Translate this page into:
Effectiveness of Gabapentinoids for Cancer-related Rectal and Vesical Tenesmus: Report of Four Cases
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Gabapentinoids could be assumed to relieve cancer-related rectal/vesical tenesmus based on their pharmacological mechanism. Four patients were refractory for cancer-related rectal/vesical tenesmus although their opioid doses were titrated up. Symptom intensity difference (SID) between initiation and follow-up after 24, 48, and 72 h and daily changes in the frequency of urination, defecation, opioid rescue doses, presence of sleep disruption, and dose of regular opioid medication were evaluated. The median reductions in daily discomfort measured as SID between baseline and follow-up after 24, 48, and 72 h were 87.5%, 70.0%, and 80.0%, respectively, while those in daily pain intensity were 75%, 66.7%, and 66.7%, respectively. The initiation dose of gabapentin was 200 or 400 mg/day and that of pregabalin was 75 mg/day in one patient. Gabapentinoids were effective at low doses administered over a short duration to patients with refractory cancer-related rectal/vesical tenesmus.
Keywords
Analgesics
cancer
gabapentin
pregabalin
tenesmus
INTRODUCTION
Malignant tumors of the pelvic viscera and retroperitoneum cause rectal and/or vesical tenesmus with a prevalence of 14% in patients with advanced rectal cancer;[12] however, few reports have investigated effective treatments. Gabapentinoids are adjuvant analgesics for refractory cancer pain and are effective against rectal/vesical tenesmus in noncancer patients.[34] However, their effectiveness against cancer-related rectal or vesical tenesmus has not been reported. We aim to report the effectiveness cases of gabapentinoids against cancer-related rectal/vesical tenesmus.
CASE REPORT
Methods
We present the cases of four patients who were effectively treated with gabapentinoids for refractory rectal/vesical tenesmus induced by malignant tumors. Therefore, patients who were effectively treated with pregabalin or gabapentin for rectal and vesical tenesmus after ineffective treatment with opioids at the National Cancer Center Hospital between April 2009 and March 2014 were screened in October 2014 and May 2019 using electronic medical records. These patients were diagnosed with primary malignant tumors of the rectum or bladder or with metastatic malignant tumor of the pouch of Douglas or rectovesical pouch. In all cases, the diagnosis had been made using computed tomography. The numeric rating scale (NRS; 0–10) was used to evaluate the intensity of discomfort (0 representing “no tenesmus” and 10 representing “intolerable tenesmus”) and pain intensity in the lower abdomen and/or anus (0 representing “no pain” and 10 representing “intolerable pain”) induced by rectal/vesical tenesmus. The primary parameters reflecting the effectiveness of gabapentinoids were changes in average discomfort and pain intensity during the previous 24 h, measured as the symptom intensity difference (SID) between the initiation (baseline) and follow-up after 24, 48, and 72 h. The secondary parameters were daily changes in the frequency of urination and defecation, opioid rescue doses, presence of sleep disruption, and dose of regular opioid medication calculated as oral morphine equivalent daily dose (MEDD). We assessed the adverse events using a 4-point scale based on symptom intensity (none, mild, moderate, and severe) for 72 h after administration. The patient's previous analgesics and adjuvant analgesics were unchanged, and their doses were not increased throughout the study period.
RESULTS OF CASE SERIES
Gabapentinoids were found to be effective in managing cancer-related rectal and vesical tenesmus in four patients [Table 1]. The median reduction in daily discomfort caused by rectal/vesical tenesmus, measured as SID between baseline and follow-up after 24, 48, and 72 h were 87.5% (range, 60%–100%), 70.0% (range, 25%–100%), and 80% (range, 50%–100%), respectively. The reductions in daily pain intensity of the lower abdomen and/or anus between baseline and follow-up after 24, 48, and 72 h were 75% (range, 66.7%–100%), 66.7% (range, 0%–100%), and 66.7% (range, 33.3%–83.3%), respectively. The frequency of urination and defecation decreased. The starting dose of gabapentin was 200 or 400 mg/day and that of pregabalin was 75 mg/day; in only one patient, the dose of gabapentin was increased to a maximum of 800 mg/day to reduce the symptom intensity. The median MEDD at initiation of a gabapentinoid was 187.5 mg; three patients received oxycodone and one received fentanyl. Increased dose of gabapentinoids or analgesics, including opioids, or any other analgesic adjuvant was required from the end of observation (72 h after starting gabapentinoids) to their discharge (median 10 days after starting gabapentinoids). Among the patients, two reported mild somnolence. Their opioid dosage was decreased, which improved the somnolence within 1 day and did not worsen the symptoms induced by rectal/vesical tenesmus.
| Gender/age | Diagnosis/cause of symptoms | Discomfort intensity on NRS*a after 0/24/48/72 (h) | Pain intensity on NRS*b after 0/24/48/72 (h) | Frequency of urination (defecation) before 24-0/after 0-24/24-48/48-72 (h) | Presence of sleep disruption after 0/24/48/72 (h) | Frequency of rescue dose before 24-0/after 0-24/24-48/48-72 (h) | Dose of gabapentinoid (mg/day) after 0-24/24-48/48-72 (h) | Dose of opioid (MEDD) after 0-24/24-48/48-72 (h) |
|---|---|---|---|---|---|---|---|---|
| Male/42 | Rectum cancer/rectum tumor | 3/0/0/0 | 3/0/0/1 | 9/6/6/7 (Colostomy) | +/−/−/− | 4/0/0/0 | Gabapentin 400/400/400/400 | Oxycodone 315/210/210/210 |
| Male/49 | Gastric cancer/metastatic tumor at rectovesical pouch | 4/1/0/0 | 3/1/1./1 | 15/8/6/5 (6/2/2/1) | +/−/−/− | 3/1/1/1 | Gabapentin 200/200/200/200 | Oxycodone 60/60/60/60 |
| Female/68 | Sigmoid cancer/metastatic tumor at Douglas’ pouch | 4/0/3/2 | 3/1/3/2 | Urethral catheterization (4/1/2/2) | +/−/−/− | 1/0/0/0 | Gabapentin 400/400/600/800 | Fentanyl 58/58/58/58 |
| Male/59 | Malignant lymphoma/bladder tumor | 5/2/3/2 | 3/1/2/1 | 6/3/8/3 (1/1/0/0) | +/−/−/− | 6/5/5/1 | Pregabalin 75/75/75/75 | Oxycodone 480/480/480/360 |
*aDiscomfort intensity on NRS: Average discomfort intensity about rectal/vesical tenesmus during the past 24 h as NRS, *bPain intensity NRS: Average pain intensity in lower abdomen and/or anal during the past 24 h as NRS. 0 representing “No tenesmus” and 10 representing “Intolerable tenesmus.” MEDD: Oral morphine equivalent daily dose (mg/day), NRS: Numerical pain rating scale (0-10, where 0 corresponded to no symptom and 10 to intolerable symptom)
Sample case history
A 42-year-old man was diagnosed with rectal cancer and multiple metastatic liver tumors and underwent defunctioning colostomy. The rectal tumor caused rectal and vesical tenesmus with discomfort, lower abdominal and anal pain, unremitting defecation urgency (despite defunctioning colostomy), and sleep disruption [Figure 1]. He received combination therapy comprising acetaminophen (4000 mg/day) and a nonsteroid anti-inflammatory drug (naproxen, 600 mg/day).
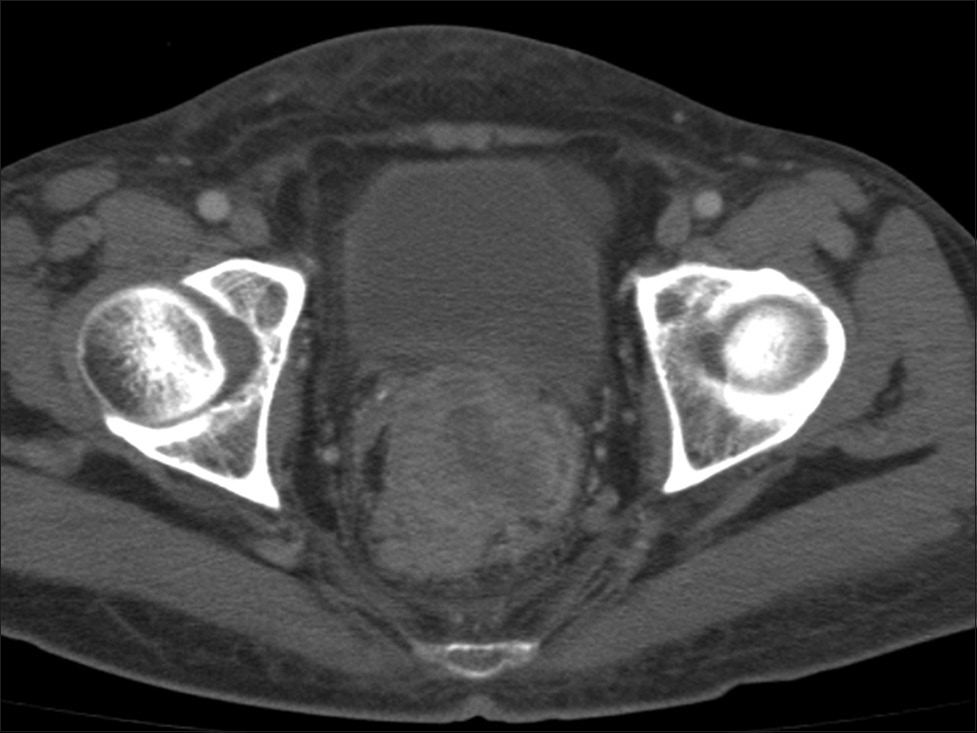
- Computed tomography scan revealed that the rectum was filled with malignant tumor, which invaded the surrounding area, including the urinary bladder
Initially, the opioid dose was titrated until poor analgesic responses or intolerance to opioid-induced side effects. Oral oxycodone, which was increased to 210 mg/day, did not improve his pain at all (3 out of 10 on the NRS). Second, he received systematic lidocaine administration; however, it was ineffective. We suggested to the patient that any other analgesic adjuvants and nerve block could be considered for his refractory cancer-related rectal/vesical tenesmus.[2] The patient chose to receive systemic administration of analgesic adjuvants before trying the nerve block. We started gabapentin because it has been mostly used as an adjuvant analgesic for refractory cancer pain.[3]
Gabapentin was started at 400 mg/day combined with oxycodone, which alleviated the lower abdomen and anal pain to 0 out of 10 the following day. Furthermore, unremitting defecation urgency and sleep disruption improved; however, he reported mild somnolence. The oxycodone dose was decreased from 210 mg/day to 140 mg/day, which reduced the somnolence without return of symptoms associated with rectal/vesical tenesmus. He was discharged 10 days after starting gabapentin. The analgesics and analgesic adjuvants were not changed any further until discharge.
DISCUSSION
The cases illustrate the effectiveness of gabapentinoids in improving the symptoms induced by cancer-related rectal and vesical tenesmus. In addition, gabapentinoids may have a beneficial effect on those patients at low doses and in a short time frame. Ní Laoire et al.[2] conducted a systematic review and reported a case series on the pharmacological treatments for malignancy-related tenesmus, including diltiazem, nifedipine, methadone, mexiletine hydrochloride, lidocaine, and bupivacaine. Gabapentinoids are effective against rectal/vesical tenesmus in noncancer patients;[4] in our study, we reported a similar effect on cancer patients.
The pathophysiology of cancer-related rectal and vesical tenesmus is not fully understood. Ní Laoire et al.[2] suggested that invasion by a malignant tumor and inflammation of the pelvic viscera (bladder, colon, or rectum), along with the involvement of the parasympathetic nervous system or somatic afferents, may cause hypersensitivity and hyperalgesia, resulting in neuropathic pain, discomfort, and smooth muscle contraction in the pelvic viscera. Gabapentinoids inhibit hypersensitivity and hyperalgesia by binding of the α2 δ subunits in association with the voltage-gated calcium channels in the cell membrane, and in turn, bind to subunits that are upregulated in the primary sensory afferents and spinal cord in neuropathic pain.[5] Gabapentinoids inhibit bladder, visceral, and rectal afferent and/or efferent hypersensitivity and excitability of the sacral reflex center induced by cancer-induced inflammatory stimuli and mitigate the stress of a painful disease entity.[67] Bladder irritation and bladder outlet obstruction are consequences of detrusor denervation and upregulation of the afferent C-fiber sensory neurons, resulting in an overall increase in afferent and efferent signaling that contributes to bladder overactivity.[78] Basic research showed that N-type calcium channels were upregulated in the bladder detrusor and spinal dorsal horn after bladder outlet obstruction in rats and that blockade inhibited detrusor overactivity mediated by enhancement of the N-type calcium channels at the cholinergic terminals that innervate the urinary bladder.[8] Gabapentin specifically binds to the α2 δ1 subunits of the N-type calcium channels and exerts various actions responsible for pain attenuation.[9] Previous studies on rats subjected to peripheral nerve injury showed that gabapentinoids reduced presynaptic γ-aminobutyric acid release to disinhibit the locus coeruleus neurons via α2 δ interactions, thereby activating the descending bulbospinal noradrenergic inhibition to produce analgesia.[10] From these findings, we speculate that gabapentinoids inhibit pelvic visceral hypersensitivity and hyperalgesia in part by activating descending noradrenergic inhibition, although the exact mechanisms remain unknown.
Gabapentinoids may improve symptoms induced by cancer-related rectal/vesical tenesmus through multiple mechanisms. Nevertheless, this study had some limitations owing to the small number of individuals and the single-center retrospective design. In addition, a patient received chemotherapy at the same time; however, the observation period of this study was short to assess the effects of chemotherapy.
Although our retrospective report presents low level evidence, it shows that gabapentinoids are effective in improving the symptoms induced by cancer-related rectal and vesical tenesmus based on the pathophysiology and pharmacological mechanisms of gabapentinoids. Large-scale prospective observational studies are being planned to investigate the effectiveness of adjuvant analgesics for symptoms of refractory cancer using the pathophysiology of cancer pain and pharmacological mechanism of each adjuvant analgesic. We believe that these studies will prove the efficacy of gabapentinoids for cancer-related rectal/vesical tenesmus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing.
REFERENCES
- Pain and quality of life after treatment in patients with locally recurrent rectal cancer. J Clin Oncol. 2002;20:4361-7.
- [Google Scholar]
- A systematic review of the effectiveness of palliative interventions to treat rectal tenesmus in cancer. Palliat Med. 2017;31:975-81.
- [Google Scholar]
- Gabapentin for neuropathic cancer pain: A randomized controlled trial from the gabapentin cancer pain study group. J Clin Oncol. 2004;22:2909-17.
- [Google Scholar]
- The efficacy of pregabalin for prevention of catheter-related bladder discomfort: A prospective, randomized, placebo-controlled double-blind study. J Anesth. 2015;29:212-6.
- [Google Scholar]
- Injury type-specific calcium channel alpha 2 delta-1 subunit up-regulation in rat neuropathic pain models correlates with antiallodynic effects of gabapentin. J Pharmacol Exp Ther. 2002;303:1199-205.
- [Google Scholar]
- Alpha 2 delta (a(2)d) ligands, gabapentin and pregabalin: What is the evidence for potential use of these ligands in irritable bowel syndrome. Front Pharmacol. 2011;2:28.
- [Google Scholar]
- Enhanced sensitivity to afferent stimulation and impact of overactive bladder therapies in the conscious, spontaneously hypertensive rat. J Pharmacol Exp Ther. 2011;338:392-9.
- [Google Scholar]
- Changes in the function and expression of T-type and N-type calcium channels in the rat bladder after bladder outlet obstruction. J Urol. 2014;191:1159-67.
- [Google Scholar]
- Implications and mechanism of action of gabapentin in neuropathic pain. Arch Pharm Res. 2013;36:237-51.
- [Google Scholar]
- Gabapentin inhibits γ-amino butyric acid release in the locus coeruleus but not in the spinal dorsal horn after peripheral nerve injury in rats. Anesthesiology. 2012;116:1347-53.
- [Google Scholar]






