Translate this page into:
Cebranopadol: A First-in-Class Nociceptin Receptor Agonist for Managing Chronic Pain
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Nociceptin/orphanin FQ (N/OFQ) peptide receptor or NOP receptor is a member of opioid receptors, such as mu-opioid peptide (MOP), delta-opioid peptide, and kappa-opioid peptide (KOP) receptor.[1] NOP receptor and its ligand N/OFQ have been extensively studies in the last two decades. Just like opioid receptors, NOP receptors are spread extensively in the central and peripheral nervous systems. Like opioid receptors, NOPs are also G-protein coupled receptors. Subsequently, selective NOP receptor agonists were studies for use in pain management to avoid adverse effects of routinely used MOP receptor agonists. Till date, they have not been approved for clinical use.
MOP receptor agonists are considered gold standard for managing acute pain and chronic pain of cancer and certain noncancer origin. However, there are undesirable effects such as constipation, nausea/vomiting, sedation, tolerance, and addiction, which are related to dose and duration of use. Use of agents with combined NOP and MOP receptor agonist activity has been described which has better analgesic profile and lesser side effects.
Cebranopadol is a novel, centrally acting, potent, first-in-class analgesic drug, which acts by dual-mechanism, i.e. NOP receptor and MOP receptor agonism.[2] It has partial activity toward KOP receptor also. In spite of MOP and KOP receptor agonistic properties, the clinical effects of cebranopadol are not similar to these receptors agonism, i.e., it has lesser or minimal adverse effect profile with similar analgesia properties. Experimental studies have shown efficacy of cebranopadol in chronic cancer pain, inflammatory conditions such as osteoarthritis, neuropathic pain such as low back ache, and certain acute nociceptive pain also.[3] Chemically, cebranopadol is trans-6,9-fluoro-4,9,9,9-dihydro-N, N-dimethyl-4-phenyl-spiro(cyclohexane-1,1,9(3,9, H)-pyrano 34-b] indol)-4-amine [Figure 1]. In experimental studies, it has been found useful in managing acute postoperative pain, chronic neuropathic pain such as low back ache, diabetic neuropathy, and cancer pain. It has been used intravenously (IV) and orally in several studies.[4]
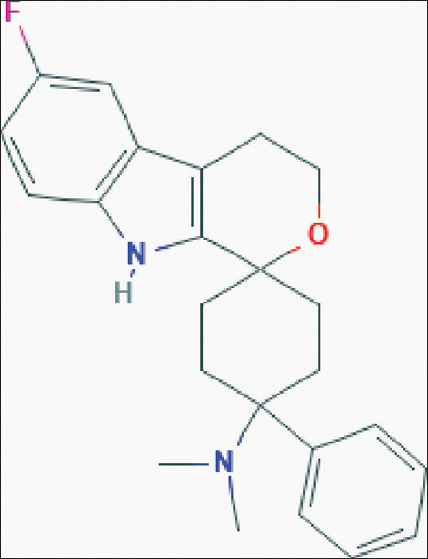
- Structure of cebranopadol (Image source: National Center for Biotechnology Information. PubChem database. Cebranopadol, CID = 11848225, https://pubchem.ncbi.nlm.nih.gov/compound/Cebranopadol [accessed on June 30, 2019])
Cebranopadol binds to NOP and MOP receptors with equal affinity and provides good-quality analgesia in animal studies and humans. The drug was better tolerated at various doses when administered orally (200, 400, and 600 μg) and did not appear to cause respiratory depression, nausea, vomiting, or sedation at above-mentioned doses.[5] It is a long-acting drug, and therefore, a single dose in 24 h has been shown to be effective in many varieties of pain model. The plasma half-life when used IV is around 4.5 h. After an IV injection at a dose ranging from 0.5 to 5.6 μg/kg, the pain relief lasted for up to 7 h. The efficacy and duration of analgesia are different in different conditions. Compared to an oral dose of 200 μg/day, patients who received 400 and 600 μg had better pain relief and less rescue analgesic requirements.[6] In human studies, there was no manifestation of withdrawal symptoms noted when cebranopadol was abruptly discontinued after around 14 weeks of clinical use. However, the US-FDA approval is still due.
In conclusion, cebranopadol is a novel centrally acting opioid which appears to have a better profile compared to MOP receptor agonists and various partial agonists, which are quite popular in clinical practice. Results on ongoing studies are awaited which might guide clinicians in using it in specific situations that can have cost-effective, favorable outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cebranopadol: A novel potent analgesic nociceptin/orphanin FQ peptide and opioid receptor agonist. J Pharmacol Exp Ther. 2014;349:535-48.
- [Google Scholar]
- Cebranopadol, a novel first-in-class analgesic drug candidate: First experience in patients with chronic low back pain in a randomized clinical trial. Pain. 2017;158:1813-24.
- [Google Scholar]
- Cancer-related chronic pain: Investigation of the novel analgesic drug candidate cebranopadol in a randomized, double-blind, noninferiority trial. Eur J Pain. 2019;23:577-88.
- [Google Scholar]
- Cebranopadol: A novel first-in-class potent analgesic acting via NOP and opioid receptors. Handb Exp Pharmacol. 2019;254:367-98.
- [Google Scholar]
- Cebranopadol: A novel, first-in-class, strong analgesic: Results from a randomized phase IIa clinical trial in postoperative acute pain. Pain Physician. 2018;21:E193-206.
- [Google Scholar]
- Clinical pharmacokinetic characteristics of cebranopadol, a novel first-in-class analgesic. Clin Pharmacokinet. 2018;57:31-50.
- [Google Scholar]





