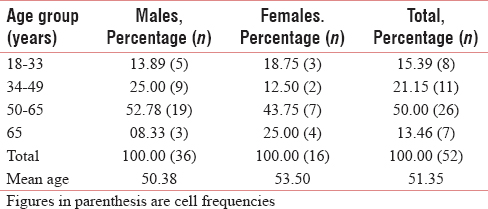
The sex-wise division shows that the mean age of male population was 50.38 years and that of females was 53.50 years.
Native participants (hailing from Puducherry) constituted more than half of the total patients (61.54%) followed by residents of Tamil Nadu (34.62) and a very few (3.84%) were from other neighboring states. The level of education of the patients requiring palliative care services was low and even more than one-fourth of them were illiterate. Poor people (88.46%) constituted major portion of the sample and also a good proportion was hailing from joint families (61.54%) [Table 3].

The socioeconomic profile of the participants revealed that they were from socially and economically lower strata.
Needs of patients requiring palliative care
Financial constraints were the most important concern from the point of the respondents followed by emotional and daily living activities.
Physical domain
Nine symptoms were identified as the physical domain. More than half of the patients complained of fatigue and sleeplessness. Less than one-fifth of them had problems of cough or nausea or pain [Table 4].

Other domains
Irrespective of the diseases, all patients faced with financial problems.
All the patients requiring palliative care experienced one or the other physical symptom and needed attention irrespective of the department from which they sought care. Majority of the patients requiring palliative care in the Department of Nephrology had financial concerns and were disturbed emotionally. All the cardiology patients in need of palliative care had financial constraints and they also had difficulty in carrying out their daily living activities. This trend was reflected in the neurology patients too [Table 5].

Slightly more than half of the patients who need palliative care services either quit or change their previous jobs due to diseases. It is more among neurological patients. However, the chances of quitting or changing jobs by caregivers were less due to disease condition of their wards [Table 6].

Majority of the patients (86.5%) requiring palliative care preferred to be beneficiaries of home-based palliative care services. Few patients (13.5%) opted for hospital-based palliative care. Care at home was preferred to that at the hospital most probably due to the positive family support at home, time and money that were spent in reaching the hospitals, and also the patients wish to have a peaceful end-of-life care enriched with the love from family members.
DISCUSSION
From a health delivery point of view, this study showed that one in ten patients who utilize the services of the Departments of Nephrology, Cardiology, and Neurology require palliative care. The findings of the present study thus confirm the observation reported earlier (Desmedt et al. (2011)).[7910]
Similar studies in Indian settings could not be found in published literature. However, the foreign studies showed similar results even though these were studies conducted in different settings.
Nearly half of the study participants requiring palliative care (46.1%) were suffering from neurological illness, mainly stroke and renal diseases accounted for about two-fifths (38.5%) of the total case requiring palliative care whereas cardiac illness accounted for less than one-fifth of the cases (15.4%) requiring palliative care. These evidences are comparable to the outcomes of the studies by Holloway et al., 2010, and Ghanem et al. (2011).[411] Cardiac cases requiring palliative care make up only 1.5% of the total cases. In a study by Gadoud et al. (2014),[12] it was found that, among patients with heart failure, about 7% was registered for palliative care. The low burden of cardiac disease in the present study is partly due to the fact that only postintervention patients admitted in the Cardiology ward and patients with conditions such as congestive cardiac failure, severe valve dysfunction, and heart disease-New York Heart Association class 3 or 4 are accommodated in the medical wards due to shortage of beds in the cardiology ward. Since medicine department was not included in the study, these cases were not included.
In the study by Desmedt et al. (2011),[10] 55% were female and the mean age was 72 years with a range of 21–99. The majority of patients were older than 65 years with a considerable number older than 80. The differences in outcome could be because the present study was limited to the departments of neurology, cardiology, and nephrology.
A study done in Hong Kong by Yong et al. (2009)[13] states that fatigue, cold aversion, pruritus, lower torso weakness, and difficulty in sleeping were the five most prevalent symptoms among end-stage renal disease patients. Similar results were observed in the present study also.
Nearly 90% of the study participants were experiencing financial problems. Three-fourth of the study participants experienced emotional discomfort. Nearly three-fourth of the participants experienced difficulties in carrying out their daily living activities and half of the participants were distraught psychologically, but only very few of them had spiritual issues.
The present study results were comparable with that of a study by Ryan et al. (2013)[14] which was done in English hospitals where sample consisted of 514 patients and physical, psychological, and social burden was evaluated among those meeting palliative care criteria (n = 185). They found that tiredness (34.6%), pain (31.1%), weakness (28.8%), and psychological discomfort (low mood: 19.9%; anxiety: 16.1%) are noted as being prevalent. Since the present study was limited to noncancer cases, pain was among the least reported symptom.
Strengths
Estimation of palliative care requirement of noncancer patients attending a tertiary care hospital and the quantification of their needs is a hitherto unexplored field in India. The study was conducted in both inpatient and outpatient wings of all the three departments mentioned above so as to ensure a comprehensive estimate of their requirement. Needs of patients requiring palliative care were assessed using validated questionnaire and their physical, psychological, financial, emotional, and spiritual domains were evaluated. Adequate time was spent with patients to elicit accurate responses. Investigator was trained in the administration of questionnaire and pretesting was done.
Limitations
The study was carried out within a short period of 6 weeks. Some specialties such as respiratory medicine, gastroenterology, orthopedics, surgery, and medicine where patients might have palliative care needs could not be included. The study was limited to cases presenting on a single day's OPD and inpatient department attendance in the selected department.
Recommendations
The daily requirement of palliative care services was around 10% in the three specialties alone which suggests that similar unmet need in palliative care services exists in other specialties and this has to be evaluated. Majority of the patients preferred home-based palliative care to hospital-based care. Hence, by means of workshops and continuing medical education, general practitioners in the periphery, doctors in JIPMER Rural Health Center (JRHC) and JIPMER Urban Health Center (JUHC), other medical personnel, and nongovernmental organizations (NGOs) should be sensitized to deliver palliative care services. Their cooperation can be sought for initiating a community-based palliative care delivery approach. JRHC and JUHC under the supervision of JIPMER can act as centers to impart essential training to caregivers and NGOs. Accredited Social Health Activist workers may be remunerated for identifying and delivering palliative care. Embarking on such novel path will pave way for establishing a community participatory approach to palliative care. One in ten noncancer patients in tertiary care hospitals may require palliative care services. This calls for an incorporation and initiation of palliative care services in other specialties to ensure holistic management of such cases.
Palliative care service calls for a team approach by consultants, paramedical personnel in unison with active participation of NGOs and caregivers as it is evident from the study that, apart from issues in physical domain, a substantial proportion of participants also had issues in the psychological, emotional, and financial domains. Counseling service has also to be rendered as a part of palliative care since a good share of the patients had psychological and emotional issues.
Policymakers of the government should be made aware regarding the dearth of quality palliative care service prevailing in the region and that formulation of a clear policy for establishing comprehensive palliative care services is the need of the hour. After such a clear policy has been drafted, an organized program for the delivery of palliative care may be launched.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Global Atlas of Palliative Care at the End of Life. 2014. Worldwide Palliative Care Alliance. Available from: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- [Google Scholar]
- 2015. WHO Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- Government of India. Proposal of Strategies for Palliative Care in India (Expert Group Report) 2012. Directorate General of Health Services Ministry of Health and Family Welfare. Available from: http://www.palliumindia.org/cms/wp.content/uploads/2014/01/National-Palliative-Care-Strategy-Nov_2012.pdf
- [Google Scholar]
- Palliative care consultations in hospitalized stroke patients. J Palliat Med. 2010;13:407-12.
- [Google Scholar]
- Hospital-based palliative care: A case for integrating care with cure. Indian J Palliat Care. 2011;17:S74-6.
- [Google Scholar]
- Palliative care in India: Current progress and future needs. Indian J Palliat Care. 2012;18:149-54.
- [Google Scholar]
- Palliative care need and management in the acute hospital setting: A census of one New Zealand Hospital. BMC Palliat Care. 2013;12:15.
- [Google Scholar]
- Validity, reliability and clinical feasibility of a Needs Assessment Tool for people with progressive cancer. Psychooncology. 2010;19:726-33.
- [Google Scholar]
- Descriptive epidemiological survey on a given day in all palliative care patients hospitalized in a French university hospital. Palliat Med. 1999;13:105-17.
- [Google Scholar]
- Palliative inpatients in general hospitals: A one day observational study in Belgium. BMC Palliat Care. 2011;10:2.
- [Google Scholar]
- Pattern of referral of noncancer patients to palliative care in the Eastern Province of Saudi Arabia. Indian J Palliat Care. 2011;17:235-7.
- [Google Scholar]
- Palliative care among heart failure patients in primary care: A comparison to cancer patients using English family practice data. PLoS One. 2014;9:e113188.
- [Google Scholar]
- Symptom burden and quality of life in end-stage renal disease: A study of 179 patients on dialysis and palliative care. Palliat Med. 2009;23:111-9.
- [Google Scholar]
- Symptom burden, palliative care need and predictors of physical and psychological discomfort in two UK hospitals. BMC Palliat Care. 2013;12:11.
- [Google Scholar]






