Translate this page into:
A Comparative Study of Transdermal Buprenorphine and Oral Morphine in the Treatment of Chronic Pain of Malignant Origin
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Objective:
The study was designed to compare the efficacy and adverse effects of buprenorphine transdermal (TD) against oral morphine in pain management of cancer patient.
Methods:
A randomized open-labeled prospective study was done in palliative cancer pain clinic in a tertiary care medical college between August 2017 and January 2018, to compare the efficacy (pain assessed by VAS) and adverse events (CTCAEv4) between arm A, buprenorphine TD, (20 μg/h, extended 7 days formulation) and arm B, oral morphine (10mg immediate releasing formulation). Patients with solid tumour malignancies with VAS score >40 (moderate to severe pain) were included in study.
Results:
63 patients were analyzed. Commonest primary cancers were breast in females and head and neck in male individuals in both arms. Initial VAS score of arm A and arm B were 81.25 and 82.26 respectively. By 1st week, 11 arm A patients were relieved from pain. Another 17 patients of arm A became pain free by 2nd week, total dose of 40 μg/h. Only 4 patients needed 60 μg/h for pain relief. In arm B, 2 patients were relieved by 1 week with total 30mg/day morphine, 11patients were relieved with 60 mg/day by 2nd week and 12 patients with 90 mg/day. 6 patients were relieved with 120 mg/day dose at the end of 4th week. Nausea and constipation were stastically higher in Arm B compared to that of Arm-A.
Conclusions:
TD Buprenorphine had similar efficacy with oral morphine, with better toxicity profile and better compliance.
Keywords
Cancer pain
oral morphine
transdermal buprenorphine
INTRODUCTION
Pain is a prevalent symptom of cancer, affecting approximately 75% of people with advanced cancer[1] and almost all patients with end-stage disease.[2] The World Health Organization pain ladder is the cornerstone of pain management, with opioids playing a major role in the treatment of cancer pain. Morphine by mouth, in immediate-release or extended formulations, is the strong opioid of choice for cancer pain globally.
Morphine is a phenanthrene opioid receptor agonist. Bioavailability of oral morphine is 20%–40%. Its main effect is binding to and activating μ-opioid receptor in central nervous system. Activation of μ-opioid receptor is associated with analgesia, sedation, euphoria, physical dependency, and respiratory depression. It also has a weak kappa agonist activity. It is mainly metabolized to morphine-3-glucuronide (M3G) and morphine-6-glucuronide (M6G). While M6G has more potent analgesic activity than morphine, M3G might be responsible for side effects, especially hyperalgesia/allodynia and myoclonus seen after high-dose morphine administration. Both M3G and M6G accumulate in patients with renal failure. Hence, its use is restricted by renal failure which increases the adverse events (AEs) such as nausea, vertigo, constipation, and respiratory depression culminating in poor analgesic tolerance. Further, the limitation of morphine use is imposed by cultural barriers, unavailability, and political ideology.
Buprenorphine is a newly developed semisynthetic opioid derivative of thebaine having morphine-like pure μ-agonistic and antagonistic activities at kappa opioid receptor.[3] High lipid and water solubility, low molecular weight of 467 g/mol, and low melting point highlight the unique physicochemical properties of buprenorphine, making it a suitable candidate for transdermal (TD) administration.[4] It has been tested widely and extensively in postoperative and chronic pain[5678] and pain in myocardial infarction.[9] Use of buprenorphine in the sublingual or TD patch has been evaluated in cancer pain management, but data on comparative studies with oral morphine are limited. As oral morphine use is often restricted due to AEs, alternative opioids such as buprenorphine TD patch remain a good choice to circumvent the toxicities of severe nausea, vomiting, and constipation. Different TD strengths are available with 10 μg/h and 20 μg/h being available from our hospital pharmacy. The limited comparative studies had prompted us to design this study to compare the efficacy and adverse effects of buprenorphine TD (20 μg/h, extended 7-day formulation) to that of oral morphine (immediate-release formulation) in the pain management of cancer patient.
Aims and objectives
A randomized open-labeled prospective study was done at a palliative cancer pain clinic in a tertiary care medical college with the following objectives:
-
To compare the efficacy of TD buprenorphine with oral morphine
-
To compare the AEs of TD buprenorphine with oral morphine.
MATERIALS AND METHODS
Patients with solid tumor malignancies, suffering from moderate-to-severe chronic pain (visual analog scale [VAS] >40) attending our palliative care clinic, were included in our study according to the inclusion and exclusion criteria. Patients in the age group of 18–70 years, with duration of pain >3 months, were included in the study, provided that they had not received any opioid group of drugs over the past 3 months. In this regard, hospital records and physicians' prescriptions were scrutinized. Only analgesics allowed before the study entry were paracetamol, ibuprofen, and diclofenac sodium along with adjuvants such as dexamethasone, pregabalin, and benzodiazepines. Patients were needed to understand VAS and respond appropriately. Minimum life expectancy of >2 months along with no signs of neurological deficits was another inclusion criterion for the study. While all patients recruited were entitled to give consent, patients' caregivers were also counseled regarding potential toxicities arising from drugs' administration and their remedies. Patients recruited in this study were randomized into two arms using computer-based randomization with 1:1 ratio.
The patients in study arm A (experimental arm) received TD buprenorphine (20 μg/h, over a period of 7 days); replaced every 7 days. Patients in Arm B (control arm) received oral morphine (immediate-release formulation) 10 mg/tab in 4 hourly divided dose, with dose modifications allowed every 7 days.
Additional drugs allowed were paracetamol (1 g every 6 h, maximum of 4 g daily dose in individuals with normal liver function tests), diclofenac sodium (50 mg QDS), lorazepam (1 mg), and short-course dexamethasone (8 mg BDPC for 3–4 days) and other adjuvants such as pregabalin or amitriptyline as per requirements. Both the drugs were available through hospital pharmacy with appropriate permission from the government health and narcotic departments.
The patients were assessed by the VAS weekly for at least four observations. For Arm A patients, if subsequent VAS scores were >40, then the dose of TD buprenorphine was increased by 20 μg/h every week. For Arm B patients, oral morphine was increased by 30 mg/day if VAS scores were >40.
The occurrence of AEs was measured in both the arms using Common Terminology Criteria for Adverse Events v4.1. Statistical analysis was done using Statistical analysis was done using R software v3.5.0, (Vinnea, Austria).
RESULTS
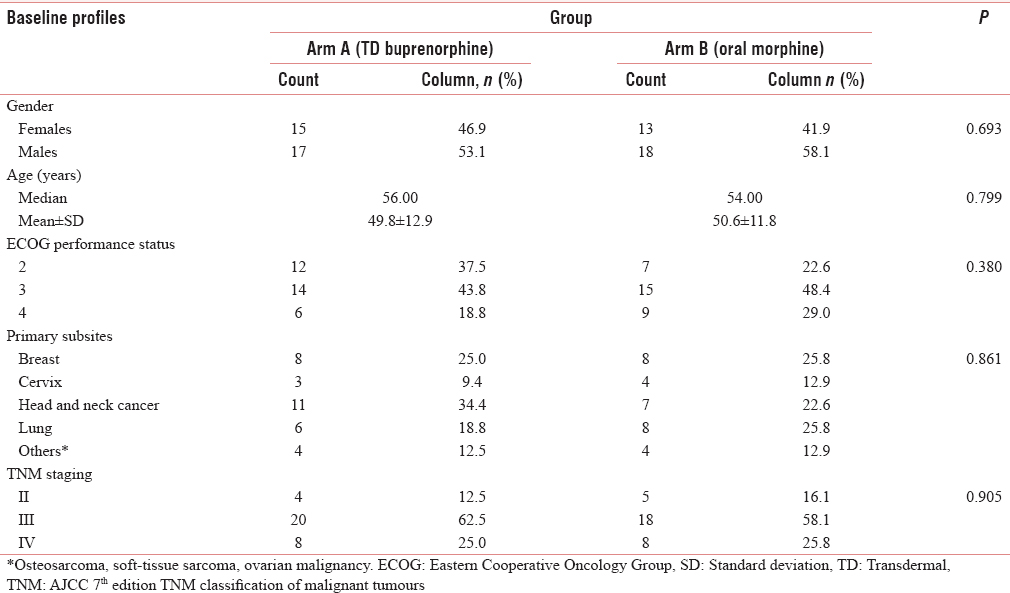
The study was conducted between August 2017 and January 2018. A total of 63 patients fulfilling our selection criteria were analyzed. Baseline parameters were comparable [Table 1]. The most common sites of primary cancer were the breast in females and the head and neck in males in both the arms. Baseline VAS scores were comparable in both the arms. The initial VAS scores of Arm A and Arm B were 81.25 and 82.26, respectively [Table 2]. At the end of the 1st week, 11 Arm A patients were relieved from pain (VAS ≤40 mm) and the rest needed an increase in the dose of TD buprenorphine by 20 μg/h. Another 17 patients of Arm A became pain free at the end of the 2nd week with a total dose of 40 μg/h. Only four patients needed 60 μg/h dose to get relief from the pain.

In Arm B, two patients were relieved by 1 week with a dose of 30 mg/day of oral morphine. Eleven patients were relieved by 60 mg/day at the end of the 2nd week and were stable with this dose. Twelve patients were relieved with 90 mg/day at the end of the 3rd week and were stabilized with that dose. Six patients were relieved with 120 mg/day dose at the end of the 4th week and were stabilized with that dose of oral morphine.
Common side effects in both the arms were constipation and nausea. Both nausea and constipation were statistically higher in Arm B compared to that of Arm A. However, the toxicities were manageable, and no patient was discontinued from the study due to toxicity [Table 3].

Our study was not designed to measure changes in quality-of-life parameters due to narcotic administration, which is one of the drawbacks of our study.
DISCUSSION
The benefits of sublingual and TD buprenorphine in the treatment of chronic cancer pain were demonstrated in a number of randomized trials as well as cohort studies.[5678] The TD formulation offered several advantages such as noninvasive and controlled release and stable plasma concentration of buprenorphine. In the year 2001, the buprenorphine TD delivery system was introduced to deliver the drug at 35, 52.5, and 70 μg/h for the treatment of chronic cancer and noncancer pain. Later on, 10 μg/h and 20 μg/h “7-day extended release” formulations were commercially available. There are conflicting reports on “daily morphine equivalent dose” of TD buprenorphine dose, with some studies mentioning TD buprenorphine to be 70–115 times more potent than PO morphine.[10111213]
Poulain et al. in a randomized multicentric, double-blinded, placebo-controlled trial showed efficacy and safety of TD buprenorphine (70 μg/h) in 289 patients with severe cancer pain. Patients were randomized to receive either buprenorphine or placebo patches during the 14-day double-blind phase. The superior efficacy of buprenorphine during the double-blind phase was statistically significant despite the high placebo effect of the patch. This was also confirmed by secondary end-points such as pain intensity and consumption of rescue medicine. AEs were comparable in both arms.[14]
Efficacy of TD and sublingual buprenorphine has been proven in numerous trials for cancer and noncancer pain.[15161718] In a multicentric Polish trial, TD buprenorphine was evaluated for efficacy and AEs in patients with moderate-to-severe cancer pain and in patients with severe, nonmalignant pain in the course of other diseases, after failure with nonopioid analgesics. The common dosage was TD buprenorphine (Transtec® 35, 52.5, and 70 μg/h).
Cancer patients accounted for 81% of the 4030 patients. Mean pain intensity on VAS (0–100 mm) gradually decreased from a mean value of 62.5 mm at the baseline visit to the value of 16.5 mm at the final study assessment. Although no specific mention was made on benefits of cancer patients, this postmarketing study definitively confirmed high efficacy and good tolerability of buprenorphine.[19]
In our study, we also found similar outcome in both the arms, the dose stabilized within 4 weeks with 1 week earlier in Arm A. The global score of quality of life also increased in both arms, but more in Arm A. The toxicities were mainly nausea, vomiting, and constipation in both arms and statistically significantly lower in Arm A.
Pace et al. compared TD buprenophine with oral morphine in which it was showed that patients receiving buprenorphine had significant physical pain relief as well as improvement in mental health and lower interference with sleep than those in morphine group. The toxicities (nausea, vertigo, and constipation) were significantly lower in TD buprenorphine group.[2]
In one of the studies, 42 (21% with cancer) patients receiving high-dose morphine (>120 mg/day) were switched to TD buprenorphine because of inadequate analgesia and severe adverse effects. Improved overall satisfaction and quality of sleep (good/very good increased from 14% to 74%, P < 0.005) highlighted pain relief which increased from 5% to 76% (P < 0.001). Only 5% of patients reported insufficient relief.[20]
CONCLUSION
In comparative studies, buprenorphine was found efficacious against tramadol, fentanyl, and even oral morphine with a better safety profile. The patients' acceptance was also better with TD formulation. Our trial might be considered as a pilot study being first of its kind in India paving the way for promising future for cancer pain management where morphine administration still poses a problem for palliative care specialists.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Prevalence of under treatment in cancer pain. A review of published literature. Ann Oncol. 2008;19:1985-91.
- [Google Scholar]
- Buprenorphine in long-term control of chronic pain in cancer patients. Front Biosci. 2007;12:1291-9.
- [Google Scholar]
- Opioid analgesics. In: Hardman JG, Limbird LE, Gilman AG, eds. Goodman and Gilman's: The pharmacological basis of therapeutics (10th ed). New York: McGraw-Hill; 2001. p. :569-619.
- [Google Scholar]
- Buprenorphine and the transdermal system: The ideal match in pain management. Int J Clin Pract Suppl. 2003;133:9-14.
- [Google Scholar]
- Buprenorphine: A new potent long-acting synthetic analgesic. Comparison with morphine. Br J Anaesth. 1977;49:251-5.
- [Google Scholar]
- Transdermal buprenorphine in the treatment of chronic pain. Expert Rev Neurother. 2005;5:315-23.
- [Google Scholar]
- Role of buprenorphine in acute postoperative pain. Rev Méd Hosp Gen México. 2016;79:174-80.
- [Google Scholar]
- Randomised trial comparing buprenorphine and diamorphine for chest pain in suspected acute myocardial infarction. Br Med J. 1979;2:300-2.
- [Google Scholar]
- Equipotent doses of transdermal fentanyl and transdermal buprenorphine in patients with cancer and non-cancer pain: Results of a retrospective cohort study. Clin Ther. 2005;27:225-37.
- [Google Scholar]
- Challenging the equipotency calculation for transdermal buprenorphine: Four case studies. Int J Clin Pract. 2008;62:152-6.
- [Google Scholar]
- Efficacy and safety of transdermal buprenorphine: A randomized, placebo-controlled trial in 289 patients with severe cancer pain. J Pain Symptom Manage. 2008;36:117-25.
- [Google Scholar]
- Analgesic efficacy and tolerability of transdermal buprenorphine in patients with inadequately controlled chronic pain related to cancer and other disorders: A multicenter, randomized, double-blind, placebo-controlled trial. Clin Ther. 2003;25:150-68.
- [Google Scholar]
- Efficacy and tolerability of a new opioid analgesic formulation, buprenorphine transdermal therapeutic system (TDS) in the treatment of patients with chronic pain. A randomised, double blind, placebo-controlled study. Pain Clin. 2003;15:193-202.
- [Google Scholar]
- Transdermal buprenorphine in cancer pain and palliative care. Palliat Med. 2006;20:s25-30.
- [Google Scholar]
- Transdermal buprenorphine in the treatment of chronic pain: Results of a phase III, multicenter, randomized, double-blind, placebo-controlled study. Clin Ther. 2004;26:1808-20.
- [Google Scholar]
- Transdermal buprenorphine in the treatment of cancer and non-cancer pain-the results of multicenter studies in Poland. Pharmacol Rep. 2011;63:935-48.
- [Google Scholar]
- Opioid rotation from high-dose morphine to transdermal buprenorphine (Transtec) in chronic pain patients. Pain Pract. 2007;7:123-9.
- [Google Scholar]






