Translate this page into:
Propensity Score Matching with Retrospective and Observational Data in Palliative Care
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Randomized controlled trial (RCT) is considered gold standard in terms of clinical research as it provides best level of evidence which is required to establish a link between treatment and outcomes.[1] RCT eliminates bias and confounding factors, enrolls patients into the desired group using a predecided inclusion and exclusion criteria, and ensures that the collected data are accurate and statistical analysis is reliable. However, executing an RCT in a setting of palliative care is difficult as it is costly to conduct, is unethical on several occasions, and is time consuming. A possible solution to this is planning a retrospective study. The biggest hurdle in such a situation is the presence of bias.[2] Another issue is that the level of evidence generated by retrospective data will not be good enough, and thus the recommendation made by the results will be difficult to accept and subsequently implement.
Observational studies are easy to conduct, are relatively cheaper, and can be designed prospectively or retrospectively in palliative care. However, confounding bias is common in observational studies as the participants are not randomized, thus interfering with the elimination of causal effects. Statistical methods are available which can be applied to the collected observational data and include only those participants who have matching characteristics to reduce bias in two groups and thus provide the researchers with more reliable data.[3]
In the era of electronic medical records, the database is full of information which by careful planning and understanding can be retrieved and analyzed using appropriate statistical tests retrospectively. This is possible by using propensity scores. Propensity scoring methods can be applied to retrospective data in which there is well-defined treatment or intervention which is compared to either a control or an existing standard of care. Propensity scoring is a prediction model that predicts the likelihood of treatment or intervention depending on a specific set of patient characteristics or variables.[4] The scoring weighs two nonequivalent groups on observed characteristics in such a way that there is less bias in the interpretation of overall effects. This balancing is done by matching study participants in comparison groups on propensity scores, weighing for propensity scores, or adjusting for propensity scores in the final analysis. By doing so, there is a uniform distribution of characteristics for participants in both arms [Figure 1]. Using propensity scoring, researchers can create study groups which are similar to each other in terms of demography and diagnosis and thus can accurately arrive at a relationship between treatment/intervention and outcome.
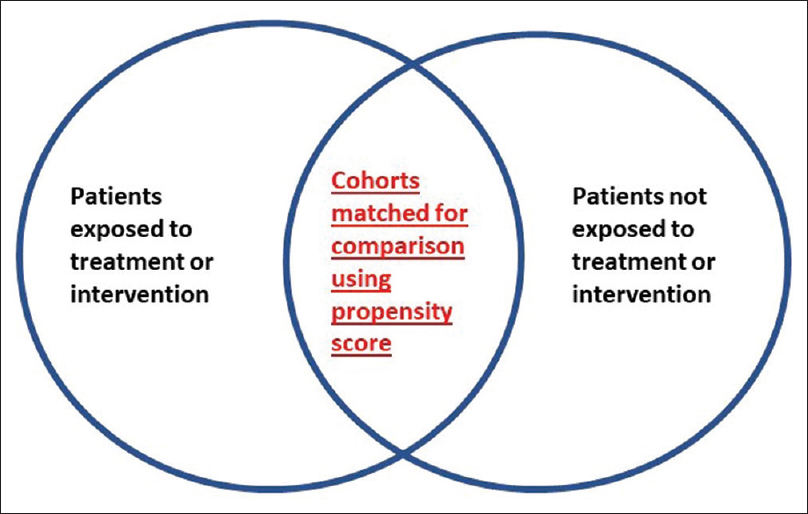
- Control group and treatment/intervention group in two circles. The area which is overlapping indicates the propensity score-matched cohorts having matching characteristics which can be analyzed
There are several ways of using propensity score.[5] In propensity score matching, two groups of patients who either received or did not receive a treatment or intervention are compared based on the propensity score match. This type of data is considered as reliable as an RCT. Another way is stratification of propensity score in which participants are divided into groups or strata based on propensity scores and are subsequently analyzed. The bias is reduced if the participants are divided into more strata or groups.[6]
When propensity scoring is used for retrospective data, the researchers need to exclude participants in either group as they might not be able to retrieve information that they need to collect and analyze. Therefore, to perform an adequately powered research using propensity scoring, a lot of records need to be retrieved which can be time consuming and cumbersome. We suggest consulting a biostatistician before designing a study using propensity score to have a research question and smooth data acquisition and analysis thereafter.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Propensity score matching: Retrospective randomization? J Foot Ankle Surg. 2017;56:417-20.
- [Google Scholar]
- An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399-424.
- [Google Scholar]
- Areview of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariable methods. J Clin Epidemiol. 2006;59:437-47.
- [Google Scholar]
- Propensity score methods: Theory and practice for anesthesia research. Anesth Analg. 2018;127:1074-84.
- [Google Scholar]





