Translate this page into:
Unilobar Versus Bilobar Biliary Drainage: Effect on Quality of Life and Bilirubin Level Reduction
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Percutaneous biliary drainage is an accepted palliative treatment for malignant biliary obstruction.
Purpose:
To assess the effect on quality of life (QOL) and bilirubin level reduction in patients with inoperable malignant biliary obstruction treated by unilobar or bilobar percutaneous transhepatic biliary drainage (PTBD).
Materials and Methods:
Over a period of 2 years, 49 patients (age range, 22–75 years) of inoperable malignant biliary obstruction were treated by PTBD. Technical and clinical success rates, QOL, patency rates, survival rates, and complications were recorded. Clinical success rates, QOL, and bilirubin reduction were compared in patients treated with complete (n = 21) versus partial (n = 28) liver parenchyma drainage. QOL before and 1 month after biliary drainage were analyzed retrospectively between these two groups.
Results:
Biliary drainage was successful in all 49 patients, with an overall significant reduction of the postintervention bilirubin levels (P < 0.001) resulting in overall clinical success rate of 89.97%. Clinical success rates were similar in patients treated with whole-liver drainage versus partial-liver drainage. Mean serum bilirubin level before PTBD was 19.85 mg/dl and after the procedure at 1 month was 6.02 mg/dl. The mean baseline functional score was 39.35, symptom scale score was 59.55, and global health score was 27.45. At 1 month, mean functional score was 61.25, symptom scale score was 36.0 4, and global health score was 56.33, with overall significant improvement in QOL (<0.001). There was a statistically significant difference in the improvement of the QOL scores (P = 0.002), among patients who achieved clinical success, compared with those patients who did not achieve clinical success at 1 month. We did not find any significant difference in the QOL scores in patients according to the amount of liver drained (unilateral or bilateral drainage), the type of internalization used (ring biliary or stent). Overall, minor and major complications rates were 14.3% and 8.1%, respectively.
Conclusion:
Percutaneous biliary drainage provides good palliation of malignant obstructive jaundice. Partial-liver drainage achieved results as good as those after complete liver drainage with significant improvements in QOL and reduction of the bilirubin level.
Keywords
Biliary drainage
Bilirubin
Malignant biliary obstruction
Quality of life
Survival
INTRODUCTION
Malignant stricture of the biliary tree is one of the common causes of obstructive jaundice.[1] There are various causes of malignant biliary obstruction such as gallbladder cancer (GBC), cholangiocarcinoma, pancreatic cancer, periampullary carcinoma, metastatic lymphadenopathy, and rarely hepatocellular carcinoma. The most common cause in our country is carcinoma of the gallbladder.[2]
Most patients with GBC and obstructive jaundice are not amenable to a curative surgical resection due to advanced disease at the time of diagnosis (locally advanced, vascular invasion, and metastasis), and hence, effective palliation is the goal of treatment.[34]
Although surgical bilioenteric bypass has been the traditional palliative approach; however, it is associated with considerable morbidity and mortality. Therefore, there was a need for minimally invasive and clinically satisfying procedure to replace the more morbid surgical procedures. Substantial advances in endoscopic and percutaneous therapies to palliate patients with biliary malignancies have been made since the introduction of the first percutaneous transhepatic biliary drainage (PTBD) procedure.[567]
During the last decade, percutaneous transhepatic insertion of metallic stents has become a firmly established palliative method for the relief of malignant biliary obstruction. Successful biliary drainage alleviates jaundice, improves liver function, and has a positive impact on quality of life (QOL).[8]
It has been shown that even if only 30% of the liver parenchyma is drained, it provides adequate palliation to relieve jaundice and associated pruritus.[910] Therefore, unilateral drainage of one lobe of the liver might be sufficient to palliate jaundice and pruritus and improve the QOL,[1011121314] though there is no doubt that the drainage of both liver lobes is technically more challenging to accomplish than drainage of a single system with an increased risk of procedure-related complications and mortality.[9], 1215 ,[1617]
We undertook this prospective study to evaluate the effect of PTBD in patients with malignant obstructive jaundice in terms of QOL and percentage reduction of bilirubin level. The secondary endpoint was to evaluate the technical and clinical success of the procedure, and the complications. We also analyzed retrospectively the effect of partial versus complete liver parenchyma drainage on QOL and bilirubin reduction level.
MATERIALS AND METHODS
Patient population
From October 2007 to May 2009, a total of 49 (20 men and 29 women, with a mean age of 48.1 years) with malignant obstructive jaundice, who had unresectable disease, were recruited according to the inclusion and exclusion criteria. The Institutional Ethics Committee approved the study protocol.
Inclusion criteria
-
Confirmed diagnosis of malignant obstructive jaundice
-
Surgically unresectable
-
Maximum Eastern Cooperative Oncology Group (ECOG) performance status up to two.[18]
Exclusion criteria
-
Refusal to participate in the study
-
Patients with massive ascites
-
Patients with bleeding diathesis.
Clinical workup
A detailed clinical history was obtained in all patients with particular reference to abdominal pain, pruritus, fever, anorexia, weight loss, and duration of symptoms. The patients underwent QOL assessment as well as performance status assessment using the European Organisation for Research and Treatment of Cancer QOL questionnaire version 3.0, based on 30 questions (EORTC QLQ-C30)[19] and ECOG performance status scale,[18] respectively.
Investigations
Laboratory investigations
All patients were subjected to the following investigations:
-
Liver function tests (LFTs) (total bilirubin, direct bilirubin, indirect bilirubin, alanine transferase, aspartate transferase, alkaline phosphatase, and total protein)
-
Coagulation profile – prothrombin time.
Imaging
All patients were evaluated with ultrasonography (USG) and either dual phase computed tomography and/or magnetic resonance imaging with magnetic resonance cholangiopancreaticography.
Images were analyzed for:
-
Cause of obstruction (gallbladder carcinoma, cholangiocarcinoma, pancreatic/periampullary carcinoma, recurrent/postcholecystectomy GBC, and peri portal nodes) [Figure 1]. The recurrent/postcholecystectomy group contains two sets of patients, one, who had been operated for GBC, now presented with recurrent mass with locally advanced disease. Second, who underwent cholecystectomy for stone disease, but histology revealed carcinoma gallbladder, but they had locally advanced disease when presented to us
-
Level of obstruction whether hilar or nonhilar obstruction
-
Criteria for unresectability. The criteria used for unresectability were those as described by Kumaran et al.:[3] Distant metastasis (liver, peritoneum, and lymph nodes), extensive local contiguous organ spread (liver, duodenum, pancreas, or hepatic flexure), contiguous involvement of greater than two segments each in both lobes of the liver, involvement of secondary biliary confluence of both lobes of liver, tumoral invasion of main portal vein or proper hepatic artery or simultaneous invasion of one side hepatic artery and the other side portal vein or simultaneous involvement of ipsilateral hepatic artery, and/or portal vein along with contralateral secondary confluence of bile ducts [Figure 1].

- Axial computed tomography images showing spectrum of malignant biliary obstruction: (a) Mass replacing gallbladder (arrow) with encasement of hepatic artery, a case of carcinoma gallbladder; (b) enhancing mass at hilum (arrow) resulting biliary dilatation, a case of cholangiocarcinoma; (c) cholangiocarcinoma with involvement of bilateral secondary biliary confluence (arrows); (d) mass in head of pancreas (arrow) with involvement of superior mesenteric artery, a case of carcinoma pancreas; (e) lymph nodal mass at porta (arrow) resulting in biliary obstruction from unknown primary; (f) carcinoma gallbladder (not shown) with lung metastases (arrows)
The diagnosis of obstructive jaundice was established on the basis of LFTs (increased serum bilirubin and alkaline phosphatase levels) and an abdominal USG showing dilated intrahepatic radicals.
The diagnosis of malignancy was established preoperatively by clinical features, imaging studies and was confirmed by either an USG guided fine needle aspiration cytology (FNAC)/trucut biopsy from mass or a positive brush cytology wherever possible. All included patients were considered unsuitable for surgical intervention either because of unresectable disease or co-morbid conditions, which precluded surgery.
After the clinical, laboratory, and radiological investigations were completed, patients were offered the option of PTBD as a palliative method of treatment. Patients were informed about the procedure and related complications in detail and written informed consent was obtained.
Procedure
The procedures were performed with USG and fluoroscopic guidance, using digital subtraction angiography machine (Allura Xpera, Philips, The Netherlands); the procedure was performed under local anesthesia with conscious sedation with close monitoring of vitals. All patients received injectable prophylactic antibiotic (cefoperazone + sulbactam 1 g) for 72 h starting 2 h before the procedure, followed by oral antibiotics (ciplo × 500 mg BD) for 3 days (total 6 days). Patients were kept nil by mouth for 4–6 h before the procedure and were well-hydrated with intravenous fluids.
The appropriate puncture site was chosen based on the status of primary confluence, secondary confluence and atrophy of liver parenchyma. Patients with extensive right-sided disease and/or right lobe atrophy with sparing of the left lobe were subjected to a left-sided approach and vice versa. For Bismuth type II blocks, either the right or left system was chosen (left was chosen if the left lobe of the liver was not atrophied, as it is technically easier for the radiologist performing the procedure and is also comfortable for the patient. However, it has the disadvantage of prolonged exposure of radiation to the operator's hands). An anterior subxiphoid approach was used for the left duct, whereas a right lateral intercostal approach was used for the right duct. Finally, either a metal stent/internal-external drainage plastic tube/was placed across the stricture site to provide internal drainage. All the patients were called 2 days after internalization for check cholangiogram, either through access catheter or through ring biliary catheter, to check for free flow of contrast into the duodenum across the stricture and to look for the stent expansion.
Postprocedure care
After the completion of the procedure, the patients were kept under observation in the clinical department for 1 day and closely followed for any immediate procedure-related major or minor complications.
Follow-up
After the placement of catheter/stent and if there was no major complication during observation, the patient was discharged and called for check cholangiogram after 2 days and then for regular follow-up at 1 week, 1 and 6 months. Follow-up of each patient was based on outpatient examinations and telephone interviews. LFT was done at each visit. Complete follow-up was available in all patients till the end of 6 months after the procedure, or till they succumbed to their disease, whichever occurred earlier.
Analysis
Technical success, clinical success, stent patency, survival, QOL, and complication rates were recorded.
Technical success
Technical success was defined as the successful deployment of the stent/internal-external drainage tube in the appropriate position resulting in drainage of the respective bile ducts.
Clinical success
Clinical success was defined by a decrease in serum bilirubin level of more than 20% relative to baseline within 1 week after stent insertion. Percent reduction in serum bilirubin level relative to baseline was calculated for each patient.
Stent/catheter patency
Stent/catheter patency period was defined as the interval between stent placement and obstructive jaundice recurrence. Stent/Catheter block was diagnosed if there was the reappearance of jaundice after it had subsided.
It was confirmed by one of the following:
-
Cholangiography, USG, or CT demonstration of redilatation of bile duct
-
Increase in total serum bilirubin concentration by 1 mg/dl from the preceding value
-
Cholangitis.
The stent/catheter was considered patent if there was no increase in the serum bilirubin levels and no dilatation of the intrahepatic bile ducts depicted in imaging.
If stent/catheter occlusion did not occur during a patient's lifetime, the patency was considered equal to the period of survival.
Survival
Survival (in days) was calculated from the day of intervention until death or last follow-up.
Quality of life assessment
QOL was assessed by EORTC QLQ-C30 prior to the treatment and after 1-month of the treatment.
The QLQ-C30 is composed of 30 questions with a scale range from mild to severe measured on a scoring scale, and the questions are grouped together into three groups as described below.
-
Functional - 15 questions are under functional group
-
Symptomatology - 13 questions are under symptomatology group
-
Global - two questions are under global group.
Interpretation of quality of life scoring system
A high score for a functional scale represents a high/healthy level of functioning and an improvement in functional status is determined by an increase in score.
A high score for the global health status/QOL represents a high QOL and an improvement in global status is determined by an increase in score.
A high score for a symptom scale/item represents a high level of symptomatology/problems, and an improvement in symptomatology status is determined by a decrease in score.
The QOL questionnaire has been translated into Hindi and validated for use among Indian patients. The QOL was assessed at 1-month posttreatment only because the QOL was expected to improve initially only. Later many patients either expired or a decrease in their QOL could also be because of disease progression and not necessarily due to biliary obstruction (stent block). Hence, all patients were not evaluated for QOL at 6 months.
Complications were divided into major and minor categories according to the reporting standards of the Society of Interventional Radiology.
-
Major complications included sepsis or cholangitis, hemorrhage requiring blood transfusion, abscess formation, peritonitis, cholecystitis, pancreatitis, pneumothorax, pneumonia, pleural infection, sepsis, and death
-
Minor complications included pain, self-limiting hemorrhage, bilovenous fistula, subcapsular biloma, and stent/catheter migration.
Statistical analysis
The Wilcoxon signed rank test was used for comparison of noncategorical variables (pre- and post-intervention bilirubin levels). The Mann–Whitney test was used to compare the percent reduction in serum bilirubin levels between partial and complete liver drainage. The Kaplan–Meier survival curves calculated the cumulative overall survival and the primary patency rates. Univariate log rank analyses were used to evaluate potential primary patency predictors (cumulative primary patency curves were stratified by the level of biliary obstruction, ring biliary vs. stent and for whole-liver vs. partial-liver drainage). Furthermore, they were used to evaluate potential survival predictive factors (cumulative survival curves were stratified by the level of biliary obstruction, and the bilirubin levels post-intervention). All variables were studied as categorical; only the bilirubin levels after stent placement were analyzed as noncategorical. As a result, they were dichotomized and their cut-off point was based on statistical significance
(a decrease to 0.4–3.9 mg/dl post-intervention vs. a decrease to 4 mg/dl or more). The Cox proportional hazards model was used to calculate hazard ratios for all the above-mentioned variables. Life table analyses were used to calculate cumulative survival and patency rates for specific time intervals. The level of statistical significance was set at P ≤ 0.05.
RESULTS
The study included 49 patients (20 men and 29 women) with malignant obstructive jaundice, who had unresectable disease, were treated in our institution with PTBD. The mean age of the patients was 48.1 years (age range, 22–75 years).
The etiology of malignant biliary obstruction was GBC (n = 35), cholangiocarcinoma (n = 6), recurrent/postcholecystectomy GBC with direct invasion into the hepatoduodenal ligament or periportal nodes causing obstruction (n = 4), pancreatic/periampullary carcinoma (n = 2), and metastatic adenopathy from unknown primary (n = 2). Etiologies of malignant obstruction are mentioned in Table 1.

Majority of the patients had hilar obstruction (n = 33, 67.4%), depicted in Table 2.

The criteria used for unresectability were those as described by Kumaran et al.,[3] which has been described in materials and methods.
The distribution of patients according to criteria for unresectability on imaging is shown in Table 3.

Patients were considered inoperable if they met the criteria for unresectability and/or they had significant co-morbidity or any other medical condition precluding surgery. Of the 49 patients, 43 patients were referred for PTBD based on unresectability at imaging, whereas the rest six patients had resectable tumors according to imaging but were considered inoperable because of co-morbid conditions.
The diagnosis of malignancy was established preoperatively by clinical features, imaging studies and was confirmed by either a USG-guided FNAC/trucut biopsy from mass or positive brush cytology wherever possible. Patients were divided into those having patent primary confluence (n = 16, 33%) and blocked primary confluence (n = 33, 67%).
In all our patients, we followed standard protocol as per interventional guidelines. We used epigastric approach for left side system puncture, whereas right side intercostal approach for right side system. We used combined ultrasound and fluoroscopic guidance in all cases. We used unilateral approach in majority of our patients (n = 44, 89.8%), whereas bilateral approach in five patients (10.2%). In majority of the patients (n = 28, 57.1%), only one lobe was drained and in 21 patients (42.9%), bilateral drainage was achieved. We placed ring biliary catheters in 25 patients (51%), and metallic stents in 24 patients (49%), and a technical success rate was 100% [Figures 2–5].

- Fluorospot images showing unilateral biliary drainage right sided approach (a) and left side approach (b)
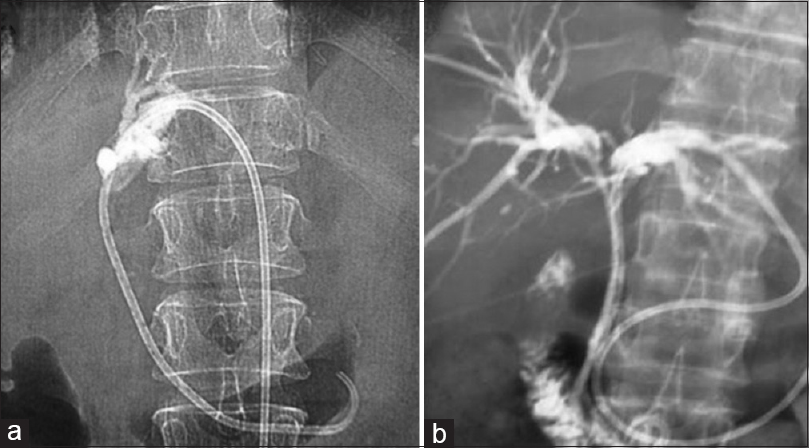
- Fluorospot images showing types of biliary drainage; unilateral biliary drainage (a) and bilateral biliary drainage (b)
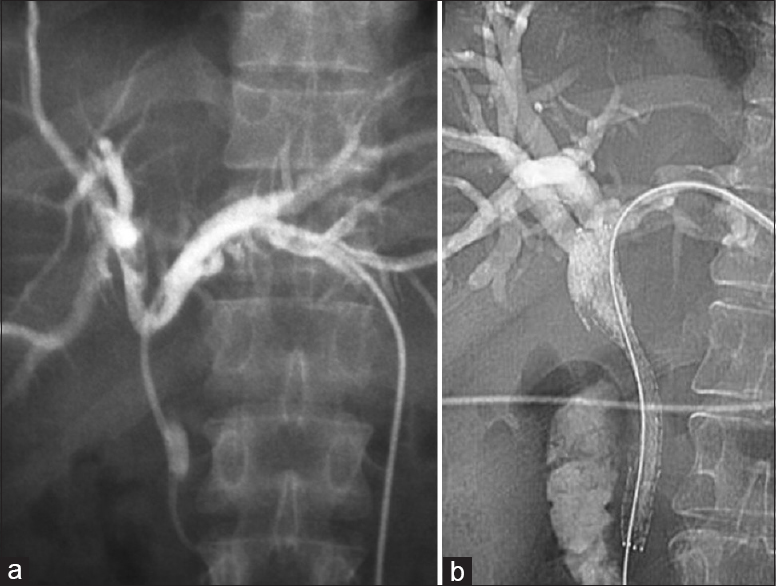
- Fluorospot images showing types of internalization of biliary drainage; Internalization done by ring biliary catheter (a) and internalization done by self-expandable metallic stenting (b)

- Fluorospot images showing types of metallic stenting; unilateral metallic stenting (a) and Y-shaped bilateral metallic stenting (b)
Clinical success
Complete follow-up was available in all 49 patients at 1 month, and 10 patients expired within 1 month either due to disease progression or co-morbid conditions. Among 10 patients who died, the latest bilirubin levels were available for six patients, just before death and so these values were recorded as 1-month follow-up. Hence, a total of 45 patients were analyzed at 1 month.
Serum bilirubin levels were measured before and after treatment. The pre-interventional values and the final post-interventional values at 1 month were recorded. Mean serum bilirubin level before PTBD was 19.85 mg/dl (range 1.2–42.8 mg/dl) and after the procedure at 1 month was 6.02 mg/dl (range 0.5–30.4 mg/dl). The mean difference in total bilirubin was 13.8 mg/dl, and the percentage reduction of total bilirubin level was 69.4% from the baseline total bilirubin level. There was a significant difference in the pre- and post-intervention bilirubin levels (Wilcoxon signed rank test, (P < 0.001). The overall clinical success rate was 89.97%. Biliary drainage was clinically unsuccessful in only five cases (11.1%): An increase in postintervention bilirubin level was noted in three patients and a minimal reduction in the other two patients.
We retrospectively analyzed bilirubin reduction between whole-liver drainage and partial-liver drainage and results are mentioned in Table 4.

We investigated if there was any difference in the clinical success rate in patients treated with partial (n = 29) versus bilateral drainage (n = 16) and found that there was no significant difference in the reduction of the serum bilirubin levels between the two groups (P = 0.136).
We also investigated the presence of differences in the clinical success rate in patients with various types of internal drainage; ring biliary catheter (n = 21) versus metallic stent (n = 24). There was no significant difference in the reduction of the serum bilirubin levels between the two groups (P = 0.345).
The difference in the clinical success rate was also studied in patients with hilar (n = 15) and nonhilar (n = 30) blocks. There was no significant difference in the reduction of the serum bilirubin levels between the two groups (P = 0.138).
Patients were stratified according to the post procedure bilirubin level into two groups (serum bilirubin <4 mg/dl vs. 4 mg/dl or more), for the purpose of analysis of patency rates and survival rates. The distribution of patients according to the absolute bilirubin levels at 1 month is shown in Table 5.

Quality of life
Of the 10 patients who died, the latest QOL scores were available for three of these patients, just before death and so these values were recorded as a 1-month follow-up. Hence, the QOL scores were calculated for 42 patients at 1-month follow-up. The preinterventional values and the final postinterventional values were recorded. There was an improvement in all the QOL parameters, which was statistically significant (P < 0.001). Pre- and post-PTBD QOL values are depicted in Table 6.
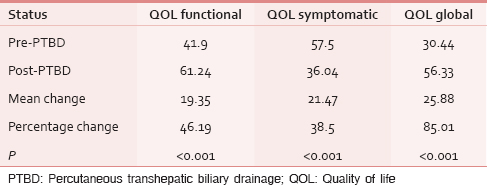
We retrospectively studied the impact of the following factors on the change in the QOL scores and found the following results:
-
Partial-liver drainage (n = 27) versus whole-liver drainage (n = 15). Functional QOL scores (P = 0.863), symptomatic QOL scores (P = 0.51), or global QOL scores (P = 0.472)
-
Ring biliary catheter (n = 19) versus stent (n = 23). Functional QOL scores (P = 0.07), symptomatic QOL scores (P = 0.39), or global QOL scores (P = 0.118)
-
Hilar (n = 14) and nonhilar (n = 28) blocks. Functional QOL scores (P = 0.07), symptomatic QOL scores (P = 0.39), or global QOL scores (P = 0.118).
We did not find any statistically significant difference in the QOL scores in patients stratified according to the amount of liver drained (partial- vs. whole-liver drainage), the type of internalization used (ring biliary or stent) or the patency of the primary confluence.
Relationship between quality of life and bilirubin level reduction
We investigated the difference in the QOL scores between the group who achieved clinical success and who did not achieve clinical success. There was a statistically significant difference in the improvement of the QOL scores (P = 0.002) between the two groups. This shows that significant reduction in bilirubin level was related to significant improvement in QOL. The graph showing this relation is shown in Graph 1.

- Relation of quality of life with improvement in bilirubin at 1 month. (Key: X-axis: Percentage change in bilirubin level at 1 month. Y-axis: Quality of life change at 1 month)
PATENCY AND SURVIVAL RESULTS WITH STATISTICAL ANALYSIS
Catheter/stent patency
Technical success was achieved in all patients (100%), as already stated. Mean patency was calculated in all patients in days. Mean primary patency was 113.2 days (range 2–445 days). Cumulative primary patency rates at 1, 3, and 6 months were 91.8%, 85.7%, and 81.6%, respectively. Distribution of patency rates is mentioned in Table 7.

Eight patients developed catheter occlusion in the total duration of 6 months (16.3%). Time to occlusion ranged between 10 and 135 days (mean 52.6 days). All occlusions were managed conservatively. None of the patients underwent re-intervention. All these patients subsequently expired.
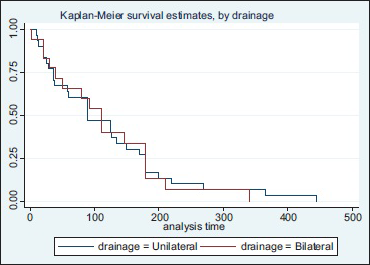
Comparison of patency rates between whole-liver (bilateral) drainage versus partial-liver (unilateral) drainage
There was no significant difference in the patency rates between the two groups. The median patency in patients with unilateral drainage was 90 days, and the median patency in patients with bilateral drainage was 110 days, which was statistically not significant (log-rank test, P = 0.9365). This analysis is shown in Graph 2.
- Cumulative patency stratified according to biliary drainage
Comparison of patency rates among patients treated with the different types of internalization (metallic stent vs. ring biliary catheter)
The median patency in patients with ring biliary drainage was 50 days, and the median patency in patients with stent drainage was 147 days, which was statistically significant (log-rank test, P = 0.007). This analysis is shown in Graph 3.
- Cumulative patency stratified according to internalization procedure
Relationship between patency rates and amount of bilirubin level reduction
In patients with serum bilirubin <4 mg/dl, the mean overall patency was 150.2 days, whereas in patients with serum bilirubin >4 mg/dl, the mean overall patency was 79.89 days with a mean difference of 70.1 days, which was statistically significant (P < 0.001). The Kaplan–Meier curve is shown in Graph 4.

- Patency stratified according to 1 month bilirubin level (Key to Kaplan–Meier graphs: X-axis: Postpercutaneous transhepatic biliary drainage interval in days. Y-axis: Probability of survival)
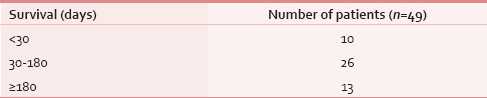
Patient survival
Forty-three patients died during the course of the study; details are mentioned in Table 8. The estimated mean length of survival for the entire patient population was 116.8 days (range 2–445 days). Calculated median survival was 90 days.
Relationship between survival rates and amount of bilirubin level reduction
In the 27 patients (60%) with post-stenting bilirubin levels of < 4 mg/dl at 1 month, mean overall survival was 151.78 days (range 37–445 days). In the remaining 18 patients (40%) with post-stenting bilirubin levels >4 mg/dl, mean overall survival was 85.28 days (range 10–365 days). Univariate Kaplan–Meier (log rank) survival analysis revealed a statistically significant difference in the survival rate when patients were stratified according to the post-stenting bilirubin levels (serum bilirubin < 4 mg/dl vs. >4 mg/dl) (P = 0.007). The graph is depicted in Graph 5.

- Cumulative survival stratified according to bilirubin levels at 1 month (Key to Kaplan–Meier graphs: X-axis: Postpercutaneous transhepatic biliary drainage interval in days. Y-axis: Probability of survival)
Comparison of survival rates between whole-liver (bilateral) drainage versus partial-liver (unilateral) drainage
There was no significant difference in survival rates between the two groups (log-rank test, P = 0.813). The Kaplan–Meier curve is shown in Graph 6.

- Cumulative survival stratified according to biliary drainage
Comparison of survival rates among patients treated with the different types of internalization (metallic stent vs. ring biliary catheter)
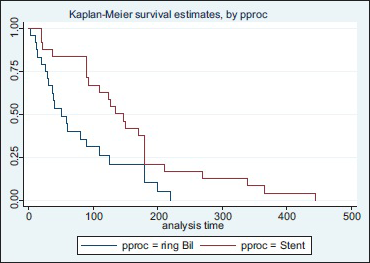
The median survival in patients with ring biliary catheter was 50 days, and the median survival in patients with stent was 135 days, which was statistically significant (log-rank test, P = 0.018). This analysis is shown in Graph 7.

- Cumulative survival stratified according to internalization
Complications
Minor complications occurred in seven patients (14.3%). They included mild hemorrhage in three patients; transient blood tinged bile in two patients and ileus in two patients. Major complications were divided into immediate and late. Immediate major complications were defined as those occurring on the same day of the procedure. No immediate major complications in the form of hemorrhage requiring a blood transfusion, shock, or procedure related death were observed in our study. Later major complications occurred in four patients (8.1%). In all the patients, complications developed 2–3 days after the procedure: All four patients developed severe sepsis leading to death, and they were all caused by severe cholangitis, not responding to antibiotics.
DISCUSSION
Malignant obstructive jaundice is a common clinical problem and can occur due to variety of causes as described earlier.[1] GBC is the most common cause of malignant biliary obstruction in our country. Most of these patients present with obstructive jaundice caused by biliary obstruction.[20] As majority of the patients are not candidates for curative resection, the therapeutic goal is often palliative, given the short life expectancy. PTBD is a well-established procedure used in patients with malignant biliary obstruction for decompression of intra- and extra-hepatic bile ducts.[2122] Successful biliary drainage alleviates jaundice, improves liver function, and has a positive impact on QOL.[8]
In our study, most frequent diagnosis was GBC (n = 35), followed by cholangiocarcinoma (n = 6), recurrent/postcholecystectomy GBC with direct invasion into the hepatoduodenal ligament or periportal nodes causing obstruction (n = 4), pancreatic/periampullary carcinoma (n = 2), and metastatic adenopathy from unknown primary (n = 2). The causes were different from those seen in Western literature where the majority were cancers causing low biliary obstruction such as cholangiocarcinoma or pancreatic carcinoma. Gallbladder carcinoma is relatively rare in Western countries. In the study conducted by Brountzos et al., they reported 76 patients of malignant biliary obstruction, in which 37% were cholangiocarcinoma, 22% were pancreatic carcinoma. Moreover, only 9% had gallbladder carcinoma.[21]
In our study, most common reason for unresectability was locally advanced disease, which was seen in 37 patients (75.55%).
We used unilateral approach in majority of our patients (89.8%), whereas bilateral approach was used in 10.2% patients in our study. The bilateral approach was used in those patients with blocked confluence, in whom the contralateral ducts were inadvertently opacified during cholangiography, as these patients were at high risk of cholangitis if left undrained.
Brountzos et al. also reported using unilateral stents in 92% and bilateral stents in 8% of patients with blocked primary confluence, which was similar to our study.[21] In the study reported by Qian et al., 233 patients received biliary catheters/stents, out of which bilateral stents were inserted in 7% of patients and unilateral stents in 93% of patients.[23]
In our study, in the majority of the patients, only one lobe was drained (n = 28, 57.1%) and in 42.9% patient bilateral drainage was achieved. In the study reported by Brountzos et al.,[21] the majority (54%) had whole-liver (bilateral) drainage. This too appears to be due to the relatively high incidence of tumors causing low bile duct obstruction, in which case even single stent caused whole-liver drainage. In the study reported by Saluja et al.,[24] all patients received unilateral drainage and there was no patient with bilateral drainage, as the primary confluence was blocked in all patients.
In our study, we placed ring biliary catheters in 25 patients (51%) and stents in 24 patients (49%). The decision of placing either ring biliary or stent was purely based on affordability of the patient. Previous studies have reported results using stents, but not ring biliary catheters.
To conclude in our study, the majority of patients had a “high” obstruction involving the primary confluence and hence there was unilateral drainage in the majority of the patients. There was almost equal division of patients receiving ring biliary catheter and metallic stents.
Catheter/Stent placement was successful in all patients (100%), which is similar to the reports of previously published studies.[2125] In the study reported by Saluja et al.,[24] the technical success achieved was 93%, in the PTBD group, whereas it was 82% in the endoscopic stenting group. In the study reported by Han et al.,[26] the technical success was 95%.
In our study, major complications occurred in 8.1% patients and minor complications in 14.3% patients. In the literature, rates of minor and major complications range between 8% and 23% and between 2% and 20%, respectively,[222728] which are in concordance with the results of our study. In the study reported by Kaskarelis et al.,[29] early complications rate within the first 30 days was 2% and the late complications rate was 16%.
The secondary endpoint of the present study was an evaluation serum bilirubin level in the pre-procedure and post-procedure period.
In our series, a significant reduction in the post-intervention bilirubin levels relative to baseline was achieved, with clinical success rates of 89.97% and an increase in post-intervention bilirubin levels was noticed in only five cases at 1 month. Laméris et al.[30] reported a similar percentage of patients with no obvious bilirubin decrease (6–7.5%), attributable to either extensive liver failure or advanced liver metastases.[30] In the study conducted by Brountzos et al.,[21] they reported an overall clinical success rate of 97.3% and stent implantation did not result in clinical success in only two cases (2.7%).
There was no significant difference in the reduction of the serum bilirubin levels between patients stratified according to unilateral versus bilateral drainage, hilar and nonhilar obstruction, ring biliary catheter, and stent. In the study conducted by Brountzos et al.,[21] their results also showed similarity with ours, as the serum bilirubin levels were similar in patients stratified according to unilateral versus bilateral drainage, in their study.
The pre-interventional values and the final post-interventional values according to EORTC QLQ-30 at 1 month were recorded. There was a significant improvement in all the QOL parameters; functional, survival, and global.
We investigated the presence of differences in the QOL scores in patients at 1 month, who achieved clinical success (n = 40), compared with those patients who did not achieve clinical success (n = 5). The percentage reduction in bilirubin level in the group that achieved clinical success was 76%, whereas there was a 29.8% increase in the bilirubin level in the group that did not achieve clinical success. There was a statistically significant difference in the improvement of the QOL score (P = 0.002), between the two groups. This showed that significant improvement in QOL was related to effective biliary drainage. In the study reported by Abraham et al.,[31] among the 26 patients, improvement in bilirubin level was documented in 84% of patients and was associated with significant improvements in social function and mental health, which was supported by the results of our study.
We did not calculate improvements in individual symptom scores, as done in previous studies,[24313233] because we did not intend to identify individual factors, which improved after biliary drainage, as it was not our objective. Rather, our aim was to assess the overall improvements in the different domains of QOL after successful biliary drainage.
In our study, the mean primary patency was 113.2 days (range 2–445 days). Cumulative primary patency rates at 1, 3, and 6 months were 91.8%, 85.7%, and 81.6%, respectively. Eight patients developed catheter occlusion in the total duration of 6 months (16.3%). Time to occlusion ranged between 10 and 135 days (mean 52.6 days). All occlusions were managed conservatively. In our series, we did not consider restenting of occluded stents, because of following reasons:
-
These patients (stent occluded) presented with rising bilirubin only
-
They had no pruritus or cholangitis
-
These patient's QOL had deteriorated and the expected survival of the patients was less
-
The procedure related complications rate would be higher than the clinical benefit.
Hence, we decided (as a team) not to restent these patients and managed conservatively, based on overall clinical scenario.
In the study conducted by Brountzos et al.,[21] mean overall primary stent patency was 120.3 days, whereas the restenosis rate was 12%. In cases of stent occlusion, they had reinserted stents and thus calculated the secondary patency, which was 242.2 days. As we had not reinserted stents in the patients who came with blocks, we could not calculate the secondary patency rates. In the study reported by Saluja et al.,[24] the mean stent patency time was 140 days in the PTBD group, and the stent occlusion was 32%, which is higher than that seen in our study. Han et al.[26] reported stent occlusion rate of 26% and mean patent period of 280 days. In the study conducted by Ho and Voss,[34] the median duration of stent patency was 10 months.
Although the majority of our patients had hilar lesions (n = 33), we performed mainly unilateral drainage. There is universal agreement that nonhilar lesions and Bismuth type I lesions should be treated with placement of a single stent. There is, however, considerable debate regarding drainage of Bismuth types II–IV hilar lesions: Some advocate bilateral drainage at the outset,[7] whereas others support the unilateral drainage of the larger, disease-free liver lobe, in nonseptic patients. We adopted the latter strategy in our study. Our goal was to drain sufficient liver parenchyma to achieve adequate palliation while maintaining the minimal invasiveness of the procedure. It is believed that adequate palliation can be obtained by draining only 30% of the liver.[91035]
Our results did not show any difference in the reduction in serum bilirubin or patency rates between the two patient groups. Inal et al. in a study comparing unilateral versus bilateral drainage in patients with hilar obstruction reported that there was no difference in the patency rates between the two strategies in Bismuth types II and III lesions; only patients with Bismuth type IV lesions benefit from bilateral stenting.[36]
Patency rates showed a significant difference among patients treated with the different types of internalization: Either stent or ring biliary catheter was used (147 vs. 50 days). We believe the reason for increased patency rates of stents could be due to the larger lumen diameter as compared to ring biliary catheters. In addition, there are less chances of stent getting infected compared to ring biliary catheters, as they are not exposed to the environment and surroundings, thereby lessening the chances of blockage with infected debris or pus. In addition, the ring-biliary catheters are internal-external catheters; they have a chance of accidental removal.
In the present study, we evaluated potential predictors of survival such as serum bilirubin, the level of biliary obstruction, and the method of liver parenchyma drainage (whole vs. partial). Such factors have also been studied previously with controversial results.[2122273738] According to our results, whenever the post-PTBD serum bilirubin level drops below 4 mg/dl the patient will survive longer. Moreover, we found that the bilirubin cut-off point represents an independent survival predictor, as shown by multivariate analysis, independent of whether the liver parenchyma was completely or partially drained, or level of obstruction. Brountzos et al. concluded in their study that the post-intervention serum bilirubin level was an independent predictor of survival (P < 0.001).[21]
We could not assess if PTBD has any effect on prolongation of survival as there was no control group in our study. However, mean survival duration was found to be similar to previously reported studies.[2225]
Limitations of the study
-
It is a retrospective analysis of prospective collected data. We could not prospectively implement partial versus complete liver parenchymal drainage
-
There was no control group available for comparing this invasive palliative technique, and a single cohort of patient was studied and followed up for improvement in bilirubin levels, QOL scores, patency, and survival. This has already been accepted as a standard procedure for palliation for inoperable malignant obstructive jaundice; hence, having a control group with no intervention meant denying patients the appropriate therapy
-
We did not categorize our patients according to the classification of malignant biliary strictures described by Bismuth. Hence, we could not investigate the presence of differences in the clinical success rates, QOL, patency, and survival among patients with different Bismuth categories
-
We did not calculate improvements in individual symptom scores in QOL assessment. Hence, we could not identify potential symptomatic predictors of good or poor QOL and the effect of PTBD on individual symptoms.
CONCLUSION
A novel point of our study is that we have evaluated the factors affecting the patency and survival in a study group comprising primarily of gallbladder carcinoma patients. Our results show that even though the survival of patients with GBC is dismal and almost all patients succumb to their illness, the QOL can be enhanced significantly in these patients by subjecting to biliary drainage, and the prognosis (survival) can be predicted by recording the 1-month post-procedure bilirubin level. Also, PTBD causes a significant reduction in the bilirubin level and improvement in QOL, irrespective of the level of the block, the amount of liver drained or the type of internalization (ring biliary or stent).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Approach to the patient who has suspected acute bacterial cholangitis. Gastroenterol Clin North Am. 2006;35:409-23.
- [Google Scholar]
- Epidemiology of digestive cancers in India. I. General principles and esophageal cancer Indian. J Gastroenterol. 1997;16:98-102.
- [Google Scholar]
- The role of dual-phase helical CT in assessing resectability of carcinoma of the gallbladder. Eur Radiol. 2002;12:1993-9.
- [Google Scholar]
- Resection or palliation: Priority of surgery in the treatment of hilar cancer. World J Surg. 1988;12:39-47.
- [Google Scholar]
- Malignant biliary obstruction: Treatment with self-expandable stainless steel endoprosthesis. Cardiovasc Intervent Radiol. 1992;15:351-5.
- [Google Scholar]
- Relief of obstructive jaundice through percutaneous transhepatic catheter: A new therapeutic method. AJR Am J Roentgenol. 1974;122:356-67.
- [Google Scholar]
- Metallic stents for the treatment of biliary obstruction: A report of 100 cases. Cardiovasc Intervent Radiol. 1992;15:367-74.
- [Google Scholar]
- Quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. J Vasc Interv Radiol. 2003;14(9 Pt 2):S243-6.
- [Google Scholar]
- Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut. 1991;32:685-9.
- [Google Scholar]
- Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: Results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001;53:547-53.
- [Google Scholar]
- Endoscopic drainage of malignant hilar obstruction: Is one biliary stent enough or should we work to place two? Gastrointest Endosc. 2001;53:681-4.
- [Google Scholar]
- Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354-62.
- [Google Scholar]
- Endoscopic single versus double (bilateral) wallstents for palliation of malignant Bismuth type III/IV hilar strictures: Comparison of clinical outcomes and costs (abstract) Gastrointest Endosc. 1999;49:AB234.
- [Google Scholar]
- Unilateral placement of metallic stents for malignant hilar obstruction: A prospective study. Gastrointest Endosc. 2003;58:50-3.
- [Google Scholar]
- Biliary endoprostheses in tumors at the hepatic duct bifurcation. Eur J Radiol. 1986;6:275-9.
- [Google Scholar]
- A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy. 1989;21:266-71.
- [Google Scholar]
- Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc. 1988;34:95-101.
- [Google Scholar]
- Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-55.
- [Google Scholar]
- The European organization for research and treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-76.
- [Google Scholar]
- One-step palliative treatment method for obstructive jaundice caused by unresectable malignancies by percutaneous transhepatic insertion of an expandable metallic stent. World J Gastroenterol. 2006;12:2423-6.
- [Google Scholar]
- A survival analysis of patients with malignant biliary strictures treated by percutaneous metallic stenting. Cardiovasc Intervent Radiol. 2007;30:66-73.
- [Google Scholar]
- Percutaneous biliary metal wall stenting in malignant obstructive jaundice. Eur J Gastroenterol Hepatol. 2003;15:915-9.
- [Google Scholar]
- Treatment of malignant biliary obstruction by combined percutaneous transhepatic biliary drainage with local tumor treatment. World J Gastroenterol. 2006;12:331-5.
- [Google Scholar]
- Endoscopic or percutaneous biliary drainage for gallbladder cancer: A randomized trial and quality of life assessment. Clin Gastroenterol Hepatol. 2008;6:944-950.e3.
- [Google Scholar]
- Palliation of malignant biliary and duodenal obstruction with combined metallic stenting. Cardiovasc Intervent Radiol. 2007;30:1173-7.
- [Google Scholar]
- Percutaneous insertion of Zilver stent in malignant biliary obstruction. Abdom Imaging. 2006;31:433-8.
- [Google Scholar]
- Percutaneous self-expandable uncovered metallic stents in malignant biliary obstruction. Complications, follow-up and reintervention in 154 patients. Acta Radiol. 2003;44:139-46.
- [Google Scholar]
- Predicting early mortality following percutaneous stent insertion for malignant biliary obstruction: A multivariate risk factor analysis. Eur J Gastroenterol Hepatol. 2000;12:1095-100.
- [Google Scholar]
- Long-term follow-up in patients with malignant biliary obstruction after percutaneous placement of uncovered wallstent endoprostheses. Acta Radiol. 1999;40:528-33.
- [Google Scholar]
- Malignant biliary obstruction: Percutaneous use of self-expandable stents. Radiology. 1991;179:703-7.
- [Google Scholar]
- Palliation of malignant biliary obstruction: A prospective trial examining impact on quality of life. Gastrointest Endosc. 2002;56:835-41.
- [Google Scholar]
- Symptom relief and quality of life after stenting for malignant bile duct obstruction. Gut. 1994;35:467-70.
- [Google Scholar]
- Quality of life in patients stented for malignant biliary obstructions. Eur J Gastroenterol Hepatol. 1997;9:481-4.
- [Google Scholar]
- Self-expandable metallic biliary stents with permanent access. AJR Am J Roentgenol. 2005;184:410-4.
- [Google Scholar]
- Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: Unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003;14:1409-16.
- [Google Scholar]
- Treatment of malignant biliary occlusion by means of transhepatic percutaneous biliary drainage with insertion of metal stents – Results of an 8-year follow-up and analysis of the prognostic parameters. Rofo. 2003;175:1125-9.
- [Google Scholar]
- Percutaneous palliation of malignant obstructive jaundice with the Wallstent endoprosthesis: Follow-up and reintervention in patients with hilar and non-hilar obstruction. J Vasc Interv Radiol. 1993;4:597-604.
- [Google Scholar]






