Translate this page into:
Effectiveness of the MELD/Na Score and the Child–Pugh Score for the Identification of Palliative Care Needs in Patients with Cirrhosis of the Liver
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
Identification of palliative care needs in patients with liver cirrhosis using the MELD/Na score and the Child–Pugh score.
Materials and Methods:
A retrospective study of hospitalized patients with hepatic cirrhosis between January 2015 and December 2016 using the Child–Pugh score and the MELD/Na score in January 2018.
Results:
Recognizing end-of-life patients (the past 12 months of life) is a challenge for health professionals, especially in diseases with poorly defined criteria, such as cirrhosis of the liver. The verification of rapid functional decline and health indicators can be verified using already defined scales such as the Child–Pugh score and the MELD/Na score. Patients were classified according to the Child–Pugh score in Class A (17%), Class B (48.9%), and Class C (34%). The corresponding survival rate was as follows: class A (87.5%), Class B (30.4%), and Class C (31.25%). The MELD/Na score intervals were >9 (2.15%), score 10–19 (46.8%), score 20–29 (27.7%), score 30–40 (19.1%), and score >40 (4.3%). Nearly 51.1% had a MELD/Na score >20 and 48.9% <20. The study revealed that 59.6% of patients died before 12 months. They were end-of-life patients who needed palliative care to reduce the impact of the disease.
Conclusions:
The Child–Pugh score and the MELD/Na score represent a viable and easy-to-use tool to identify patients in need of palliative care, among those with liver cirrhosis. Early identification, timely evaluation, and effective treatment of physical, spiritual, family, and social problems improve the quality of life of people with incurable diseases and their families.
Keywords
Child–Pugh score
cirrhosis of the liver
identification of palliative care needs
MELD/Na score
INTRODUCTION
People are “approaching the end of life” when they are likely to die within the next 12 months. Patients with chronic liver disease have a life-limiting illness that causes multiple distressing symptoms and negatively affects quality of life. This population traditionally does not have an instrument for the identification of palliative care needs the “end of life,” the MELD/Na score, and the Child–Pugh score may be useful in its identification.[123]
Patients with cirrhosis of the liver should be treated with specific treatments for the control of symptoms at the end of their life course because of the strong impact of the disease on the patient and the family. To properly care for these patients, it is necessary to identify and organize an interdisciplinary plan of professionals in palliative care, with the intention of reducing the impact of the disease on patients.[45]
MATERIALS AND METHODS
A retrospective study of hospitalized patients with hepatic cirrhosis between January 2015 and December 2016 using the Child–Pugh score and the MELD/Na score in January 2018.
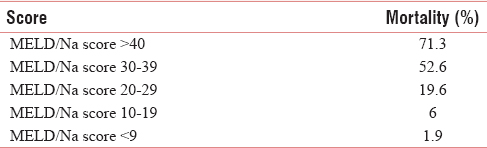
The MELD/Na score is a scoring system for accessing the severity of chronic liver disease using values as serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time and sodium, to predict survival [Table 1].
The Child–Pugh score is used to access the prognosis of chronic liver disease, mainly cirrhosis. The score employs five clinical measures of liver disease: total bilirubin, serum albumin, prothrombin time, ascites, and hepatic encephalopathy [Table 2].[67]

RESULTS AND DISCUSSION
During this period, 6493 patients were hospitalized and 47 with liver cirrhosis were included in this study [Table 3].

The median age was 64.3 years; 95.7% were male. The median hospitalization time was 10.7 days. The overall mortality rate was 68.1%.
Patients were classified according to the Child–Pugh score in Class A (17%), Class B (48.9%), and Class C (34%). The corresponding survival rate was as follows: class A (87.5%), Class B (30.4%), and Class C (31.25%).
The 1-year mortality rate was as follows: class A (12.5%), Class B (65.2%), and Class C (68.75%). The mortality rate after the 1st year was as follows: class A (0%), Class B (4.3%), and Class C (0%). Palliative care needs were identified in Classes B and C [Table 4].

The MELD/Na score intervals were >9 (2.15%), score 10–19 (46.8%), score 20–29 (27.7%), score 30–40 (19.1%), and score >40 (4.3%). Nearly 51.1% had a MELD/Na score >20 and 48.9% <20 [Table 5].

In January 2018, 31.9% were alive. About 44.7% had died in <3 months, 10.6% between 3 and 6 months, and 4.3% after 6 months.
The study revealed that 59.6% of patients died before 12 months. They were end-of-life patients who needed palliative care to reduce the impact of the disease.
According to the Child–Pugh score, in <1 year, the mortality rate of patients in Class B was 65.2% and 68.7% in Class C, and according to the MELD/Na score, patients with a score >20 had 51.1% mortality.
Given these percentages, both classes of patients had criteria to be identified as end-of-life patients requiring special care.
Patients had a decrease in quality of life, clinical, psychological, social, and family changes. Therefore, therapeutic adjustment was necessary to control the worsening of the following symptoms: edema, ascites, fever, fatigue, tiredness, drowsiness, confusion, loss of appetite, pain, dyspnea, and increased bleeding.
CONCLUSIONS
According to the MELD/Na score, in a 3-month period after hospitalization, a number between 19.6% and 71.3% of patients had a mortality likelihood of 51.1%. These numbers of patients were in need of palliative care. The confirmed mortality rate was 44.7%, during these first 3 months.
According to the Child–Pugh score, our Classes B and C patients have a mortality of 65.2% and 68.75% at 1 year, respectively, needing palliative care.
The Child–Pugh score and the MELD/Na score represent a viable and easy-to-use tool to identify patients in need of palliative care, among those with liver cirrhosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol. 2005;42(Suppl (1)):S100-7.
- [Google Scholar]
- Cirrhosis in Adults: Etiologies, Clinical Manifestations, and Diagnosis. 2016. UpToDate. Available from: https://www.uptodate.com/contents/cirrhosis-in-adults-etiologies-clinical-manifestations-and-diagnosis
- [Google Scholar]
- Important predictor of mortality in patients with end-stage liver disease. Clin Mol Hepatol. 2013;19:105-15.
- [Google Scholar]
- Downgrading MELD improves the outcomes after liver transplantation in patients with acute-on-chronic hepatitis B liver failure. PLoS One. 2012;7:e30322.
- [Google Scholar]
- Integration of palliative care in end-stage liver disease and liver transplantation. J Palliat Med. 2014;17:1271-7.
- [Google Scholar]
- Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91-6.
- [Google Scholar]






