Translate this page into:
The Possible Role of Meditation in Myofascial Pain Syndrome: A New Hypothesis
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background of Hypothesis:
Myofascial pain syndrome (MPS) is the most common musculoskeletal pain disorder of the head and neck area. In the past, several theories were put forth to explain its origin and nature, but none proved complete. Myofascial pain responds to changing psychological states and stress, anxiety, lack of sleep, anger, depression and chronic pain are direct contributional factors. Myofascial pain syndrome may be considered as a psychosomatic disorder. There are numerous accepted palliative approaches, but of all, relaxation techniques stand out and initiate healing at the base level. In this article, the connection between mental factors, MPS and meditation are highlighted. Recent literature has shed light on the fundamental role of free radicals in the emergence of myofascial pain. The accumulating free radicals disrupt mitochondrial integrity and function, leading to sustenance and progression of MPS. Meditation on the other hand was shown to reduce free radical load and can result in clinical improvement. ‘Mindfulness’ is the working principle behind the effect of all meditations, and I emphasize that it can serve as a potential tool to reverse the neuro-architectural, neurobiological and cellular changes that occur in MPS.
Conclusions:
The findings described in this paper were drawn from studies on myofascial pain, fibromyalgia, similar chronic pain models and most importantly from self experience (experimentation). Till date, no hypothesis is available connecting MPS and meditation. Mechanisms linking MPS and meditation were identified, and this paper can ignite novel research in this direction.
Keywords
Meditation
myofascial pain
pain relief
psychosomatic disorder
MYOFASCIAL PAIN SYNDROME AND CURRENT PALLIATIVE METHODS
Myofascial pain syndrome (MPS) is a common dysfunction affecting up to 85% of general population.[1] It affects the muscles of mastication and neck and covers sensory, motor, and autonomic symptoms. This syndrome is associated with neurological, otologic, musculoskeletal, and gastrointestinal features.
MPS was originally described by Janet Travell (John F. Kennedy's physician) and David Simons. Kellgren published seminal papers in this area introducing the concept of trigger points.[23] In 1952, Travell and Rinzler explained the genesis of pain with illustrations depicting pain patterns of over thirty muscles.[4] MPS is characterized by the presence of tender zones called trigger points and each trigger point is composed of hypercontracted muscle fibers.[5] Palpation of trigger zones provokes radiating and referred pain in a certain pattern. The affected muscles are usually shortened with increased tone and tension. Some research suggests MPS as a reflex disorder caused by a reverberating circuit of sustained neural activity.[678] Chronic myofascial pain is usually a result of, and sometimes a product of, both emotional influences and physical factors.[6] According to Fricton et al., MPS is a regional muscle disorder that is associated with several behavioral, psychosocial, and cognitive contributing factors.[59101112131415] Once the contributing factors are recognized, they should be minimized. This may be possible with the help of meditation. MPS is usually managed by stretch and massage, thermotherapy, electrotherapy, laser therapy, dry needling, acupuncture, shockwave therapy, botulinum toxin type A injection, trigger point injections, pharmacological methods, and according to a recent report even hyperbaric oxygen therapy can be used.[1617181920] Pharmacological treatment methods include diclofenac patch, tramadol, tropisetron, opioids, lidocaine patch, tizanidine, benzodiazepines, cyclobenzaprine, thiocolchicoside, gabapentin, pregabalin, amitriptyline, duloxetine, sumatriptan, botulinum type A toxin, ketamine, L-tryptophan, and memantine.[21] Although medications provide improvement in acute cases, they carry a risk of adverse effects and offer only symptomatic relief. Nonpharmacological methods such as meditation do not carry the risk of adverse effects.
WHY MEDITATION?
Patients with myofascial pain commonly experience depression, sleep disturbance, anger, fatigue, and altered mental function. They frequently require an interdisciplinary approach to address the many dimensions of pain experience. Although medications are frequently advised, it is necessary to think of alternative therapies such as meditation. Meditation operates on a wide range of pain categories and can alleviate chronic pain in patients who do not respond to traditional medical care.[22] Meditation works better than morphine in pain management. However, the role of meditation has long been underestimated in the scientific community and has never tried in MPS. Therefore, I examined this potential arena while taking into account two important considerations:
-
Various precipitating factors are known to maintain MPS
-
Meditation alleviates all known precipitating factors of MPS.
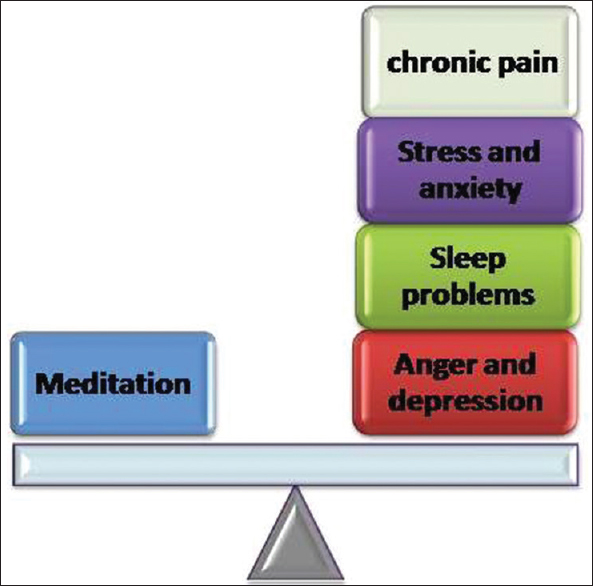
MPS has the characteristics of a psychosomatic condition. As meditation has substantial effect on pain perception, sleep patterns, psychological morbidity, and sympathetic nervous system, it seems reasonable to hypothesize that it can control the progression of MPS [Figure 1 and Table 1]. In the subsequent sections, evidence is presented supporting this hypothesis. The motivation to link meditation and myofascial pain came from direct participation and my observations during mindfulness meditation. I could overcome pain and symptom complex in MPS using meditation. This experience encouraged me to scientifically build on this hypothesis.
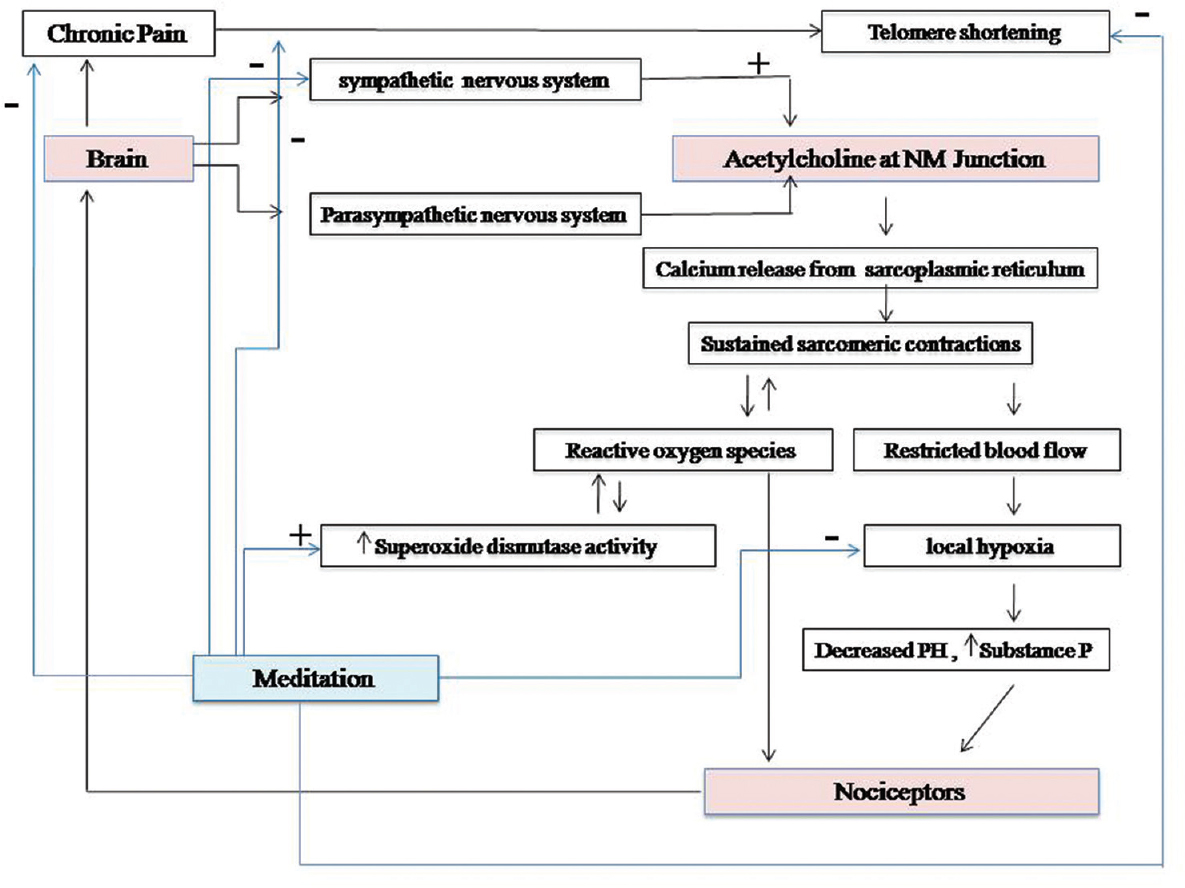
- Genesis of myofascial pain syndrome and the possible sites of action of meditation.
WHAT IS MEDITATION?
Meditation is a very ancient practice that originated in India. Later, it has spread out to China and Western world. In the recent years, it emerged as a new field that challenges even modern science in treatment and palliative care capable of improving health and well-being.[23] The word meditation is from the Latin word “meditation” meaning “to contemplate.” The Sanskrit root would be “dhyana.” The essence of meditation is “mindfulness or awareness” or simply “being in the moment.” “Mindfulness” is essentially a Buddhist concept - the word itself is an English translation of the Pali term “sati.” A good meditator witnesses all experiences regardless of their nature or valency (pleasant, unpleasant).[24] There are many techniques in meditation. They can range from mantra chanting (transcendental meditation [TM]) to more powerful mindfulness and insight meditations as taught in Zen. Despite the technique used, awareness remains as the essence of all forms of meditation. Awareness (of breath, mantras, thoughts, and emotions) liberates the hidden inner tendencies that lie dormant in the mind and results in emotional well-being. In mindfulness, there is expression or release of repressed thoughts or tendencies. The hidden tendencies lead to thoughts, and thoughts lead to emotions. A causal relationship exists between thoughts and emotions, one leading to the other. This chain can be broken with “awareness or mindfulness”. Meditators do not engage with the content of thoughts but experience them as they are, without judgment or analysis.[25262728]
At the biological plane, meditation decreases sympathetic activity, lowers cortisol (marker of stress), causes cortical thickening, and also brings specific changes in the electroencephalogram (EEG) that correspond to mental relaxation.[29] It also activates areas in the brain responsible for emotion regulation.[30] Mindfulness-based treatment programs were applied in the management of chronic pain, anxiety, emotional disorders, and mainly fibromyalgia (FM), a similar but a more generalized form of MPS.[31323334] The role of meditation in muscular pain disorders was identified early, but surprisingly no studies are available on its role in MPS.
FIBROMYALGIA: A MODEL SYSTEM FOR MYOFASCIAL PAIN SYNDROME
Many studies identified MPS and FM as similar conditions with overlapping biology and pathogenesis. Both are frequently associated with local tenderness, taut muscle bands, and active trigger points.[35] In FM multiple, generalized trigger points, generalized fatigue and musculoskeletal pain, poor sleep, headache, gastrointestinal disturbance, numbness, sensation of swelling occur more often compared to MPS.[34] Symptoms only vary in severity. In MPS, referred pain and taut bands are more common. FM is associated with poorer quality of life compared to MPS.[36] Coexistence of FM and MPS can also occur, and pain and tenderness in masticatory muscles may be an important component of FM.[37] The stomatognathic system is frequently involved in FM. FM and MPS hence represent two ends of the same clinical entity. In recent literature, mindfulness-based stress reduction reduced majority of FM symptoms including sleep quality and fatigue, and home practice reduced general symptom severity.[33] The positive impact of meditation on FM existed even after long observation period and was shown as a potential intervention in a quasi-randomized trial.[32]
Sufficient data are available on MPS, FM, meditation, and on the impact of meditation in FM. Owing to the similarities and overlap between FM and MPS, I have attempted to apply some of these findings to identify potential mechanisms involved in the alleviation of myofascial pain through meditation.
BRAIN SIGNATURE IN MYOFASCIAL PAIN: CAN MEDITATION GATE NEURAL PATHWAYS?
MPS produces a characteristic brain signature. Both structural and functional changes were noticed in patients with myofascial pain. Literature reported significant changes in gray matter and white matter anatomy. To investigate central nervous system (CNS) changes in MPS, high-resolution structural brain and brainstem scans are analyzed using voxel-based morphometric approaches. The first report of CNS changes in MPS was in 2011, by Younger et al.[38] Significant change (both decrease and increase) was noted in the gray matter volume as compared to controls mainly in the trigemino-thalamocortical pathway (trigeminal sensory nuclei, thalamus, and primary sensory cortex) and a decrease in gray matter volume was noted in the limbic system (posterior putamen, globus pallidus, and anterior insula). In another similar study, a regional decrease was found in white matter volume in the medial prefrontal cortex (PFC) bilaterally.[39] Furthermore, a decrease in gray matter volume occurred in the cingulate gyrus, insular cortex, frontal gyrus, and superior temporal gyrus bilaterally in the temporomandibular disorder patients. When myofascial trigger points were stimulated,[40] enhanced activity was found in somatosensory (SI, SII, inferior parietal, mid-insula) and limbic regions (anterior insula) and suppressed activity was found in the hippocampal area. In a positron emission tomographic study,[41] it was shown that induced jaw-muscle pain (a chronic pain model that mimics MPS) was associated with a significant increase in regional cerebral blood flow in the posterior insula, anterior cingulate, prefrontal cortices, right posterior parietal cortex, brainstem, cavernous sinus, and cerebellum indicating them as potential areas involved in assimilating jaw pain.
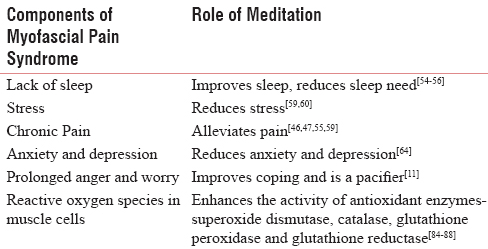
This link between the brain and MPS can be exploited constructively by meditation. It has a direct effect on all brain regions responsible for pain modulation [Figure 2]. Mindfulness meditation acts on the same brain regions that are responsible for the assimilation of myofascial pain. Meditation increases cerebral blood flow in the anterior cingulate cortex (ACC), PFC, insula (region involved in emotion regulation). Mindfulness meditation also regulates the autonomic nervous system by a midfrontal brain system.[42] Regular mindfulness practice causes a greater activation of ACC and less utilization of PFC. With constant practice, the utilization of the PFC-ACC regions and their connectivity with the amygdala and insula is enhanced. The primary somatosensory cortex shows high activity during pain and meditation reduces its activity significantly.
- A block diagram connecting areas of the brain that participate in pain, emotion, and autonomic regulation. These are potential areas involved in myofascial pain syndrome and probable targets of meditation.
Potential targets of meditation in the brain and regions which may involve in myofascial pain syndrome
The ACC is a center that consists of Brodmann area 24, 32, and 33. This brain region participates in pain, autonomic functions, impulse regulation, and emotion. The ACC is also associated with other functions deeply connected with conscious experience. Brodmann area 24 in ACC registers physical pain and its activity can be correlated with pain intensity. ACC is mainly linked to the experience of pain. It is involved in the emotional reaction to pain rather than to the perception of pain itself. Hence, there are two things, the sensation of pain and the emotional reaction to pain. Meditation works precisely in this area.
The insular cortex or insula is another important region in brain targeted by meditation. The insula, mainly the anterior region controls the autonomic nervous system (both sympathetic and parasympathetic limbs). It is believed to involve in consciousness and has been linked to emotion. Anatomically, the insular cortex is divided into a larger anterior region and the smaller posterior region. The anterior insula receives projections from the basal thalamus and has reciprocal connections with the amygdaloid complex. The posterior insula connects reciprocally with the secondary somatosensory cortex and receives input from thalamic nuclei. This region receives inputs from the posterior part of the thalamus specialized to convey pain information. Thalamus acts as a gateway that determines the flow of sensory (pain) information. Thalamic communication with higher centers is deactivated by mindfulness meditation and the pain signals simply fade away.[43]
Mindfulness meditation also reduces pain by activating the orbitofrontal cortex (Brodmann area 10, 11, and 47) [Figure 2].[43] The orbitofrontal cortex is a part of the PFC and an important area for cognitive processing. It receives projections from medial thalamus and is thought to participate in emotional processes. It also participates in both inhibitory and excitatory regulation of autonomic function. Connectivity of the orbitofrontal cortex with limbic areas includes reciprocal projections to insular cortex, parahippocampal regions, and hippocampus. The orbitofrontal cortex shares connections with limbic system, amygdala (extensive reciprocal connections), and direct and indirect connections with the hypothalamus.
Pain represents altered cortical activity and brings classic changes on the EEG. The experience of pain is associated with relatively lower amplitudes of slower wave (delta, theta, and alpha) activity and relatively higher amplitudes of faster wave (beta) activity.[44] Electroencephalographic studies on (insight) Zen meditation found increased alpha and theta activity in the frontal cortex, generally related to relaxation.[45] Theta activity, in particular, is a marker of deeper relaxation and is directly related to the degree of experience, being greater in more senior practitioners. EEG pattern changes in response to neuromodulatory approaches such as meditation which indicates pain modulation at cortical level. Recently, the brain wave pattern in FM and fatigue syndrome revealed an alpha rhythm disturbance (7.5–11 Hz) and alpha-delta sleep (alpha intrusions in nonrapid eye movement sleep).[4647] A similar phenomenon may occur in MPS. As meditation increases alpha, theta, and delta activity and corrects disturbed cortical activity, it can be considered.
Sleep disturbance, stress, anxiety, and depression in myofascial pain syndrome are alleviated through meditation
Several researchers point sleep deprivation as a contributory for pain syndromes in general and in myofascial pain. In an internet survey conducted on 2500 FM patients, insomnia was the most frequent aggravating factor.[48] Although many studies have shown a connection between pain syndromes and sleep disturbance, the direction of cause and effect is still a gray area. Studies attempted to answer this problem. Kundermann et al.[49] identified that pain sensitivity increases without any other general effects on physical sensation. Moldofsky and Scarisbrick[50] reported that sleep-deprived individuals have more musculoskeletal symptoms and a significant increase in muscle tenderness. Furthermore, musculoskeletal pain threshold decreases significantly in sleep-deprived individuals.[51] A close relationship was also found between increase in pain sensitivity and sleep debt in hours.[52] Pain and insomnia make a vicious cycle.
Meditation has unique effect on sleep. It reduces the need for sleep and improves the quality of sleep.[535455] In this way, it may arrest further progression of MPS. Shortage of sleep is also important cause of stress and anxiety, both contribute to MPS. Travell and Simon emphasized in their book titled, “Myofascial Pain and Dysfunction: Upper half of body” that an inquiry into the nature of sleep is important in MPS patients.[56] They stated that anxious and depressed patients have a trouble falling asleep. Painful muscles in MPS interrupt sleep and disrupted sleep can make the muscles even more painful. Impaired sleep occurs at a greater frequency in patients with severe myofascial pain.[56] Smythe considered sleep disturbances as one of the four important criteria in the diagnosis of FM.[56] Most of the FM patients demonstrate an overnight increase in the tenderness of the muscles. Improving sleep quality can reduce pain and fatigue, further supporting the hypothesis that sleep dysfunction is a pathogenic stimulus.[57] Sleep deprivation in healthy individuals can cause symptoms of myalgia, tenderness, and fatigue suggesting the possible role of sleep dysfunction in the origin of chronic muscle pain.[58] Epidemiological studies also indicate poor sleep quality as a risk factor for the development of chronic muscle pain. Sleep deprivation impairs descending pain-inhibition pathways that are important in coping with pain.
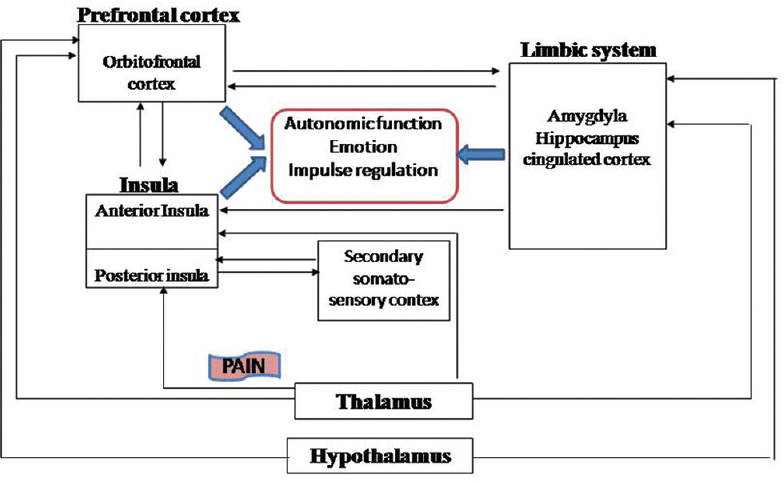
Stress and anxiety are the body's response to perceived physical and mental stress. Although anxiety is a short-lived in general population, in a few, it is almost a permanent state. In a meta-analysis, it was concluded that clinicians should discuss with their patients the role of meditation programs for psychological stress.[59] In various studies, stress was identified as a contributor for MPS. Hence, the role of stress in the progression of MPS cannot be underestimated. As meditation reduces stress, it can be considered.[60] Mindfulness meditation has promising potential as a nonpharmacologic treatment of chronic pain for patients with MPS.[61] The common benefits with mindfulness meditation include pain reduction, acceptance of pain, better sleep, and enhanced well-being [Figure 3].[6263] Based on available data, MPS seems closely related to chronic anxiety, depression, and other psychological states.[64] It is important to eliminate perpetuating factors to avoid recurrent episodes of pain.
- Meditation is a neuromodulatory practice capable of neutralizing the effect of perpetuating factors on myofascial pain syndrome.
Autonomic arousal in myofascial pain syndrome
Autonomic nervous system is pivotal in muscle contractility, genesis of muscle spasm, and MPS [Figure 1]. Acetylcholine produced near the motor endplate is necessary for muscle function. When sufficient amount is reached, the postsynaptic receptors are activated to initiate muscle action potential. The amount of acetylcholine is proportional to degree of sympathetic activity, which is further controlled by mental and psychosocial factors through inhibitory and excitatory pathways. Sympathetic output modulates contractility and sympathetic dominance alters muscle function. Sympathetic control naturally intensifies motor activity. MPS patients have shown altered autonomic function in many studies.[53] Meditation is a wakeful state accompanied by a lowering of cortical and autonomic arousal.[65] According to Park et al., mindfulness meditation can significantly lower the muscle sympathetic nerve activity.[66] In another study, physiological indices of stress were found to be lower in people who regularly practiced TM than nonmeditating control participants.[67] A noxious loud tone (100 db, 0.5 s, 3000 Hz) was presented to participants during normal waking and stress reaction to each tone as indicated by the galvanic skin response (GSR) was compared between the two groups.[67] GSR is a marker of autonomic arousal and its measures reflect sympathetic load or output. Habituation of the GSR to tones was faster for meditators than for controls, and meditators made fewer multiple responses during habituation indicating greater autonomic stability in response to stress. In many experiments, meditators were found to make fewer spontaneous GSR's than control participants. Thus, meditators were found to be more stable than controls on three autonomic indices: Rate of GSR habituation, multiple responses, and spontaneous GSR. In myofascial pain individuals, the autonomic responses are less stable, but in meditators responses are more steady.[29686970] Meditation can therefore play a pivotal role in treating underlying autonomic dysfunction in MPS.
POTENTIAL EFFECTS OF MYOFASCIAL PAIN SYNDROME AND MEDITATION AT CELLULAR SCALE
According to recent reports, MPS involves the formation of oxygen free radicals.[71] In the striated muscle, the accumulation of reactive oxygen species (mainly nitric oxide and superoxide radicals) contributes to contractile dysfunction and myopathy (both are components of MPS).[71] Superoxide radicals are normally acted upon by superoxide dismutases (SODs) and converted to hydrogen peroxide, which is later cleaved by either catalase or glutathione peroxidase. Reactive oxygen species are generated by electron transport chain and three additional sources. They include xanthine oxidase, phospholipase A2, and nicotinamide adenine dinucleotide phosphate oxidase 2-mediated pathways.[71] During sustained vigorous contractile activity (seen in MPS), the mitochondrial function increases many fold.[72] Reactive oxygen species generated in mitochondria and other nearby sites cause damage to mitochondrial components to initiate a chronic degenerative processes.[73] At subcellular level, mitochondria dysfunction is central to the pathogenesis of MPS. In the past, “mitochondria” was highlighted in a variety of clinical conditions ranging from neuropathic pain to chronic fatigue syndrome.[74] Meditation, both transcendental and insight type (zen), was showed to diminish oxidative stress.[75] The activity of antioxidant enzymes such as SOD, catalase, glutathione peroxidase, and glutathione reductase is enhanced in meditators. Meditation preferentially upregulates SOD activity, reduces lipid peroxidation, and is therefore an antioxidant therapy at cellular scale.[76777879] Lower oxidative stress, can improve mitochondrial performance, which is critical for effective calcium transport during muscle contraction.[80] An effective calcium transport is necessary for proper muscle function.
Chronic pain syndromes such as FM are also associated with chromosomal aberrations such as “telomere shortening.” Telomeres are protective caps located at the chromosomal ends. Telomere length is a metric of biological aging and cellular morbidity, and its assessment is an active research focus in pain syndromes. Patients with higher levels of pain within FM population were associated with shorter telomere length as compared to controls.[81] Furthermore, depression had a significant role. When both pain and depression were combined, patients categorized as “high-pain and high-depression” had shorter telomeres than those with “low-pain and low-depression.” Telomere length also correlated with pain threshold, pain sensitivity, and also gray matter volume. Patients with shorter telomeres were more sensitive to evoked pain and had less gray matter in the primary somatosensory cortex, the area associated with pain processing. Elizabeth blackburn (Nobel laureate-Physiology, 2012), who identified telomeres also conducted many studies on the effect of meditation on telomerase, an enzyme that maintains the size of telomeres. In one of her preliminary investigations, telomerase activity was found to be significantly elevated in the 3-month meditation retreat participants than controls.[82] We can expect somewhat similar results if mediation is tried in MPS patient population.
CONCLUSIONS
In this publication, the possible link between MPS and meditation was explored. Chronic pain, anger, anxiety, stress, and depression have a significant impact on certain areas of the brain and also on muscle fibers at a subcellular level leading to the progression of MPS. We can expect clinical improvement with meditation, as it reduces stress and psychological morbidity, which may be its triggers at the root level. Sympathetic burden is common to individuals with this condition, and meditation reduces sympathetic tone stabilizing autonomic function. Due to the effect on the sympathetic limb, muscle relaxation occurs as a byproduct of meditation. Brain plays a fundamental role in generation and modulation of myofascial pain. MPS is a central sensitization syndrome, and it is reasonable to consider meditation as a palliative intervention. Functional neuroimaging studies have revealed a network of brain regions in the limbic system, insula, PFC, and thalamus to be involved in the processing of pain information in general and especially myofascial nociceptive information. Meditation increases the activity in the same regions in the brain that participate in MPS. Meditation reduces the experience of pain (suffering) by uncoupling sensory dimension (pain sensation) from the intrinsic alarm response (emotional reaction to pain). The brain is highly plastic and responds promptly to changes in the degree of mindfulness. Many research, especially randomized controlled trails, are needed in this neglected area.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Discrepancy between prevalence and perceived effectiveness of treatment methods in myofascial pain syndrome: Results of a cross-sectional, nationwide survey. BMC Musculoskelet Disord. 2010;11:32.
- [Google Scholar]
- Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2007;21:427-45.
- [Google Scholar]
- Myofascial pain syndrome of the head and neck: A review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615-23.
- [Google Scholar]
- Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil. 1998;79:863-72.
- [Google Scholar]
- The spinal cord connections of the myofascial trigger spots. Eur J Pain. 2007;11:624-34.
- [Google Scholar]
- Alexithymia, anger and psychological distress in patients with myofascial pain: A case-control study. In: Front Psychol. Vol 4. 2013. p. :490.
- [Google Scholar]
- A simple working type classification proposed for the psychosomatic disorders of the oral cavity. J Coll Physicians Surg Pak. 2012;22:612.
- [Google Scholar]
- Myofascial temporomandibular disorder pain, parafunctions and psychological stress. J Oral Rehabil. 2008;35:45-52.
- [Google Scholar]
- Clinical survey of the patients with temporomandibular joint disorders, using Research Diagnostic Criteria (Axis II) for TMD: Preliminary study. J Craniomaxillofac Surg. 2012;40:366-72.
- [Google Scholar]
- The psychosomatic disorders pertaining to dental practice with revised working type classification. Korean J Pain. 2014;27:16-22.
- [Google Scholar]
- Nonpharmacological treatments for musculoskeletal pain. Clin J Pain. 2001;17:33-46.
- [Google Scholar]
- Meditative analgesia: The current state of the field. Ann N Y Acad Sci. 2014;1307:55-63.
- [Google Scholar]
- Current studies on myofascial pain syndrome. Curr Pain Headache Rep. 2009;13:365-9.
- [Google Scholar]
- A novel treatment modality for myofascial pain syndrome: Hyperbaric oxygen therapy. J Natl Med Assoc. 2009;101:77-80.
- [Google Scholar]
- An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4:33-47.
- [Google Scholar]
- What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002;64:71-83.
- [Google Scholar]
- Moving beyond Mindfulness: Defining Equanimity as an Outcome Measure in Meditation and Contemplative Research? Mindfulness (N Y) 2014 doi: 10.1007/s12671-013-0269-8
- [Google Scholar]
- Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57:35-43.
- [Google Scholar]
- A randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers. Evid Based Complement Alternat Med 2011 2011:960583.
- [Google Scholar]
- Baseline and strategic effects behind mindful emotion regulation: Behavioral and physiological investigation. PLoS One. 2015;10:e0116541.
- [Google Scholar]
- Measuring a journey without goal: Meditation, spirituality, and physiology. Biomed Res Int 2015 2015:891671.
- [Google Scholar]
- Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936-43.
- [Google Scholar]
- Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom. 2007;76:226-33.
- [Google Scholar]
- Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. Pain. 2011;152:361-9.
- [Google Scholar]
- Fibromyalgia and myofascial pain syndrome – A dilemma. Indian J Anaesth. 2009;53:575-81.
- [Google Scholar]
- The fibromyalgia and myofascial pain syndromes: A preliminary study of tender points and trigger points in persons with fibromyalgia, myofascial pain syndrome and no disease. J Rheumatol. 1992;19:944-51.
- [Google Scholar]
- A comparison study of quality of life in women with fibromyalgia and myofascial pain syndrome. Disabil Rehabil. 2004;26:198-202.
- [Google Scholar]
- Coexistence of fibromyalgia, temporomandibular disorder, and masticatory myofascial pain syndromes. Rheumatol Int. 2007;27:541-4.
- [Google Scholar]
- Chronic myofascial temporomandibular pain is associated with neural abnormalities in the trigeminal and limbic systems. Pain. 2010;149:222-8.
- [Google Scholar]
- Changes in regional gray and white matter volume in patients with myofascial-type temporomandibular disorders: A voxel-based morphometry study. J Orofac Pain. 2011;25:99-106.
- [Google Scholar]
- Central representation of hyperalgesia from myofascial trigger point. Neuroimage. 2008;39:1299-306.
- [Google Scholar]
- Central representation of muscle pain and mechanical hyperesthesia in the orofacial region: A positron emission tomography study. Pain. 2004;108:284-93.
- [Google Scholar]
- Central and autonomic nervous system interaction is altered by short-term meditation. Proc Natl Acad Sci U S A. 2009;106:8865-70.
- [Google Scholar]
- Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31:5540-8.
- [Google Scholar]
- Neuromodulatory treatments for chronic pain: Efficacy and mechanisms. Nat Rev Neurol. 2014;10:167-78.
- [Google Scholar]
- Zen meditation: An integration of current evidence. J Altern Complement Med. 2009;15:585-92.
- [Google Scholar]
- Alpha-delta sleep in patients with a chief complaint of chronic fatigue. South Med J. 1994;87:465-70.
- [Google Scholar]
- Sleep cycles and alpha-delta sleep in fibromyalgia syndrome. J Rheumatol. 1994;21:1113-7.
- [Google Scholar]
- An internet survey of 2,596 people with fibromyalgia. BMC Musculoskelet Disord. 2007;8:27.
- [Google Scholar]
- Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med. 1976;38:35-44.
- [Google Scholar]
- The effectiveness of physiotherapy and manipulation in patients with tension-type headache: A systematic review. Pain. 2004;112:381-8.
- [Google Scholar]
- The effects of total sleep deprivation, selective sleep interruption and sleep recovery on pain tolerance thresholds in healthy subjects. J Sleep Res. 2001;10:35-42.
- [Google Scholar]
- Altered autonomic function in patients with arthritis or with chronic myofascial pain. Pain. 1989;39:77-84.
- [Google Scholar]
- Meditation acutely improves psychomotor vigilance, and may decrease sleep need. Behav Brain Funct. 2010;6:47.
- [Google Scholar]
- “I felt like a new person.” the effects of mindfulness meditation on older adults with chronic pain: Qualitative narrative analysis of diary entries. In: J Pain. Vol 9. 2008. p. :841-8.
- [Google Scholar]
- Travell & Simons’ Myofascial Pain and Dysfunction: Upper Half of Body. Vol 1. USA: Lippincott Williams & Wilkins; 1999.
- Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014;174:357-68.
- [Google Scholar]
- Mind-body therapies – Use in chronic pain management. Aust Fam Physician. 2013;42:112-7.
- [Google Scholar]
- Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complement Altern Med. 2012;12:162.
- [Google Scholar]
- The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8:163-90.
- [Google Scholar]
- Contributing factors to chronic myofascial pain: A case-control study. Pain. 2003;104:491-9.
- [Google Scholar]
- Psychophysiological correlates of meditation. Arch Gen Psychiatry. 1975;32:1326-33.
- [Google Scholar]
- Mindfulness meditation lowers muscle sympathetic nerve activity and blood pressure in African-American males with chronic kidney disease. Am J Physiol Regul Integr Comp Physiol. 2014;307:R93-101.
- [Google Scholar]
- Autonomic changes in Brahmakumaris Raja yoga meditation. Int J Psychophysiol. 1993;15:147-52.
- [Google Scholar]
- Changes in autonomic variables following two meditative states described in yoga texts. J Altern Complement Med. 2013;19:35-42.
- [Google Scholar]
- Modulation of release of reactive oxygen species by the contracting diaphragm. Am J Respir Crit Care Med. 2000;161(3 Pt 1):891-8.
- [Google Scholar]
- Mitochondrial free radical generation, oxidative stress, and aging. Free Radic Biol Med. 2000;29:222-30.
- [Google Scholar]
- Mitochondrial dysfunction and molecular pathways of disease. Exp Mol Pathol. 2007;83:84-92.
- [Google Scholar]
- Roles of meditation on alleviation of oxidative stress and improvement of antioxidant system. J Med Assoc Thai. 2010;93(Suppl 6):S242-54.
- [Google Scholar]
- Can meditation slow rate of cellular aging? Cognitive stress, mindfulness, and telomeres. Ann N Y Acad Sci. 2009;1172:34-53.
- [Google Scholar]
- Lower lipid peroxide levels in practitioners of the transcendental meditation program. Psychosom Med. 1998;60:38-41.
- [Google Scholar]
- Effect of Zen meditation on serum nitric oxide activity and lipid peroxidation. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:327-31.
- [Google Scholar]
- Free radical-mediated skeletal muscle dysfunction in inflammatory conditions. J Appl Physiol. 2007;102:2056-63.
- [Google Scholar]
- Pain is associated with short leukocyte telomere length in women with fibromyalgia. J Pain. 2012;13:959-69.
- [Google Scholar]
- Intensive meditation training, immune cell telomerase activity, and psychological mediators. Psychoneuroendocrinology. 2011;36:664-81.
- [Google Scholar]






