Translate this page into:
Palliative Care Social Work In India: Current Status and Future Directions
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Palliative care (PC) involves total care for persons suffering from life-threatening illnesses and their families. Social work as a profession and an academic discipline is gaining momentum in India for the past few decades. A large number of professional social workers are working with individuals, families, and communities to provide PC in India. Authors have presented the current status of PC social work interventions and discussed the future directions in the practice, research, and training in PC and end-of-life care.
Keywords
Chronic illness
clinical social work
psychiatric social work
psychosocial
terminal illness
INTRODUCTION
The World Health Organization defines palliative care (PC) as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”[1] PC is considered under the human right to health.[2] PC is required for a wide range of disorders and conditions such as cardiovascular diseases, cancer, chronic respiratory diseases, HIV/AIDS, diabetes, and many other conditions that require PC, including kidney failure, chronic liver disease, multiple sclerosis, Parkinson's disease, rheumatoid arthritis, neurological diseases, dementia, congenital anomalies, chronic mental illness, spinal cord injuries, and drug-resistant tuberculosis.[2] Each year, an estimated 40 million people are in need of PC, 78% of whom live in low- and middle-income countries, and for children, 98% of those needing PC live in low- and middle-income countries.[23]
The concept of PC is relatively new one to India which was introduced only in the mid-1980s, and since then, hospice and PC services have developed with the efforts of committed individuals, organizations, and collaboration between national and international agencies.[4] In different parts of the world, including in Indian subcontinent, a number of major barriers exist in the efforts to meet the needs for PC, such as national health policies, health-care systems which do not often include PC services and training on PC for health professionals.[2356] PC starts with specific physical symptoms but it can only be completed by consideration of the patient's feelings and emotions, family's concerns, neighborhood, friendship networks, and sociocultural and political atmosphere.[7] As PC involves the total care for patients and families and it extends even after death of the person with illness, the best result is achieved through a multidisciplinary team comprising doctors, nurses, counselors, psychologists, social workers, and volunteers.[8]
PC as a specialty of service, practice, and an academic discipline requiring training is still in infancy in India, which is true in social work as in other disciplines. Many professional social workers have been working in PC in India for the past few years. In spite of this, there is no uniform way of “working or practice.” PC being a practice approach with significant volunteering opportunities and visibility value, there is ambiguity regarding the role played by the professional social workers. Authors attempt to explore and delineate the professional social work services in the area of PC and describe a framework for the same.
SOCIAL WORK IN PALLIATIVE CARE
The International Federation of Social Workers defines social work as “a practice-based profession and an academic discipline that promotes social change and development, social cohesion, and the empowerment and liberation of people. Principles of social justice, human rights, collective responsibility and respect for diversities are central to social work. Underpinned by theories of social work, social sciences, humanities and indigenous knowledge, social work engages people and structures to address life challenges and enhance wellbeing.”[9] According to the National Association of Social Workers (NASW), “clinical social work practice is the professional application of social work theory and methods to the treatment and prevention of psychosocial dysfunction, disability, or impairment, including emotional and mental disorders. The practice works with the goal of enhancement and maintenance of psychosocial functioning of individuals, families, and small groups.”[10] PC social work (PCSW) has developed primarily as a specialist health-related form of clinical social work and has been recognized and recommended as a necessary and appropriate part of PC.[7111213] The goal of PC and social work is one and same that to improve the overall quality of life of those who are suffering from any kind of problems.
Apart from the physical problems, the patient and the carers undergo significant psychosocial issues in individual, familial, and other social functioning and they may also need support for practical aspects of care such as financial, housing, aids to daily living, and spiritual care.[14] PCSW practice requires a variety of skills and have multiple roles to play in PC services, training, and research.[7] As a trained professional, the PC social worker prioritizes the problems and concerns of all involved parties and seeks to facilitate finding solutions for them. The PC social worker fulfills a valuable liaison role – patients, family members, nurses, physician, psychologist, clergy, and others are well served by an experienced PC social worker as member of the team.[7] As a part of the interdisciplinary team, PC social workers will represent the individual/family's wishes at every team meeting and advocate within systems to enhance their responsiveness and ensure that each patient and family receives care that is hand tailored to fit their needs.
Palliative social work assessment
Any PCSW intervention begins with psychosocial assessment. A PC social worker in the care setting should have adequate knowledge and skill to understand the physical symptoms and associated difficulties, psychiatric evaluation (annotation of patient history, mental status examination), and psychosocial assessment. The biopsychosocial approach provides the framework for assessment in the PC setting and this is carried out on the assumption of basic rights and social justice of persons with illness and their family for comprehensive understanding of the problems and culturally sensitive PCSW interventions. Assessment should cover the individual aspects of patient, familial, financial, and all other social aspects.[15] Interventions are guided by theoretical grounding which is drawn from a range of perspectives and models such as system perspective; medical model of a chronic illness; problem-solving approach; strength perspective; antidiscriminatory practice perspectives, rights-based approach; a partnership practice perspective, and community care model.[1617]
At the individual level, the assessment covers various components of a person's functioning as follows:
-
Biological factors
Process of disease progression, symptoms, past history, or comorbid illness and current health situation (including the impact of problems such as pain, ulcers, bleeding, sleep, delirium, decreased mobility, sexual functioning, etc.).
-
Psychological factors
Understanding about the disease, how they deal with life – their coping strategies/reactions to various crisis situations, risk of suicide/homicide, and client's goals in palliative treatment.[17] Chronic illness and difficulties associated with it may trigger reactive depression or anxiety disorders. Hence, periodic mental health assessment may be required for the affected person.
-
Spiritual factors
Indian psyche is rooted in cultural and spiritual beliefs. People often resort to spiritual, and as an extension, religious coping, in response to a life-threatening illness. It is necessary to understand and pay due attention to the patient's and caregiver's spiritual orientation, guiding spiritual/religious philosophies, spiritual metaphors that aid coping and preparation for end of life, resilience emanating from one's spirituality, and coming to terms with the life situation and reality, all of which influence PC planning.[17]
-
Social factors
Family factors, socioeconomic status, social support, knowledge and expectations of the patient and family, impact of the individual's illness on the family, and employment and resources in the family have to be taken into consideration, keeping a lie span perspective in focus.[18]
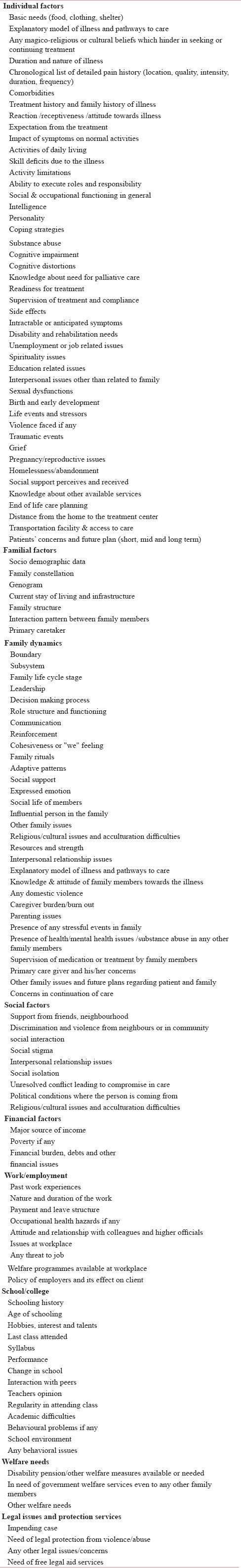
Family assessment is integral to understand the resources, limitations, and stress, thereby aiding in the development of effective care plan. Authors propose a framework of PCSW assessment [Table 1]. Assessment is the basis for formulating an individual intervention plan, which could be discussed in the multidisciplinary team. The interventions from PCSW perspective can be included, but are not limited to the following:
Social case work
As a method of social work, case work is concerned with the adjustment and development of individuals toward more satisfied life and well-being by alleviating psychosocial problems. The person who needs PC service is often under severe stress and psychological pain as they are undergoing life-threatening disease, advanced stages of life, and disabling conditions. These may make them to be isolated from mainstream and results in unemployment, financial burden, decreased family support, poor recreational activities, and other associated difficulties.[19] Arrangement of practical help and aids (such as wheelchair, walkers, and waterbed) also may improve the quality of life of patients with illnesses.
Breaking bad news
One of the most difficult tasks for clinicians as part of their care of patients is that of communicating the negative news, such as a severe diagnosis or disability or death. Most important is that the individual and the family have a right to know about his/her illness and also the news about death.[20] The way in which news about a terminal diagnosis or disability or recurrence is broken can have a profound effect on the patient's psychological health when the information given is perceived by the patient as too much or too little or as not expected by clinician; and if the resultant concerns remain undisclosed and unresolved, there is a high risk that the patient or family may develop clinical anxiety and/or depression or adjustment problems.[20] It is everyone's right to know about one's own health condition and it will help the clients to prepare their future in better ways. With adequate training and through evidence-based steps, PC social workers may break the bad news to patient and family members.[21]
Counseling and psychotherapy
As and when required, individual patients and their family members would benefit from counseling and psychotherapy. Working with this group from an existential therapy, supportive psychotherapy, and cognitive-behavioral perspectives has shown evidence in PC.[222324]
By the very definition of PC, it espouses a holistic approach to care. Spirituality becomes an essential component of this, and being a fatalistic and traditional society, Indian psyche is geared toward making sense of our experiences through a spiritual, often religious lens. Addressing this need, and facilitating religious/spiritual counsel as and when a patient or family requires, it may be coordinated by the PCSW team.[2526]
Family case work
Family members are the important team members in PC. The PC social worker assesses the caregiver's understanding about the disease (diagnosis, prognosis about the illness and its management), how they deal with life – their coping strategies/reactions to various crisis situations, risk of suicide/homicide, and client's/family's goals in palliative treatment, their grief, anxiety related to the future, caregiver burden, caregivers' and children's needs; respite care needs, financial problems, emotional and spiritual/religious issues, family structure; changes in the family dynamism (roles, leadership, communication, decision-making styles, and coping strategies), marital relationships, perceived and received social support, stigma, and discrimination-related matters, etc.
Family psychoeducation
This would enable the patients and their families to have a better understanding of the disease and to reinforce patients' strengths, resources, and coping skills. In this process, they are also equipped with skills necessary to deal with the periodic crises that are an inevitable part of a life-threatening, chronic illness.
Caregivers' mental health
The caregiver may need mental health evaluation and individual therapy for managing own negative emotions, grief, and depression.
Family therapy is necessary when the impact of the illness threatens the family equilibrium or aggravates a preexisting family pathology. Collusion (withholding of information) is very common in India, where family members make most of the decisions of health care for the patient. At times, they insist on not telling the patient anything about the disease or its likely progression. Family therapy or cognitive reframing helps bring behavioral and attitudinal changes; reduces interpersonal barriers; and helps deal with collusion in a better way.[17] The caregiver may be performing practical caregiving at home (e.g., catheter management), which needs training, supervision, and guidance.
Discussing ethical issues
Ethical dilemmas such as the decisions on continuing life support, withdrawing or withholding treatmentinevitably arise in life threatening situations. These discussions are ably mediated by the PC social workers. With their skills in problem solving, crisis management, facilitating, advocacy and networking PC social workers aid to find solutions that are helpful for each family considering their unique problems.[27] PC social work services does not end with the death, but continue throughout the bereavement period and longer until the family is able to manage independently..
Social group work
Group work seeks to facilitate the intellectual, emotional, and social development through group activities. Group activities are the strategic plans administered in PC, which have the effects of both psychosocial healing and an intervention model for holistic development. Group education programs for patients and families have shown significant positive outcomes in many studies.[2728] Educative, recreational groups may be possible in hospice/hospital/clinic and community settings in PC for patients, family members, and PC staff and volunteers. Patient and family self-help and bereavement groups help the family think of ways to take care of themselves and to cope with loss/grief and they also provide support to caregivers. The Indian Cancer Society (ICS) and the Cancer Patient Aid Association (CPAA) are some of the family and patient support groups available to cancer patients in India.[17]
Working at the community level
Hospice and home-based care
The main approach to care for patients who suffer from life-threatening disorders in developed countries is hospice care services. The need for improved hospice care in developing countries is high, and it is underexplored so far.[29] In general, hospice means specialized care that provides comfort and supportive end of life care to the patients and their families when curative treatment has not worked and death is inevitable. In Indian situation, with limited resources in health-care sector, care takes place at the home setting, with the family members being responsible for direct and indirect caregiving. Hospital/hospice services run by nongovernmental organizations (NGOs) and the government are the main health-care resources for this group.
It is recommended that the community models for the provision of home-based PC are possible by involving various community caregivers and supervised by health-care professionals trained in PC.[30] In this context, PC social workers play the vital role in linking the family with the necessary support and services. The strong community orientation inherent in PCSW training helps in this process by involving different stakeholders and facilitating the care in the community. Thus, it is necessary to understand various factors such as the community/social factors for comprehensive assessment and interventions. PC social workers have to understand social support, availability of resources, societal structures, and barriers to accessing community resources, cultural values and beliefs, existing health-care facilities – their availability, accessibility, and affordability. As structural inequities such as poverty and gender and caste-based exclusion (women and some caste groups in India are marginalized and are largely excluded from health-care services) are barriers in health-care services, they need to be addressed in a systemic perspective.[17]
Program planning and development
The PC social workers in the community use their skills in service and developing program models. It includes conducting periodic survey of PC needs of people in a particular community and ensuring availability of services for them, forming group/organization, and providing training for of those who are interested (may be volunteers from diverse field includes college/school students, National Service Scheme, National Cadet Corps, Nehru Yuva Kendra volunteers, Accredited Social Health Activists, etc., or neighbours) in providing PC. Neighborhood network in PC in Kerala is a successful example of such a model.[3132] Resource mobilization (financial, material, human resources, etc.) is a felt need of individuals and families requiring PC services. Working with government organizations such as panchayathiraj institution/district authorities to help them develop PC delivery care plans, policies and programs, advocacy and network with various governmental organizations/NGOs for policies, programs, and necessary services for patients and families becomes a mandate for social workers in PC. Networking with the NGOs becomes a useful approach in this process. The ICS and CPAA are some of the family and patient support groups available to cancer patients in India.[17]
At macro level, developing the understanding about the care needs among the community groups through awareness programs among public will help mobilize the involvement of various stakeholders in PC. Community support aids in facilitating the available welfare measures to support family caregivers in becoming independent after the loss of an earning family member. This may be through networking and liasoning with various groups to provide vocational training, jobs, monetary help to start their own small business, and educational support (fees, uniforms, books, shoes, and writing material) for siblings or children of the patients and their dependents.[17]
Research and advocacy
Documentation is essential for accountability and dissemination of good practices, which then serve as models to be emulated. Advocacy for PC needs to be strengthened at different levels. Hence, building evidence for support in PC needs, in general, and for specific PCSW services is essential. The findings from such efforts can help in establishing effective programs and informing practice. Identifying issues and undertaking action researches for evidence-based best practices for different disease-specific groups is crucial. Developing evidence-based policies and programs related to PC is very important, in which the PC social worker can play a pivotal role.[17]
CARING FOR THE CARERS
Although staff stress and burnout in hospice or PC has been demonstrated to be lesser, studies have noted suicidal ideation, increased alcohol and drug usage, anxiety, depression, and difficulty in dealing with issues of death and dying along with secondary traumatic stress, compassion fatigue, and burnout including in palliative social workers.[53334] Emotional and spiritual support to the team (physicians, nurses, and volunteers) is very important. Burden and burnout may negatively influence the functionality. Supervised PCSW, opportunities for peer supervision and personal therapy, the professional competence and freedom to know when the palliative social worker is emotionally over involved, and to seek help for the same are essential toward ensuring better functioning as a PC social worker.
PALLIATIVE CARE SOCIAL WORK TRAINING AND STANDARDS OF PRACTICE
Social work training empowers trainees in working with and being sensitive to individuals and families from varying cultures, ages, and socioeconomic status. This enables them to help individuals and families across the lifespan in coping with trauma, suicide, illness, and death. Irrespective of the setting that a social worker is working in, they are called to provide support in various areas of psychosocial needs and they must be prepared to assess such needs and intervene appropriately. In India, social work knowledge and skill development in the PC and end of life care is uneven and not integrated sufficiently with theoretical concepts and research in students' graduation and postgraduation level. While the 2-year predoctoral program in clinical and psychiatric social work serves to develop clinical competencies, skill development for end of life care is not given due focus.
PC social workers should develop competencies in palliative and end-of-life care to work with individual, family, group, team, community, and organizational interventions that extend across settings, cultures, and populations and encompasses advocacy, education, training, clinical practice, community organization, administration, supervision, policy, and research.[35] It is the need of the hour to develop competent human resources in PCSW to cater the needs of PC in India. For this, social work curriculum should include PC and end-of-life care theory and practice from graduation level onward. A PC social worker should be knowledgeable about and competent to follow values and ethics in social work practice in PC. In the absence of established codes of practice in India, PC social workers would benefit from following the Standards for Palliative and End of Life Care set by the NASW.[36]
CONCLUSION
PC social workers work in individual, familial, and community level to provide comprehensive PC service and add quality of life to the individuals suffering from terminal or life-threatening diseases and their families. PCSW is in its infancy stage in India in terms of practice, training, and research. Training in PC and end-of-life care needs to be included in graduation level of social work education. More structured training programs are required during the academic period and as part of continuing education programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2016. Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- Palliative care in India: Successes and limitations. J Pain Palliat Care Pharmacother. 2003;17:121-8.
- [Google Scholar]
- Hospice and palliative care development in India: A multimethod review of services and experiences. J Pain Symptom Manage. 2008;35:583-93.
- [Google Scholar]
- Barriers and challenges encountered by end-of-life care professionals: An Indian perspective. In: Journal of Palliative Care. Canada: Centre Recherche Institut Univ Geriatrie Montreal; 2014.
- [Google Scholar]
- Improving access to opioid analgesics for palliative care in India. J Pain Symptom Manage. 2002;24:152-9.
- [Google Scholar]
- Oxford textbook of palliative medicine. USA: Oxford University Press; 2011.
- Palliative care in India: Current progress and future needs. Indian J Palliat Care. 2012;18:149-54.
- [Google Scholar]
- 2014. Global Definition of Social Work. Available from: http://www.ifsw.org/get-involved/global-definition-of-social-work/
- 1989. NASW Standards for the Practice of Clinical Social Work. Available from: http://www.socialworkers.org/practice/standards/clinical_sw.asp
- Developments in end-of-life and palliative care social work international issues. Int Soc Work. 2009;52:513-24.
- [Google Scholar]
- Relationships between social work involvement and hospice outcomes: Results of the national hospice social work survey. Soc Work. 2004;49:415-22.
- [Google Scholar]
- Job satisfaction: How do social workers fare with other interdisciplinary team members in hospice settings? OMEGA J Death Dying. 2004;49:327-46.
- [Google Scholar]
- Psychosocial issues in palliative care. New York: Oxford University Press; 2008.
- Guideline for social work assessment in mental health settings. Int J Res Sci Innov. 2015;2:165-8.
- [Google Scholar]
- Palliative care: An Indian perspective. In: Altilio T, Otis-Green S, eds. Oxford Textbook of Palliative Social Work. New York: Oxford University Press; 2011.
- [Google Scholar]
- Life-Span Development. Boston, MA: McGraw-Hill; 2009.
- Integrated Practice of Social Work Methods: Prospects of Social Work Intervention Through Community Palliative Care. Social Work Chronicle. 2013;2(1):1-13.
- [Google Scholar]
- Breaking bad news: Consensus guidelines for medical practitioners. J Clin Oncol. 1995;13:2449-56.
- [Google Scholar]
- Counselling and psychotherapy in palliative/hospice care: A review. Palliat Med. 1988;2:36-50.
- [Google Scholar]
- CBT for chronic illness and palliative care: A workbook and toolkit. England: John Wiley & Sons; 2013.
- Existential psychotherapy in palliative care. In: Chochinov HM BW, ed. Handbook of psychiatry in palliative medicine. New York: Oxford University Press; 2000. p. :197-214.
- [Google Scholar]
- Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. J Palliat Med. 2009;12:885-904.
- [Google Scholar]
- Effects of spiritual care training for palliative care professionals. Palliat Med. 2005;19:99-104.
- [Google Scholar]
- Evaluation of a psycho-educational group programme for family caregivers in home-based palliative care. Palliat Med. 2008;22:270-80.
- [Google Scholar]
- Teaching family carers about home-based palliative care: Final results from a group education program. J Pain Symptom Manage. 2009;38:299-308.
- [Google Scholar]
- Perspective of patients, patients' families, and healthcare providers towards designing and delivering hospice care services in a middle income country. Indian J Palliat Care. 2015;21:341-8.
- [Google Scholar]
- Palliative care in India: Situation assessment and future scope. Indian J Cancer. 2015;52:99-101.
- [Google Scholar]
- A model for delivery of palliative care in India – The Calicut experiment. J Palliat Care. 1999;15:44-9.
- [Google Scholar]
- Secondary traumatic stress and oncology social work: Protecting compassion from fatigue and compromising the worker's worldview. J Psychosoc Oncol. 2005;23:1-14.
- [Google Scholar]
- Social work competencies in palliative and end-of-life care. J Soc Work End Life Palliat Care. 2005;1:87-120.
- [Google Scholar]
- 2004. Standards for Palliative and End of Life Care. Available from: https://www.socialworkers.org/practice/standards/Palliative.asp






