Translate this page into:
Quality of Life with Cancer: Role of Physicians for a Better Well-Being
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
There has been an increasing number of cancer cases in India with the current toll at 2.5 million, and around 700,000 cases added each year.[1] Palliation is an integral part of oncological treatment. Palliative care aims to improve the quality of life (QOL) of patients and their family. Like Jonson et al.[2] said “QOL refers to the subjective satisfaction expressed or experienced by an individual in his physical, mental and social situation,” therefore, palliation provides a holistic approach to patient therapy.
In an article, Fowlie et al.[3] said “patient's QOL is not determined so much by the extent of his symptoms, the quality of his support system, or his knowledge of or involvement in his disease or treatment, but rather by the extent to which he has come to terms with his condition and is at peace with himself.”
The objectives of the present study were to determine the QOL in patients diagnosed with cancer visiting the hospital and finding issues affecting their life, especially in times of a terminal illness. The general version of the Functional Assessment of Cancer Therapy (FACT-G) questionnaire[4] was used to assess the QOL of patients. The FACT-G questionnaire was licensed for use in English and Hindi in this study. Version 4 of the questionnaire has four sections: measuring physical, social/family, emotional, and functional well-being. The responses are then scored based on the given template, and the QOL is obtained. There has been no given cutoff to grade QOL as poor, but lower scores are associated with poorer QOL.
The hospital ethics committee approved the study protocol. A total of 60 patients aged between 34 and 82 years were included in this study. The detailed purpose and procedure of the study were explained to them, and a signed consent form was obtained. All of the participants were assured confidentiality of the collected data. Most patients answered the questions themselves; some who needed assistance, especially the illiterate or the physically impaired were assisted by the nurse on duty.
Our study population consisted of 48 (80%) males and 12 (20%) females. The distribution of the type of cancer was as follows: prostate cancer - 14 (23.3%), cervical cancer - 7 (11.7%), lung cancer - 6 (10%), colon cancer - 6 (10%), laryngeal cancer - 5 (8.3%), carcinoma of the stomach - 4 (6.7%), cancer of buccal mucosa - 3 (5%), breast cancer - 3 (5%), esophageal cancer - 2 (3.3%), carcinoma of the gallbladder - 2 (3.3%), tonsillar carcinoma - 2 (3.3%), chronic myeloid leukemia - 1 (1.7%), Hodgkin's lymphoma - 1 (1.7%), non-Hodgkin's lymphoma - 1 (1.7%), pancreatic carcinoma - 1 (1.7%), ovarian carcinoma - 1 (1.7%), and carcinoma of the tongue - 1 (1.7%). All patients were currently on treatment.
The FACT-G QOL score ranged between 21 and 80 (50.92 ± 16.49) in our study population [Figure 1]. The scores can be between 0 and 108; this shows that most patients had a poorer QOL. Even with lower scores on the index, 23 (38.3%) patients were quite a bit, and 20 (33.3%) were somewhat satisfied with the life they were living. Twenty-one (35%) and 9 (15%) patients were experiencing a lot or quite a bit of pain, respectively, in the past 1 week; whereas, 12 (20%) and 11 (18.3%) experienced no or a very little pain. It was noted that 31 (51.7%) patients were disturbed from the side effects of their treatment and 12 (20%) were not experiencing any difficulties with the side effects of their therapy. Pain has always created a negative impact on the QOL. Many chronic pain sufferers have expressed that pain has caused a negative impact on their mental health, sleep, job, and personal relationships. It has also been shown in various past studies that inadequate pain control, end of dose pain, and side effects have affected individuals and their relationship with physicians.[4] Therefore, it should be ensured that physicians consider the factor of pain and other side effects to provide effective management to improve the overall end-of-life palliation and care.
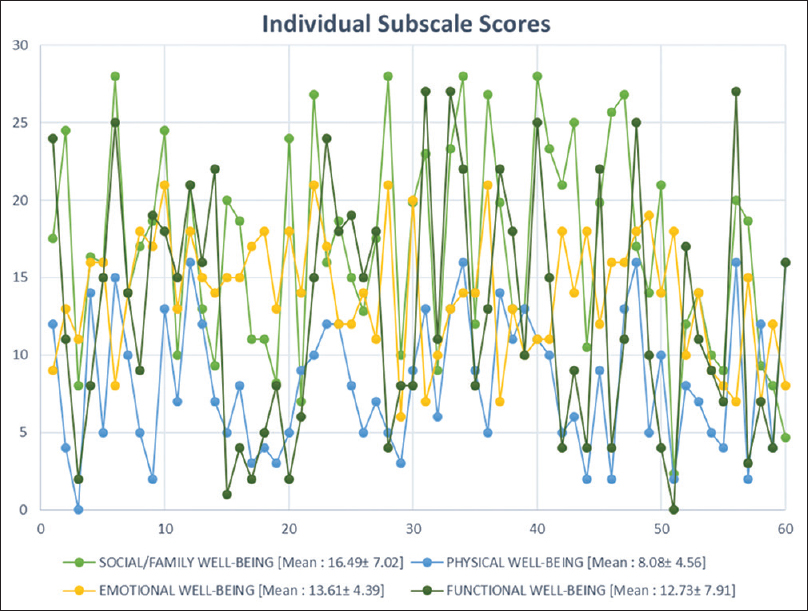
- FACT-G individual subscale scores of patients (N=60).
Thirty-seven (61.6%) patients were anxious about their illness and deteriorating condition. Of the 60 participants, 40 (66.6%) participants were having good support from their family and friends during the time of illness. It is important that all physical, mental, emotional, and spiritual problems are addressed. As physicians, our role does not end at therapy; we can go beyond. We can organize camps or meetings in hospitals or clinics where patients meet other people fighting a similar battle. Getting a chance to interact with others will alleviate their fears and decrease the anxiety and fear associated with the illness. Patients can also be advised of complementary therapy such as yoga to modulate their stress response system and help them live a better QOL. For most, cancer is nothing more than a death sentence; hence, it should be ensured that all patients needs are catered to. Physicians should understand that cancer therapy and a good QOL are not mutually exclusive components; therefore, improving the QOL with effective treatment should be our ultimate goal.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Addressing a long-felt need: Introducing palliative care for MBBS students in the new competency-based medical education curriculum. Indian J Palliat Care. 2019;25:359-60.
- [Google Scholar]
- Clinical Ethics A Practical Approach to Ethical Decisions in Clinical Medicine. London: Bailliere Tinda11; 1982.
- Quality of life in advanced cancer: The benefits of asking the patient. Palliat Med. 1989;3:55.
- [Google Scholar]
- The impact of pain on quality of life and the unmet needs of pain management: Results from pain sufferers and physicians participating in an internet survey. Am J Ther. 2008;15:312-20.
- [Google Scholar]





