Translate this page into:
Patients with End-stage Interstitial Lung Disease may have More Problems with Dyspnea than End-stage Lung Cancer Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Patients with end-stage interstitial lung disease (ILD) do not appear to receive adequate palliative care despite apparent suffering before death. The aim of this study was to evaluate their signs, symptoms, and treatment received before death.
Methods:
Patients with ILD and lung cancer (LC) who were hospitalized and died in our hospital were enrolled retrospectively. Signs and symptoms and treatments at 7 days, 3 days, and 1 day before death were evaluated and compared between the two groups of patients.
Results:
A total of 23 patients with ILD and 59 patients with LC group were eligible for participation. Significantly more LC patients had loss of consciousness than ILD patients on 7 days (ILD: LC = 1 [5.6%]:24 [41%], P = 0.013), 3 days (1 [5.6%]:33 [56%], P < 0.001). Significantly more ILD patients had dyspnea than LC patients on 3 days (16 [89%]:38 [64%], P = 0.047) 1 day before death (21 [91%]:33 [56%], P = 0.001). On 1 day before death, significantly more LC patients received morphine than ILD patients (2 [8.7%]: 14 [24%], P = 0.015). More ILD patients received sedation (11 [48%]: 11 [19%], P = 0.007).
Conclusions:
End-stage ILD patients may experience dyspnea more frequently than terminal LC patients, and they need sedation. Morphine should be administered to ILD patients who have dyspnea. Additional prospective studies are needed.
Keywords
Dyspnea
Interstitial lung disease
Morphine
Palliative care
INTRODUCTION
Interstitial lung disease (ILD), especially idiopathic pulmonary fibrosis (IPF), is a fatal disease with a poor prognosis, and the therapeutic options are limited.[123] The mean survival time of patients with IPF in Japan is 61 months.[4] Moreover, most end-stage patients with ILD have dyspnea, hypoxemia, and cough.[5] These signs and symptoms, in the end, stage are similar to those of patients with lung cancer (LC). ILD patients generally do not receive adequate palliative care in Japan. Less ILD patients receive morphine even if they suffer from dyspnea than LC patients.[56] In addition, the guidelines from the Japanese Respiratory Society (JRS) only contain recommendations on the diagnosis and treatment of ILD, which may account for why ILD patients are infrequently provided palliative care.[7] By contrast, there are guidelines on palliative care for ILD patients based on collaboration between several medical societies.[89] Moreover, the current view in the United Kingdom is that access to palliative care should be based on patients’ needs instead of a diagnosis.[1011] While the patients with ILD cannot be admitted to the palliative care units because only malignancy and advanced immunodeficiency syndrome patients can admit to these facilities in Japan, 8.5% of the patients with lung disease who admitted to hospice have noncancer in the US,[12] and both patients with ILD as well as patients with LC receive palliative care in Western countries.
To the best of our knowledge, there have not been any studies comparing the signs and symptoms of end-stage ILD and LC patients during the last few days of life, although physicians realize that patients with end-stage ILD have distress as often as patients with LC. The aim of this study was to evaluate the signs, symptoms, and treatments of patients with ILD before death. This study found that end-stage ILD patients had the same signs and symptoms as end-stage LC patients.
METHODS
Patients
This retrospective study was performed at Komatsu Municipal Hospital (340-bed community hospital). Patients with a diagnosis of ILD who were admitted to and died in this hospital from January 2007 to September 2013 were enrolled in this study. ILD was defined based on the American Thoracic Society/European Respiratory Society/JRS/Latin American Thoracic Association idiopathic interstitial pneumonia (IIPs) consensus guidelines 2002[13] and 2013.[14] ILD associated with collagen-vascular disease was included. Data from surgical lung biopsies were not required. Patients with LC who were admitted to and died in our hospital during the same period were also enrolled in this study. All patients were admitted to receive palliative care only. Therefore, patients receiving specific antitumor-specific treatment such as chemotherapy and radiation therapy were excluded. The types of LC included pathologically proven small cell and nonsmall cell carcinoma. The study protocol was approved by the Institutional Review Board of Komatsu Municipal Hospital.
Factors analyzed
Clinical data were collected from electronic medical records. Signs and symptoms at 7 days, 3 days, and 1 day before death was examined for both groups of patients. The frequencies of the following signs and symptoms were determined: Level of consciousness, cough, sputum, fatigue, delirium, dyspnea, appetite loss, and pain. Loss of consciousness was defined as more than one point of the Japanese Coma Scale.[15] Causes of loss of consciousness were then researched. Nurses assessed these symptoms and recorded on the medical record. We could not evaluate the relationship between laboratory findings and several symptoms because only six patients underwent laboratory testing of blood samples and arterial blood gas analysis during the study period.
The following treatments received by the patients were investigated: Sedation, intubation, nonintubated ventilation, supplemental oxygen, opioids, and antimicrobials and glucocorticoids based on clinical condition. Sedation was evaluated if a patient received it to reduce subjective dyspnea. Patients who received morphine for analgesia were excluded from the study. Patients who were administered morphine for dyspnea were included this study.
Statistical analysis
The signs, symptoms, and treatments of ILD and LC patients were compared. Continuous variables with a normal distribution were compared using the Student's t-test. The Wilcoxon rank sum test was used for variables with a nonnormal distribution. The Chi-square statistic or Fisher exact test was used to compare categorical variables. Differences were assumed to be significant for P < 0.05. Analyses were performed using SPSS for Windows, version 20.00 (SPSS Inc., Chicago, IL, USA).
RESULTS
Patient characteristics
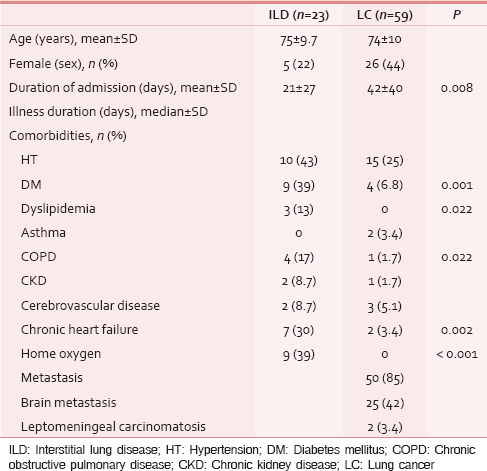
Patient characteristics are shown in Table 1. There were 23 ILD patients and 59 LC patients with 5 (22%), and 26 (44%) female patients, respectively. The respective mean ages were 75 ± 9.7 years and 74 ± 10 years. There were no significant differences in the ages and numbers of each gender between ILD and LC patients. The duration of hospitalization of the LC patients was significantly longer than for the ILD patients (42 ± 40 days versus 21 ± 27 days, respectively; P = 0.008). Five ILD patients died within 2 days from the date of admission, whereas only one LC patient died within 7 days from admission. Diabetes mellitus, dyslipidemia, chronic obstructive pulmonary disease (COPD), and chronic heart failure were significantly more common in patients with ILD. Fifty LC patients (85%) had metastatic disease when admitted, including 25 patients (42%) with brain metastasis and two patients (3.4%) with leptomeningeal carcinomatosis.
Signs and symptoms
The signs and symptoms of patients are shown in Table 2. Significantly more LC than ILD patients were not conscious at 7 days (26 [45%] vs. 2 [11%] respectively; P = 0.012) and 3 days (37 [63%] vs. 4 [22%], respectively; P = 0.003) before death. Anorexia was also more frequent in LC patients than in ILD patients at 7 and 3 days before death. Patients with LC had pain more frequently than ILD patients on days 7-1 before death. Significantly more ILD patients than LC patients felt dyspnea at 1 day (21 [91%] vs. 33 [56%], respectively; P = 0.001) and 3 days before death (16 [89%] vs. 38 [64%], respectively; P = 0.047).

Medications and care
The medications and types of care received by study patients are shown in Table 3. Each physician decided whether to administer any sedative agents. More ILD than LC patients received sedation on day 1 before death (P = 0.007). There were more ILD patients who received morphine to reduce dyspnea in LC patients than ILD patients throughout 1-7 days before death. Midazolam was more frequently administered to ILD patients than LC patients 1 day before death (P = 0.031). Two patients at 1 day before death, one patient at 3 days before death and one patient at 7 days before death received midazolam for sedation. The remaining patients received midazolam to relieve distress. There were no patients who received midazolam as an anti-anxiety agent. Antimicrobials were more frequently administered to ILD than LC patients on days 7-1 day before death. Intubation and urethral catheterization were used more frequently for ILD than LC patients on days 7-1 day before death. Advanced directives were discussed with all LC patients, their families, and medical staff. On the other hand, three ILD patients (13%) did not make a decision for advance directive at 1 day before death.

Causes of loss of consciousness
Causes of loss of consciousness is described in Table 4. Receiving sedative agents was most commonly seen in ILD patients at 7 days, 3 days, and 1 day before death. On the other hand, disease progression was most commonly seen in LC patients. Furthermore, brain metastasis, delirium, hypercalcemia, and carcinomatous meningitis were also the reasons of loss of consciousness in LC patients. Patients who received sedative agent was less in LC patients than ILD patients at 7 days to 1 day before death.

DISCUSSION
Our study found that ILD patients have dyspnea more frequently than LC patients during the end stage of disease. LC patients needed to receive sedative agent more frequently than ILD patients because they suffered more distress and the other medication could not relieve these symptoms. This indicated that ILD patients may have more problems with dyspnea than LC patients. Arita et al. reported that 97% of ILD patients had dyspnea until 3 days before death,[5] and Bajwah et al. reported that 93% of ILD patients had dyspnea during their last year of life.[16] On the other hand, the prevalence of dyspnea in patients with advanced cancer ranges between 19% and 51%, and over 60% of advanced cancer patients with dyspnea have moderate to severe dyspnea.[17] Although these studies evaluated patients during various stages of their disease and did not evaluate end-stage patients, the results of these studies and our study suggest that end-stage ILD patients may have more severe dyspnea than terminal LC patients.
Our study found that more ILD than LC patients were conscious on days 7-3 before death. Arita et al. reported that 45% of ILD patients had loss of consciousness 24-48 h before death,[5] which is similar to our study findings. Moreover, loss of consciousness was not a finding in two case-control studies of ILD patients with acute exacerbation (AE), which is frequently fatal.[1819] Our study found that 45-88% of LC patients developed loss of consciousness. Unlike ILD patients, there were several causes of loss of consciousness such as brain metastasis, delirium, hypercalcemia, and carcinomatous meningitis in LC patients. Patients with malignancy sometimes develop an altered level of consciousness, because of brain metastasis,[20] leptomeningeal carcinomatosis,[21] hypercalcemia due to pseudohyperparathyroidism,[22] Hyponatremia,[23] hypoxemia, hypercapnia,[24] and delirium.[25]
Morphine is commonly used to reduce dyspnea in palliative medicine.[26] The effects of morphine, including suppression of respiratory center sensitivity in the brain stem, reduced oxygen consumption as a result of reduced respiratory rate, elevation of endogenous endorphin levels, central sedation, and improvement of heart failure, are thought to play roles in the relief of dyspnea.[27] Results of two clinical studies indicate that morphine was an effective pharmacological agent for dyspnea in cancer patients.[2829] As shown in this study, morphine was not commonly used for dyspnea in ILD patients, however, Allen et al. found that subjective breathlessness, determined on a 100-mm visual analog scale, fell by a mean of 47 mm during the first 15 min after the first morphine injection of patients with IPF.[30] Although nebulized morphine is a treatment used for dyspnea, it was not effective for improving the dyspnea of patients with ILD during exercise.[31] A systematic review in the management of dyspnea reported that oral and parenteral opioids were more effective than nebulized opioids, and the data from the meta-analysis was insufficient for concluding whether nebulized opioids were effective.[26] These studies were all performed in Western countries, and there have not been any Japanese studies. In fact, patients with nonmalignant disease do not tend to receive opioids treatment even if they are suffering from dyspnea.[45] In our study, there were only two patients (8.7%) with ILD, who received morphine for their dyspnea, and both patients had concomitant malignant disease.
In our study, most ILD patients were administered midazolam for sedation. Bajwah et al. reported that eight patients (18%) with ILD received benzodiazepines for dyspnea, which was effective in 7 (88%).[16] Navigante et al. demonstrated that morphine was useful for controlling baseline levels of dyspnea in cancer patients, and dyspnea was improved when midazolam was used in addition to morphine.[32] However, a review of several studies found no evidence that benzodiazepines were effective in relieving breathlessness of patients with advanced cancer and COPD. Furthermore, there were no studies on the efficacy of benzodiazepines for ILD patients with dyspnea.[33] Therefore, morphine should be administered not only for patients with LC, who have dyspnea but also for patients with ILD who have dyspnea.
It is difficult for physicians to recognize whether patients are end stage or not. The clinical presentation of many ILDs is insidious.[34] Some ILD progress gradually, the other patients may present acutely because of AE or infection. The most common cause of death is AE in Japan.[35] AE-ILD is a fatal and progressive disease. Several studies researched that age at the onset, respiratory status before the AE, low C-reactive protein and lactose dehydrogenase were prognostic factors for AE-ILD.[3637] These factors may be tools to recognize patients’ prognosis. On the other hand, progressive breathlessness and respiratory failure are common natural history for the patients whose diseases progress slowly.[34] These patients may be easily assessed end stage such as LC patients.
This study has several limitations. First, it was a retrospective analysis with a very small study population. Second, we could not objectively evaluate the signs and symptoms of any of the patients, because the electronic medical record did not include these descriptions. Third, our study patients with ILD had various types of disease. Finally, since this was a retrospective study, it is possible that selection bias was present. Therefore, additional prospective studies using objective assessments and enrolling more patients are needed to confirm and further clarify these results.
CONCLUSIONS
Terminal ILD patients may experience dyspnea more frequently than end-stage LC patients, and they need sedation. To relieve their distress, morphine should be used more frequently than its current practice, for ILD patients with dyspnea. Additional prospective studies using objective assessments and more patients are needed to accurately determine how morphine is used for terminal ILD patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We appreciate the assistance with methods in the study provided by Hidekazu Ino, the department of internal medicine, Komatsu Municipal Hospital (Japan). We are also grateful for the diligent and thorough critical reading of our manuscript by Mr. John Wocher, Executive Vice President and Director, International Affairs/International Patient Services, Kameda Medical Center (Japan) and Yoshihido Ohkuni, department of respirology, Kameda Medical Center (Japan).
REFERENCES
- Predicting survival in idiopathic pulmonary fibrosis: Scoring system and survival model. Am J Respir Crit Care Med. 2001;164:1171-81.
- [Google Scholar]
- Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;157:199-203.
- [Google Scholar]
- A histologic pattern of nonspecific interstitial pneumonia is associated with a better prognosis than usual interstitial pneumonia in patients with cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med. 1999;160:899-905.
- [Google Scholar]
- Nationwide epidemiological survey of patients with idiopathic interstitial pneumonias using clinical personal records. Nihon Kokyuki Gakkai Zasshi. 2007;45:759-65.
- [Google Scholar]
- Studies of palliative care for pulmonary fibrosis and interstitial pneumonia at the end-of-life over the last 20 years. Jpn J Chest Dis. 2010;69:354-61.
- [Google Scholar]
- A study of clinical features of patients with end – stage pulmonary fibrosis under home oxygen therapy. Respir Res. 1995;14:868-73.
- [Google Scholar]
- Idiopathic Interstitial Pneumonias: Diagnosis and Treatment (2nd ed). Tokyo: Nankodo; 2011.
- An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788-824.
- [Google Scholar]
- National Institute for Health and Care Excellence (NICE) In: The diagnosis and management of suspected Idiopathic pulmonary fibrosis. Manchester: National Institute for Health and Care Excellence; 2013.
- [Google Scholar]
- Reaching out: Specialist palliative care for adults with non-malignant disease. London: National Council for Hospices and Specialist Palliative Care Services; 1995.
- National Hospice and Palliative Care Organization (NHPCO) 2012. NHPCO facts and figures: Hospice care in America 2012 edition [Internet]. Alexandria VA: National Hospice and Palliative Care Organization; Available from: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf
- [Google Scholar]
- American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165:277-304.
- [Google Scholar]
- An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733-48.
- [Google Scholar]
- New grading of level of disordered consiousness (author's transl) No Shinkei Geka. 1974;2:623-7.
- [Google Scholar]
- Specialist palliative care is more than drugs: A retrospective study of ILD patients. Lung. 2012;190:215-20.
- [Google Scholar]
- Palliating Dyspnea for Patients with Cancer. Available from: http://www.meetinglibrary.asco.org/sites/meetinglibrary.asco.org/files/Educational%20Book/PDF%20Files/2009/09edbk.patientcare. 03.pdf
- Cyclosporin A in the treatment of acute exacerbation of idiopathic pulmonary fibrosis. Intern Med. 2010;49:109-15.
- [Google Scholar]
- Procalcitonin-guided antibiotic use in acute exacerbations of idiopathic pulmonary fibrosis. Int J Med Sci. 2013;10:903-7.
- [Google Scholar]
- Paraneoplastic coma and acquired central alveolar hypoventilation as a manifestation of brainstem encephalitis in a patient with ANNA-1 antibody and small-cell lung cancer. Neurocrit Care. 2006;4:137-9.
- [Google Scholar]
- Clinical analysis of meningeal carcinomatosis associated with primary lung cancer: Significance of intrathecal chemotherapy. Jpn J Lung Cancer. 2008;48:688-92.
- [Google Scholar]
- Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352:373-9.
- [Google Scholar]
- Diagnosis and management of hyponatremia in cancer patients. Support Care Cancer. 2007;15:1341-7.
- [Google Scholar]
- A systematic review of the use of opioids in the management of dyspnoea. Thorax. 2002;57:939-44.
- [Google Scholar]
- Palliaton of respiratory symptoms. In: Oxford Textbook of Palliative Medicine. New York: Oxford University Press; 1998. p. :583-616.
- [Google Scholar]
- The effects of morphine on dyspnea and ventilatory function in elderly patients with advanced cancer: A randomized double-blind controlled trial. Ann Oncol. 1999;10:1511-4.
- [Google Scholar]
- Effect of intraoral and subcutaneous morphine on dyspnea at rest in terminal patients with primary lung cancer or lung metastases. J Opioid Manag. 2013;9:269-74.
- [Google Scholar]
- Low dose diamorphine reduces breathlessness without causing a fall in oxygen saturation in elderly patients with end-stage idiopathic pulmonary fibrosis. Palliat Med. 2005;19:128-30.
- [Google Scholar]
- Low-dose nebulized morphine does not improve exercise in interstitial lung disease. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1940-5.
- [Google Scholar]
- Midazolam as adjunct therapy to morphine in the alleviation of severe dyspnea perception in patients with advanced cancer. J Pain Symptom Manage. 2006;31:38-47.
- [Google Scholar]
- Benzodiazepines for the relief of breathlessness in advanced malignant and non-malignant diseases in adults. Cochrane Database Syst Rev. 2010; (1):CD007354.
- [Google Scholar]
- Epidemiologic survey of Japanese patients with idiopathic pulmonary fibrosis and investigation of ethnic differences. Am J Respir Crit Care Med. 2014;190:773-9.
- [Google Scholar]
- Prediction of outcome after acute exacerbation of idiopathic interstitial pneumonia. Jpn J Thorac Dis. 1997;35:746-54.
- [Google Scholar]
- Effects of corticosteroid pulse treatment on outcomes in acute exacerbations of idiopathic interstitial pneumonia. Jpn J Thorac Dis. 1997;35:9-15.
- [Google Scholar]






