Translate this page into:
An Observational Study to Assess the Socioeconomic Status and Demographic Profile of Advanced Cancer Patients Receiving Palliative Care in a Tertiary-Level Cancer Hospital of Eastern India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Socioeconomic status (SES) comprises of not just gross income but also educational qualification, financial security and individual perceptions of social status and class. It has been observed that people with low SES have less access and utilization of palliative care services. With this background, this observational study was carried out at SGCCRI to assess and evaluate the SES of patients attending the palliative care department and analyse the major social concerns of patients in the last days of life.
Objectives:
Assessment of socio- economic status and demographic profile of patients with advanced cancer receiving palliative care.
Materials and Methods:
From May 2017 to October 2017 we assessed the demographic features and socio-economic status of 80 advanced cancer patients receiving palliative care by interviewing them face to face with the help of a self designed social assessment sheet.
Results:
A total of 80 patients consented to be interviewed with regards to assessment of their socio-economic conditions. Majority were male patients (64%) with the highest percentage in the age group of 60-70years (33%). 38% of the patients interviewed were from rural surroundings. Only 38% of the patients had completed their basic education. Approximately 30% of the patients interviewed had income less than 1lakh/month while majority (>60%) had income in the bracket of 1lakh- 2lakh. In 30% of cases, the patient was the sole earner in the family.
Conclusion:
It was observed that majority of patients and their family were constrained with regards to financial resources and large percentage of patients had social insecurity with respect to future of family members.
Keywords
Demographics
palliative care
socioeconomic status
INTRODUCTION
The present-day global incidence of new cases of cancer is 14.1 million per year, and the number of cancer-related deaths is 8.2 million deaths/year.[1] India being the second most populous country backs the global data with 2.5 million people living with cancer, 0.7 million new cases diagnosed with cancer, and 0.55 million cancer-related deaths annually.[2] Medical science has dominated the field of oncology in the last few decades with advances in cancer therapeutics and the introduction of screening for early detection of certain cancers.[3] For an increasing proportion of cancer patients, survival becomes a way of life. However, increased survival is associated with adversities such as chemotoxicity, socioeconomic insecurities, increased dependence on caregivers, and social isolation. A cancer diagnosis may threaten any of patient's responsibilities at home, workplace, and recreationally which may result in a range of potential social problems which are an underlying reflection of life and socioeconomic status (SES) of individual patients.[4] Assessment of social concerns is, however, not considered a routine part of standard cancer care as the primary preoccupation of the oncology team is usually to emphasize on maintaining survival.[5] Although many patients develop good coping strategies to having had a cancer diagnosis and treatment,[6] there are others who may struggle and who would benefit from good psychosocial support.[7]
Studies from western countries found that SES impacted inequities in healthcare system with low SES patients having less access to medical resources and high-volume service providers.[8] A growing body of literature suggests a persistent relationship between SES and health status with SES influencing survival in several common cancers.[9]
Detection and characterization of social problems have been found to improve care of cancer patients and result in improved quality of life. With this background, this study aims to identify the character and prevalence of social problems experienced by cancer patients.
SUBJECTS AND METHODS
This was a prospective, single-institutional, observational study carried out in the Department of Palliative Care at Saroj Gupta Cancer Centre and Research Institute (SGCCRI), Kolkata.
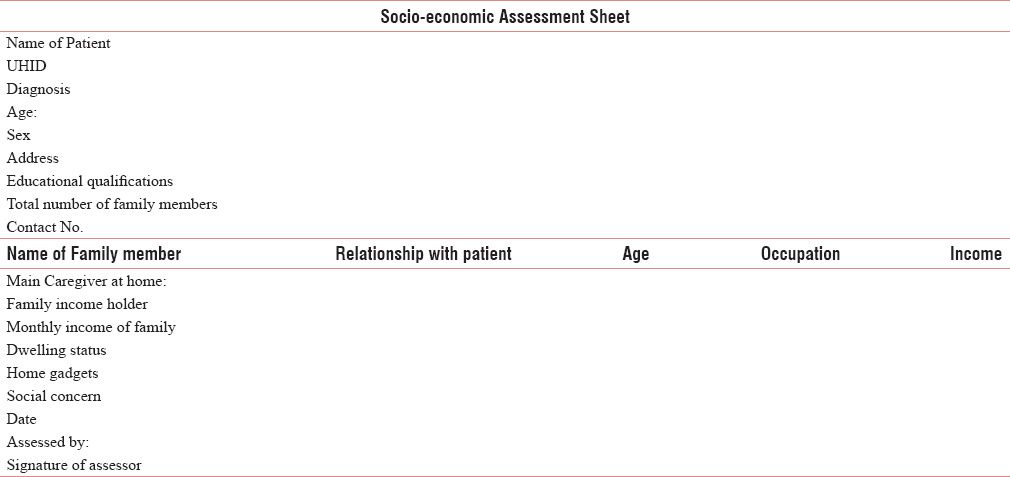
Patients were invited to participate by a palliative care consultant in outpatient clinics, and consenting patients were recruited for assessment and analysis. Information regarding the demographics and SES was collected from the medical notes and patients. An interview guide was designed [Table 1] incorporating general introductions followed by the question format.
Eighty patients were analyzed over a period of 7 months from July 2017 to December 2017. Patients with advanced cancer above 18 years of age attending palliative care outpatient department (OPD) and consenting to participate in the study were included. Patients were assessed using a self-designed social assessment sheet and modified Kuppuswamy scale to determine SES in face-to-face interviews during their presentation to palliative care OPD.[10]
Modified Kuppuswamy scale using education, occupation, and monthly family income to calculate the socioeconomic scale was used, and the patients were scored into five different socioeconomic classes based on their respective scores.[11]
Ethical consideration
Subjects were explained the purpose of the study, and those who gave consent to participate in the study were interviewed to collect the desired information on the designed assessment sheet. In case of respondents who were very sick, assent was taken from primary caregivers. Confidentiality of responses was assured.
RESULTS
Of the 80 patients interviewed, 39% (n = 31) belonged to the age group of 60–70 years followed by 24% being in the age bracket of 50–60 years and minimal representation from adolescents and children. Sixty-four percent of the patients (n = 51) were males while 36% (n = 29) were females [Table 2]. Approximately 54% of the participants stayed >25 km from the hospital and for whom communication to the hospital at regular intervals was a concern.

Of the type of cancer affected, 37.5% had cancers of gastrointestinal tract followed by 20% afflicted with gynecological cancers, 12.5% each of head and neck and thoracic cancers, and the remaining being genitourinary, brain, and bone cancers [Table 3].

There was an equal mix of patients from rural (n = 31) and urban areas (n = 33) with a minority 20% of patients (n = 16) from semi-urban locales of Kolkata. Majority of the participants of the study had attained basic level of education of up to matriculation (n = 29) [Table 2].
Applying the modified Kuppuswamy scale, 61% of participants had a score of <15 belonging to lower middle and lower SES, 26.25% had a score between 16 and 25 and belonged to the upper middle class, while 12.5% had scores between 26 and 29 and belonged to upper class of the society [Table 4]. In 30% of the patients and families studied, patient himself/herself was the sole bread earner of the family [Table 4].

The major social problems were listed as follows:
-
Insecurities regarding family members future in 32.5% of participants
-
Financial insecurity in 26.25% of participants
-
Maintaining independence in 12.5% of participants
-
Progression of disease in 10% of participants
-
Unable to overcome the psychological stress of being inflicted with a life-limiting condition in 18% of participants.
DISCUSSION
The study gives us a brief understanding regarding the SES of cancer patients presenting to palliative care OPD of SGCCRI, Kolkata. Social problems that dominated the study scenario were (a) future insecurities for family; (b) financial insecurities; (c) maintaining independence; and (d) fear regarding disease progression and terminality of disease.
These corroborated in most of the concerns with a study conducted by Wright et al.[5] Our study contradicted with Wright et al. and Keller and Henrich.[512] in view of gender inequalities in which female representation was higher as compared to male representation. It was observed that patients with low SES had reduced coping to psychological distress as compared to patients with high SES and required referral to a psychologist which corroborated with similar findings from a study conducted by Schock,[13] who linked higher income with access to better healthcare and more resources with which to make better health decisions.
Our study has certain limitations which must be considered while interpreting the results. We used data from a single cancer hospital which caters to a particular area and not entirely representative of the entire region. As a result, the demographic and socioeconomic characteristic of the cancer cases from this hospital may be different from the nationwide data.
CONCLUSION
In this population-based observational study, it was observed that majority of patients and their families were constrained with regard to financial resources and large percentage of patients had social insecurity with respect to future of family members after patient's death. In a subgroup of patients, concern regarding maintaining independent activities of daily living was major distress. Participants of low SES were found to have difficulties in coping with their diagnosis and predicament and required intervention by a psychologist to relieve their anxiety and psychological distress. Furthermore, in a large percentage of patients, the patient himself/herself was the sole earner of the family and the diagnosis of cancer brought economic crisis to patient's family and thereby leading to financial insecurities.
Our study provides a correlation between SES and level of coping mechanisms of patients suffering from advanced cancer. This provides direction to screen patients for social and psychological distress and address them at the appropriate time.
Further studies in a larger population of patients to clarify and establish this correlation may be performed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Available from: http://www.whoint/mediacentre/factsheets/fs297/en
- Available from: http://www.cancerindia.org.in/statistics
- Pearce N Why Study Socioeconomic Factors and Cancer ARC Sci Publ. 1997;138:17-23. Review PMID: 9353660
- Psychological, social, and behavioral issues for young adults with cancer. Cancer. 2011;117:2289-94.
- [Google Scholar]
- Assessment of and intervention for psychosocial problems in routine oncology practice. Br J Cancer. 1995;72:229-35.
- [Google Scholar]
- Low socioeconomic status is associated with more aggressive end-of-life care for working-age terminal cancer patients. Oncologist. 2014;19:1241-8.
- [Google Scholar]
- Race, socioeconomic status, treatment, and survival time among pancreatic cancer cases in California. Cancer Epidemiol Biomarkers Prev. 2007;16:546-52.
- [Google Scholar]
- Modified Kuppuswamy's socioeconomic scale: Social researcher should include updated income criteria, 2012. Indian J Community Med. 2013;38:185-6.
- [Google Scholar]
- Manual of socio economic status scale (urban) Delhi: Manasayan 1981
- Illness-related distress: Does it mean the same for men and women? Gender aspects in cancer patients distress and adjustment. Acta Oncol. 1999;38:747-55.
- [Google Scholar]
- Socioeconomic Status and Cancer Outcomes in the United States: Examining Geographic Dissidence in Incidence and Mortality Rates 2016






