Translate this page into:
Decubitus Ulcer Development: An Investigation on Its Effect and Evidence in Home Care Patients
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Aims:
Decubitus ulcer (DU) is one of the commonly observed health problems among home care patients. As well as deteriorating social, physical, and psychological conditions of the patients, it is a cause of severe economic loss due to long-term bed occupancy and high care costs. This study aimed to examine the factors which affect the development of decubitus ulcer among home care patients and provide extensive data to the literature.
Patients and Methods:
This study was conducted with on home care patients aged over 40 years old who were registered at Etimesgut Ankara Sehit Sait Erturk State Hospital. Following the face-to-face interviews with the patients at home, the scores of Subjective Global Assessment (SGA), Mini Nutritional Assessment (MNA), Daily Life Activities (DLA), and Geriatric Depression Scale (GDS) were recorded. Development of DU was monitored through routine examinations in the home care patients. It was encountered how SGA, MNA, DLA and GDS functioned in predicting the development of DU using logistic regression during effort and also how status of equipment and presence of comorbid diseases affected its development.
Results:
It was determined that malnutrition affected development of DU by decreasing mobility while the presence of psychological problems increased the risk for development. Furthermore, number of comorbid diseases and status of health equipment used by the patients were found effective in the development of DU.
Conclusion:
It is obvious that decreased inability of independent mobility in DLA increase the risk for malnutrition and consequently two assessments show a negative impact on psychology of the patient.
Keywords
Daily life activities
decubitus ulcer
depression scale
logistic regression
nutrition
INTRODUCTION
Pressure sore, which is also known as decubitus ulcer (DU), is a clinical situation. It involves ischemia, necrosis, and tissue necrosis due to pressure on the body parts which remained immobile for a long time. As well as threatening life quality of the patient by affecting the physical health, pressure sores also cause psychological problems such as loss of independence and social isolation.[1] Pressure sores are life-threatening problems because of movement restriction especially in the geriatric patient group. Decreased cognitive functions or movement restriction among geriatric patients increases the risk for pressure sores.[23] Although approximately 90% of pressures sores can be prevented with accurate risk assessment and treatment interventions, incidence of pressure sore is 10%–23% in the hospital wards while it may rise to 56% in intensive care units.[4567] Pressure sores which can be prevented with protective measures appear as an important indicator of quality for patient care centers and intensive care units.[8]
It has been reported that DU was observed among 70% of patients aged over 70 years old,[1] 20% of paraplegic patients, 26% of quadriplegic patients,[9] and 6%–14% of individuals with an acute and chronic health problem and higher than 25% of individuals living at nursing homes.[10] A study which was conducted in a neurological intensive care unit has encountered the incidence of pressure sore to be 18.3%.[11]
Ensuring sufficient and balanced nutrition among home care patients have great importance with respect to protecting and improving their health, preventing or delaying development of chronic diseases, extending their lifetime, and increasing their life quality. Malnutrition is a common clinical condition in home care patients and it reaches up to 50% in the society.[12131415] The effect of clinical, social, and cultural factors on development of malnutrition has been emphasized in several studies.[1617] SGA and MNA are the nutritional assessment tools commonly used to determine the presence of malnutrition.[1819] SGA is a subjective application depending on the experience of the practitioner and is a simple, noninvasive, and inexpensive tool which can be applied in a short time.[20] Another assessment, MNA, is a tool recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN) for the patients followed up in-home care programs, nursing homes, and hospitals.[2122]
Impairment, which can be defined as a difficulty or a deficit in performing the activities required to sustain a normal life, is a crucial factor in the development of DU among home care patients. In determining the mobility status of home care patients, daily life activities (DLA) evaluates them regarding the ability to maintain their DLA alone or with assistance. Efficacy of activities such as relieving oneself, taking a bath and doing the chore may vary by several factors such as age, gender, presence of illness, social status, and mental health (Roth, 1990; Lastowiecka, 2006). It has been highlighted that efficacy in DLA has an important impact on development of DU, psychological and physical health problems of the patients (Nakamura, 1997; Sund-Levander and Wahren, 2002; Xavier, 2003).
Life quality is an indicator of the balance between expectations of the individuals from life and their current life. A reduction in cognitive function, biological, and social motives which constitute the essential strength of mental health due to depression has a negative impact on the daily life of the home care patients.[2324] Social and economic decline in the lives of the individuals due to increased physical health problems increases the incidence of psychological disorders in the home care patients. Especially, depression appears to be a key factor which affects life quality solely or concurrently with other disorders. Unless treated, negative outcomes, such as early death, impaired general health status and worsened DU are observed, contrarily, its proper treatment improves life quality.[252627282930]
Due to the poor methodology of previous studies, there is still lack of any extensive study conducted which has investigated the effect of nutrition, independently performed DLA, psychological status, and presence of an accompanying diseases in development of DU in the literature. There may be several factors related and non-related with patient in development of pressure sore. These factors include patient age, accompanying disease, malnutrition, psychological disorders, decreased muscle mass, spasticity, neurological diseases-status of consciousness, immobility, and urinary and fecal incontinence (Jeffrey et al., 2006).[3132] Some authors have reported that malnutrition and mobility also play crucial roles.[123] Stratton et al. (2005) have concluded that high-protein nutrition may help the treatment of pressure sores (PS).
The absence of a study in the literature which has investigated comprehensively the factors that affect the development of DU in the home care patients is a very important lack. Accordingly, this study has investigated the factors which affect the development of DU among home care patients.
PATIENTS AND METHODS
Study population and assessment of clinical characteristics
This prospective study was conducted at Ankara Etimesgut Sehit Sait Erturk State Hospital, Turkey. The study population included 336 home care patients aged over 40 years old who recently registered at the hospital. The approval for the study was taken from Verbal and written informed consents on acceptance to participate in the study were taken from the patients. Demographic data of the patients were collected from the medical records, additional data to complete the questionnaires and physical examinations were obtained by the face-to-face interviews at home.
Oral and written consents of the patients for accepting to participate in the study were received. Information was collected from medical records of the patients, and they were interviewed at their homes and examined the patients.
Assessments
The nutritional status of the patients was determined using the Subjective Global Assessment (SGD) and MNA. The Subjective Global Assessment suggested by Destky et al., (1987) was used in this study. The patients were divided into three groups according to the face-to-face patient interviews: well-nourished, moderately (or suspected to be) malnourished and severely malnourished. MNA was used in determining the other nutritional status assessment. The patients were questioned by six questions, and the classified in three groups based on scores as malnourished between 0–7 points, risky between 8–11 points, and normal nourished between 12–14 points (Vellas et al., 2006).
DLA assessment developed by Barthel was used to identify the DLA of the patients. The patients were divided into two groups based on scores, and the groups indicated total dependence, severe dependence, moderate dependence, and mild dependence with <20; 20–40; 40–60 and >60 scores, respectively (de la Torre-Garcia et al., 2011).
The study used the short form of Geriatric Depression Scale (GDS) which was developed by Yesavage to evaluate depressive symptoms. The validity and reliability studies of the Turkish version of this scale were conducted by Ertan and Eker.[33]
The demographic features of the home care patients, presence of accompanying diseases, equipment availability for accompanying disease at home and status of DU were observed at the period of home examination of the patients.
Statistical analysis
Data collected in the face-to-face interviews with the patients aged over 40 years old were analyzed in the SPSS 20 (SPSS Inc., Chicago IL, USA) software package. Number and percentage distribution, Chi-square, Mann–Whitney U test, and Pearson's correlation analysis were performed in the statistical analysis process. Furthermore, the relationships between SGA, MNA, DLA, GSD, and status of accompanying disease which affect the development of PS (yes/no) and demographic characters of the patients were analyzed with logistic regression, and a prediction model was established. Statistically, significance level was accepted to be P < 0.05.
RESULTS
Characteristics of patients
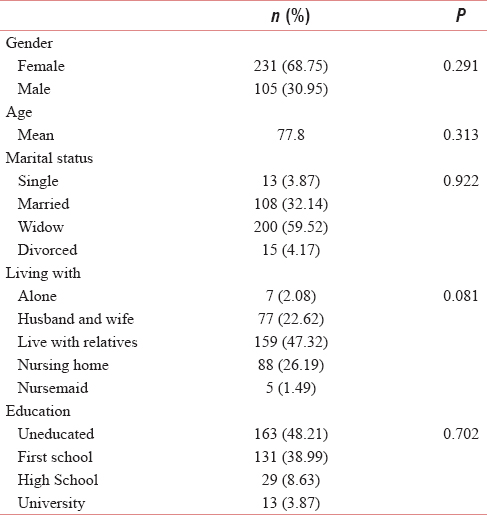
Demographics of 336 home care patients were summarized in Table 1. Of the patients, 68.75% of the patients are female while 30.95% were male, and mean age was 77.8. Study population consisted of 13 married, 108 widows and widower, 200 single and 15 divorced subjects. Most of the patients (177) were living with their relatives while 88 patients were staying at nursing homes. Seven patients were living alone whereas 77 and 5 of the patients were accompanied by their spouses and a nursing maid, respectively. Most of the patients (163) are either uneducated or either primary school graduates (131). Only 13 of them had attended a university.
The distribution of the patients with accompanying diseases, as a factor which affects the development of DU, was presented in Table 2 and their distribution regarding the availability of health equipment at their homes was summarized in Table 3.


It was investigated whether there was an accompanying disease with DU in the home care patients and a correlation between those. It may be concluded according to the results that presence of urinary incontinence (0.000003) was effective in the development of DU. The effects of endocrinological and hematologic diseases were slightly above the significance level of 0.05 and no correlation was found between comorbidity and DU. This result indicates that the presence of an accompanying disease separately showed no impact on development of DU.
It was investigated whether there was a difference resulting from presence and absence of health equipment used by the patients at home in the development of DU. Accordingly, no statistically significant difference was found between the presence and absence of sphygmomanometer (P = 0.646959), nebulizer (P = 0.494435), functional Cot (P = 0.139152), hydrating moisturizer (P = 0.586771), oxygen source (P = 0.150983), and insulin pump (P = 0.586861), diaper use and between the effects of formula support (P = 0.116343) on development of DU. It was observed that there was a difference between the presence and absence of only six equipment such as percutaneous endoscopic gastrostomy, tracheostomy, urinary catheter, enteral pump, pulse oximetry, and mechanical ventilator.
The results of the assessments
In the light of the information obtained in the examinations and follow-ups in the home care patients; their SGA, MNA, DLA, and GDS scores were calculated. It was evaluated whether there was a difference between the assessment scores in the development of DU. The results were given in Table 4.

Subjective Global Assessment was determined for each patient during face-to-face interviews and examinations to identify nutritional status of the patients. It was remarkably found that there was a difference between the scores of nutritional assessments (P = 0.000036) of the patients with respect to the development of DU. Likewise, there was a difference between the scores of nutritional statuses in MNA as another evaluation method with respect to the development of DU (P = 0.003359), there was a statistically significant difference based on dependence status in the development of DU (P < 0.05) in DLA assessment which evaluates the independence status of the patients for daily physical activities. It was also observed that there was a difference between the GDS classifications used for identifying the patients' psychological conditions (P > 0.000011). All examined assessments appear to be affecting the development of DU.
Correlation analyses
Correlation analysis was performed to identify the relationship between the development of DU and nutritional status, daily life activity, depression, number of accompanying diseases, and number of health equipment used by the patients at home who were determined in the follow-up examinations. The results of the analysis were given in Table 5.

A statistically significant correlation was found between the development of DU and independent variables. DU was negatively related with SGA at a moderate level. There was a similar correlation between DU and MNA. Well or moderately nourishment contributed to decreased risk for development of DU. A significantly positive relationship was found between daily life activities and DU. The risk for development of DU decreased as independent mobility of the patients increased in daily activities. Increased independent mobility showed a significantly positive correlation with also psychological conditions of the patients. Deteriorated psychological condition contributed to increased risk for the development of DU. Consequently, the scores of all these examined assessments affected the development of DU.
There was a significantly positive correlation between the number of accompanying diseases and DU development. Increased number of accompanying diseases also increased the risk of DU development. A similar relationship was found with the health equipment used by the patients at home. High number of equipment used at home showed an impact on the development of DU. Higher numbers of equipment increase the risk. This indicates that equipment should be used in treatment process rather than protective medical practice. Increased number of equipment used by patient is an indicator of a poor health status for the patient. A very strongly positive relationship between the number of accompanying diseases and equipment (0.563**) also confirms this assumption.
Logistic regression
Logistic regression was performed to determine the factors which affect the development of DU and to designate the prediction model of DU. Prediction rate of logistic regression was presented in Table 6. Table 7 shows the model outcomes and the model power of the prediction.


The absence of DU was predicted correctly at 98.3% in the model while the development of DU was predicted correctly at 37.20%. Total prediction rate is at 90.405%. The prediction model was given in Table 7. R2 of the model was calculated to be 0.776, and this result means that model's prediction strength and reliability is high.
The Prediction Model can be formulized as follows:
DU = −0.682 + 1.400 SGA – 1.634 MNA – 0.663 DLA – 1.285 GDS + 0.109 AD + 0.180 EQ
DU: Decubitus ulcer, SGA: Subjective Global Assessment, MNA: Mini Nutritional Assessment, DLA: Daily Life Activity, GDS: Geriatric depression Scale, AD: Accompanying Disease, Eq: Equipment.
Prediction results for the development of DU among the patients based on their ages were given in Figure 1, distribution of the DU development based on the patient age was presented in Figure 2.

- Prediction results of the patients

- PS classification based on patient age
DISCUSSION
Geriatric symptoms are most commonly observed among home care patients. The frequency of the geriatric symptoms increases by advanced age. These common symptoms among home care patients include malnutrition, comorbid chronic diseases, and psychological diseases. DU is a major geriatric syndrome leading mortality and morbidity among home care patients. Many factors which contribute to the development of DU have been reported in the literature; however, there is no study which has investigated all these factors concurrently in an identical study. The researchers have listed several factors which affect the development of DU such as malnutrition, immobility, and protein deficiency (Jeffrey et al., 2006; Theisen, 2012).[3132] Malnutrition has been emphasized to play a role in both development of DU and tissue impairment in the studies (Thomas, 2001; Fontaine and Raynaud-Simon, 2008; Schols et al., 2010; Van Anholt, 2010; Pham et al., 2011).[1] Thomas (2001) has stated that DU developed in 17% of the malnourished patients and 9% of the nourished patients in the 4th week of admission (Thomas, 2001). Desvenes (2005) has addressed increased protein and calorie intake and supplementation of vitamins and minerals such as A, C, E, and zinc which increase collagen synthesis, mediate epithelization and enhance the immune system to prevent the development of DU.
Besides the effect of nutrition on the development of DU, it has been stated in another study that individuals carry higher risk because of reduced physical movement due to senility, skin turgor and decreased skin perfusion (Casimiro et al., 2002). The researchers have achieved a consensus that movement restriction is an important factor in the development of DU (Molaschi, 1995; Topeli, 2000; Casimiro, 2002; Atılgan and Karadeniz, 2007). Likewise, several factors, such as movement restriction and malnutrition, have negative impacts on the daily routine life of the patients.[2324] Deteriorated routine life may worsen psychological problems leading to negative outcomes such deteriorated general health, elevated DU and early death.[252627282930]
In the literature, the factors which contribute to the development of DU were addressed separately. Until today, there are only a limited number of studies which have investigated the effects of all these factors concurrently. In our study, we have concurrently evaluated all these factors which may affect the development of DU such as nutritional status, independent mobility in DLA, accompanying diseases, psychological problems, and number of the equipment used by the patients together. We have obtained similar results with the literature. We have found a very strong correlation between the number of accompanying diseases and equipment used by the patients. It may be proposed from this result that home care patients use health equipment because of comorbid chronic diseases rather than an expectation to elevate life quality. Furthermore, malnutrition remarkably contributed to the development of DU while decreased mobility and existing psychological problems increased the risk for development of DU in our study. We have also observed in our study that decreased mobility increased the risk for malnutrition and these two factors negatively affected psychological conditions of the patients. Consequently, it is obvious that all these factors trigger the development of DU. Home care patients are generally individuals with limited level of independent mobility, insufficient self-care, and malnourishment. They experience psychological problems since they could not perform these functions. Therefore, all these factors contribute to the development of DU in those patients.
CONCLUSION
Face-to-face interviews and examinations were performed with 336 home care patients aged over 40 years old. SGA, MNA, DLA, and GDS scores of the patients were calculated. Demographic characters of the patients, number of accompanying diseases, and health equipment were also investigated. The factors which might affect DU and its development were analyzed. It was consequently seen that status of malnutrition, dependence level in DLA and the presence of psychological problems affect the development of DU. In addition, accompanying diseases and health equipment used by the patients at home had an impact on the development of DU. The logistic regression results show that the prediction model for the development of DU was successful at 90.4%. It is obvious that decreased capability of independent mobility in DLA increases the risk of malnutrition and these two assessments have a negative impact on the psychological status of the patients.
It is a requirement to increase daily physical activities of the patients and regulate their nutrition. Planning for home care patients should be performed under the control of health-care professionals. Their psychological status should be also followed up by the specialized staff. It would be reasonable to follow-up home care patients by experienced intensive care specialists, anesthetists, and internists since they especially need a systemic approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Pressure ulcer prevalence and risk factors during prolonged surgical procedures. AORN J. 2011;94:555-66.
- [Google Scholar]
- Admission Norton scale scores (ANSS) correlate with rehabilitation outcome and length in elderly patients with deconditioning. Arch Gerontol Geriatr. 2012;54:381-4.
- [Google Scholar]
- Incidence of pressure ulcers in a neurologic intensive care unit. Crit Care Med. 2001;29:283-90.
- [Google Scholar]
- Pressure ulcers in intensive care patients: A review of risks and prevention. Intensive Care Med. 2002;28:1379-88.
- [Google Scholar]
- Guideline implementation results in a decrease of pressure ulcer incidence in critically ill patients. Crit Care Med. 2007;35:815-20.
- [Google Scholar]
- Quality improvement program to reduce the prevalence of pressure ulcers in an intensive care unit. Am J Crit Care. 2008;17:328-34.
- [Google Scholar]
- Skin changes at life's end: SCALE ulcer or pressure ulcer? Br J Community Nurs. 2011;16:491-4.
- [Google Scholar]
- The perioperative management of the patient with pressure sores. Ann Plast Surg. 1983;11:347-56.
- [Google Scholar]
- Determination of risk for pressure ulcer development in bedridden patients and preventive measures that nurse's use for these patients. Turk J Res Dev Nurs. 2006;8:35-45.
- [Google Scholar]
- relation between album in levels and pressure sore in high-risk patients defined with Braden's risk assessment tool. Cumhuriyet Univ Nurs High Sch J. 2003;7:1-10.
- [Google Scholar]
- Prevalence of malnutrition on admission to four hospitals in England. The malnutrition prevalence group. Clin Nutr. 2000;19:191-5.
- [Google Scholar]
- Hospital malnutrition: The Brazilian national survey (IBRANUTRI): A study of 4000 patients. Nutrition. 2001;17:573-80.
- [Google Scholar]
- Desnutriçao hospitalar cinco anos apos o IBRANUTRI. Braz J Clin Nutr. 2003;18:65-9.
- [Google Scholar]
- The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235-9.
- [Google Scholar]
- Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr. 1997;66:1232-9.
- [Google Scholar]
- Treatment of protein-energy malnutrition in chronic nonmalignant disorders. Am J Clin Nutr. 2001;74:6-24.
- [Google Scholar]
- Beyond malnutrition screening: Appropriate methods to guide nutrition care for aged care residents. J Acad Nutr Diet. 2012;112:376-81.
- [Google Scholar]
- Inter-rater reliability of the subjective global assessment: A systematic literature review. Nutrition. 2013;29:350-2.
- [Google Scholar]
- Indications and limitations of the use of subjective global assessment in clinical practice: An update. Curr Opin Clin Nutr Metab Care. 2006;9:263-9.
- [Google Scholar]
- Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56:M366-72.
- [Google Scholar]
- Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN), et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415-21.
- [Google Scholar]
- Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):23-35.
- [Google Scholar]
- Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health. 2008;8:323.
- [Google Scholar]
- Physical disability and depressive symptomatology in an elderly population: A complex relationship. The Italian longitudinal study on aging (ILSA) Am J Geriatr Psychiatry. 2009;17:144-54.
- [Google Scholar]
- Effects of community-dwelling older adults' demographics and social, mental, and physical functions on depressive disorder. J Phys Ther Sci. 2013;25:463-6.
- [Google Scholar]
- Depression as a correlate of functional status of community-dwelling older adults: Utilizing a short-version of 5-item geriatric depression scale as a screening tool. J Nutr Health Aging. 2014;18:765-70.
- [Google Scholar]
- Depression and its association with functional status and physical activity in the elderly in Karachi, Pakistan. Asian J Psychiatr. 2015;14:46-51.
- [Google Scholar]
- A study of the relationship between depression symptom and physical performance in elderly women. J Exerc Rehabil. 2015;11:367-71.
- [Google Scholar]
- Depressive trajectories and risk of disability and mortality in older adults: Longitudinal findings from the health, aging, and body composition study. J Gerontol A Biol Sci Med Sci. 2016;71:228-35.
- [Google Scholar]
- Pressure ulcer prediction in older adults receiving home health care: Implications for use with the OASIS. Adv Skin Wound Care. 2003;16:132-9.
- [Google Scholar]
- Outcome and assessment information set data that predict pressure ulcer development in older adult home health patients. Adv Skin Wound Care. 2011;24:404-14.
- [Google Scholar]
- Reliability, validity, and factor structure of the geriatric depression scale in Turkish elderly: Are there different factor structures for different cultures? Int Psychogeriatr. 2000;12:163-72.
- [Google Scholar]






