Translate this page into:
Cluster Analysis of Symptoms of Bangladeshi Women with Breast Cancer
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Breast cancer (BC) patients may experience multiple symptoms due to the disease itself, cancer treatment or combination of both.
Aim:
The aim of the present study was to express multiple symptoms experienced by the patients with BC as clusters.
Methods:
This was a retrospective study. We examined symptom profiles of 120 patients with BC who attended the Centre for Palliative Care, Bangabandhu Sheikh Mujib Medical University in Dhaka, Bangladesh, from January 2009 to December 2013. We included all case sheets of BC patients, which had documentation of needed information. Following symptoms were analyzed: pain, nausea, loss of appetite, constipation, weakness, cough, breathlessness, sleeplessness, lymphedema, sadness, anxiety, and depression. Hierarchical cluster analysis was used to identify the natural groupings within the set.
Results:
We could identify three clusters, namely (1) “neuropsychiatric,” (2) “gastro-respiratory,” and (3) “miscellaneous” symptom clusters. The symptoms in cluster 2 comprised of cough, breathlessness, nausea, and constipation. Cluster 1 was characterized by pain, depression, anxiety, weakness, sleeplessness, and loss of appetite. Cluster 2 was comprised of cough, breathlessness, nausea, and constipation. Cluster 3 consisted of two symptoms lymphedema and sadness. The results revealed that the multiple symptoms of patients with BC experienced had been clustered together. Neuropsychiatric symptoms and weakness formed a significant strong relationship with each other.
Conclusion:
Knowledge obtained from this study could be beneficial for better understanding, assessment, and management of symptom clusters in women with BC. It may also help patients to plan ahead for them to seek management of concurrent symptoms to improve their quality of life.
Keywords
Breast cancer
cluster analysis
hierarchical
symptom cluster
INTRODUCTION
Worldwide breast cancer (BC) is the most common cancer of women.[1] BC is also the most common cancer in Bangladesh.[2] BC patients may experience multiple symptoms at a time due to the disease itself, treatment or combination of both.[3] The study follows definitions of “symptoms” and “clustered symptoms” after a literature review. Subjective perception of disease is known as “symptom.”[4] Symptoms may be complex and clustered in nature.[5] Aggregations of three or more symptoms that may or may not be originated from a single source are known as “clustered symptoms.” Sufferings due to multiple symptoms are a source of reduced quality of life (QoL) and functional status in patients with BC.[67] Previous studies have found that symptoms of fatigue, depression, sleep disturbances, and pain are prevalent across different stages of BC and treatment.[891011121314]
Symptoms such as pain, fatigue, sleep alterations, depression, and loss of appetite were identified by previous studies as most common, associated or highly prevalent symptoms of BC patients.[15161718] Symptom clusters may affect each other and may trigger other symptoms to affect QOL.[192021] The identification of meaningful subgroups of patients within this disease/particular to the disease is therefore important as these groups may represent different etiological and pathophysiological entities and they may require different treatment approaches.[22] Symptom clusters in Bangladeshi women with BC are little known. The aim of this study was to investigate the existence of natural symptom clusters of women with BC systematically.
METHODS
This was a retrospective study. Hospital notes and case sheets were screened to identify patients with BC primary BC patients registered with the Centre for Palliative Care over a 5 years' period between January 2009 and December 2013, in the only medical university in Bangladesh to include in the study. The inclusion criteria were women aged 18 years or above diagnosed with BC of any stage with or without ongoing definitive treatment. The exclusion criteria included a medical history of cancer or immune-related disease (i.e., multiple sclerosis, HIV, and lupus) or not having a histopathologically confirmed breast malignancy.
At the time of first consultation, patients demographic and other symptoms were documented after thorough assessment of the patient in a case sheet with a total of 91 variables (22 demographic and 69 clinical) by a team that include one medical doctor with 6 weeks' training in palliative medicine and one nurse trained in 6 weeks' palliative nursing. The University Institutional Review Board approved this study.
All analyses were carried out using SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. (Chicago, USA). Baseline data were analyzed using parametric statistics and are expressed as mean values. Using the whole data set, Pearson correlation coefficients were used to explore linear relationships between different continuous variables.
A hierarchical cluster analysis was used to classify data based on variables according to physical and psychological symptoms. The hierarchical cluster analysis method is explanatory, and we had no preconceived ideas about how variables would cluster together. Euclidean distance measure was used in the process. Similar symptoms were put by the technique into the same group in a hierarchical way, so that, most similar two symptoms are first put into a group. The algorithm iteratively estimates the cluster means and assigns each variable to the cluster. The validity of the three subgroups solution was explored by comparing subgroup membership across physical and psychological symptom measures, using ANOVA. Statistical significance was defined as P < 0.05.
RESULTS
Sample characteristics
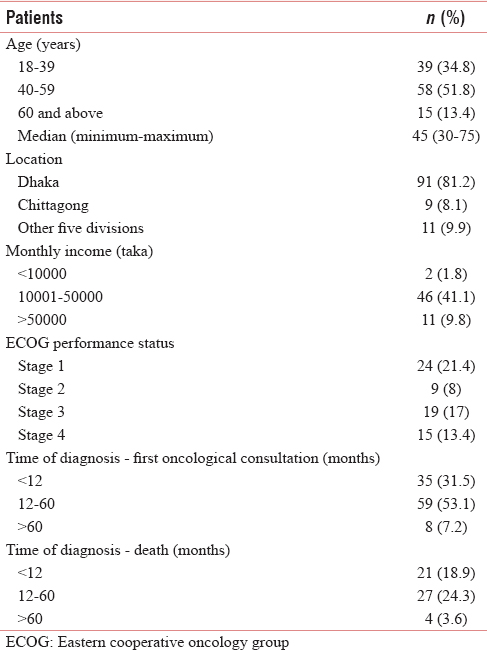
A total of 120 case sheets of carcinoma breast patients were selected for this study. Among those case sheets, eight were discarded because the patients did not have any histopathological evidence on admission. These patients underwent fine-needle aspiration cytology after admission to have diagnosis. Data are therefore presented on 112 patients. No significant difference in the baseline measures of physical, psychological symptoms or demographic variables between those patients whose case sheets were discarded for this study. The initial dataset included 120 individuals ranging in age from 17 to 80 years. Complementary therapy was taken by 40 (35.7) patients, which include Ayurveda, homeopathy, or religious approach. Among the patients, 93 (83%) of the patients had definitive therapy. Forty-seven patients (44%) had emotional problems. The most common conditions were depression, n = 28 (28%) and anxiety states, n = 32 (30%).
Time since diagnosis to the first consultation ranged from 3 days to 143 months, with a mean of 25 months (standard deviation [SD] = 25.3). Time since diagnosis to death ranged from 8 days to 145 months, with a mean of 28 months (SD = 27.67). Among the study group, 39% of the women had Stage II BC. Other clinical characteristics are summarized in Tables 1 and 2.
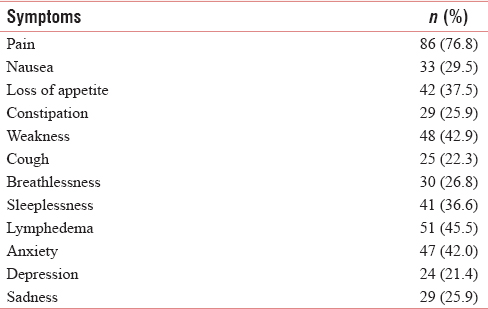
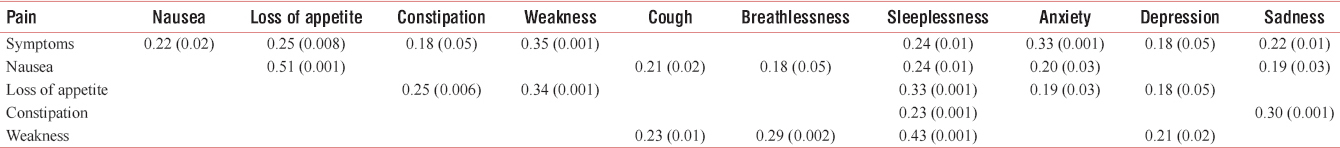
Significant medium correlation between pain with weakness and anxiety, large correlation between nausea with loss of appetite and a large correlation was found with weakness and sleeplessness. Other significant correlations are shown in Table 3.
Cluster analysis
Hierarchical cluster analysis grouped together related symptoms, based on the observed similarities between them. Using the agglomerative cluster approach, a dendrogram was generated. Figure 1 shows the total process of joining individual points to one big cluster.
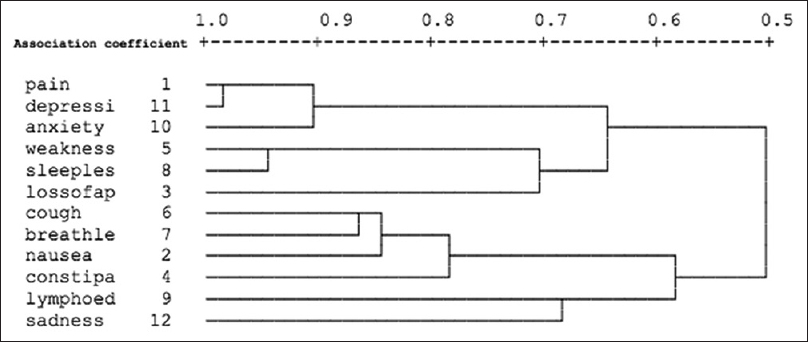
- Results of cluster analysis
The results of cluster analysis with matrix of association coefficients between individual symptoms are shown in Table 4. Pain, depression, and anxiety were associated most closely. The association coefficient between pain and depression, anxiety, and weakness was 0.917, 0.875, and 0.708, respectively. Furthermore, weakness and sleeplessness formed a relatively tight cluster with a distance of 0.875. Loss of appetite was joined next to this cluster, with an association coefficient of 0.625. The next symptoms included in this cluster were cough, breathlessness, nausea, and constipation. Thus, we could identify three symptom clusters. Cluster 1 was characterized by pain, depression, anxiety, weakness, sleeplessness, and loss of appetite. This cluster was named as “neuropsychiatric” symptom cluster. The symptoms in cluster 2 comprised cough, breathlessness, nausea, and constipation.
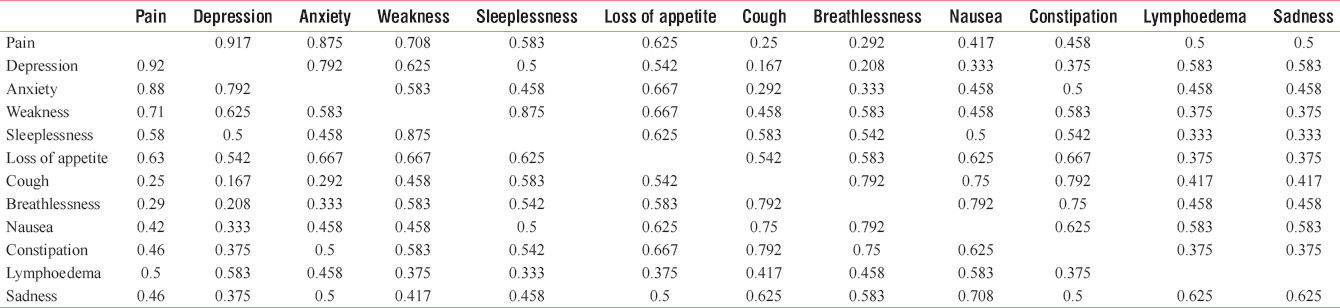
This cluster was named as “respiratory-gastrointestinal” symptom cluster. Cluster 3 consisted of two symptoms lymphedema and sadness, and this was named as “miscellaneous” symptom cluster.
A one-way between-groups multivariate analysis of variance was performed to investigate cluster differences in physical and psychological symptoms. Pain, nausea, loss of appetite, constipation, weakness, cough, breathlessness, sleeplessness, lymphedema, anxiety, depression, and sadness were used as dependent variables. The independent variable was a group containing three clusters. Preliminary assumption testing was conducted to check for normality, linearity, univariate and multivariate outliers, homogeneity of variance-covariance matrices, multicollinearity, with no serious violations noted. There was a statistically significant difference between Group 1, Group 2, and Group 3 on the combined dependent variables, F (11, 11) =2.76, P = 0.011; Wilks' Lambda = 0.07; partial eta squared = 0.95. When the results for the dependent variables were considered separately, differences to reach statistical significance, using a Bonferroni adjusted alpha levels of 0.302, 0.412, and 0.20, was weakness, F (2, 21) = 5.98, P = 0.009, partial eta squared = 0.36; sleeplessness F (2, 21) = 9.05, P = 0.001, partial eta squared = 0.46 and lymphedema F (2, 21) = 4.00, P = 0.03, partial eta squared = 0.27. An inspection of the mean pain scores indicated that cluster 1 had slightly lower levels of pain (confidential interval = 0.78, SD = 0.44) than other two groups (C2 = 1.00, SD = 0.00) and (C3 = 1.00, SD = 0.00).
DISCUSSION
There are several important findings derived from this retrospective analysis that may be used to inform future studies. We chose a set of symptom clusters of pain, nausea, loss of appetite, constipation, weakness, cough, breathlessness, sleeplessness, lymphedema, sadness, anxiety, and depression based on the previous literature. A longitudinal study discovered the symptoms of BC before surgical intervention and also to know the impact of these symptoms on 94 patients.[1] It was found that 35% of the females with BC had pain, 32% had fatigue, sleep disturbances affected 25.5%, and 11% had depression. QoL was measured with Hospital Anxiety and Depression Scale, Insomnia Severity Index, Functional Assessment of Cancer Therapy-Fatigue; and Brief Pain Inventory and European Organization for research and treatment. Fatigue showed a moderate correlation with emotional functioning and a weak correlation with physical and social functioning. A secondary analysis of 128 women with BC (Stages I and II) was undertaken at 4 weeks after lumpectomy or mastectomy, before receiving their first dose of chemotherapy.[5] This time point was selected because it provided an adequate duration of time after surgery for return of baseline immune parameters. They chose a well-described symptom cluster of fatigue, depression, pain, and sleep disturbance, a majority of the sample had very low symptom scores for both pain and sleep disturbances. In our study, about 77 (68.8%) of the participants had undergone surgery, 88 (78.6%) had completed or undergoing chemotherapy schedules, and 60 (53.6%) had radiotherapy. We found that pain (76.8%) had the highest scores among all symptoms.
We excluded symptoms with extremely low scores. Although the pain was measured with the numerical scale, other symptoms were not measured with any measurement scale. Therefore, we could not assign any clinical significant cutoff score for each symptom, however, we decided to include the symptoms according to their scores to increase the homogeneity of the sample in terms of their symptom experience. We decided to include symptoms which had scores >20%.
Another study with a total of 320 women with BC undergoing chemotherapy were ranged in age from 17 to 68 years, with a mean of 47.3 years (SD = 8.8), majority had Stage II BC.[22] This study revealed that symptom clusters were not identical across symptom dimensions. In addition, symptom clusters revealed in this study are more likely treatment-related symptom clusters, particularly gastrointestinal and fatigue-related symptoms. Gastrointestinal symptoms (such as nausea, vomiting, and lack of appetite) and fatigue-related symptoms were reported as common adverse effects of the standard chemotherapy regimen using the combination of cyclophosphamide, methotrexate, 5-FU, and doxorubicin. Gastrointestinal and fatigue are identified as clusters in BC patients undergoing chemotherapy in two studies.[515] Our study identified neuropsychiatric and weakness as clusters in BC patients. The findings from this study supported previous studies that symptom clusters existed in this group of women across cultural studies. The differences in the structures of symptom clustering might be from the differences between the sample characteristics or the methodology used in each study.
Limitations
There are three major limitations of the study. First, approximately 40% of the case sheets did not include everyday cognition (ECOG) measurements. Although they appeared similar to those who had ECOG grades in terms of gastrointestinal symptoms and psychological profile, subtle differences could not be excluded from the study. Second, the study was carried out in a tertiary Centre, and therefore, the finding should not be generalized to primary care or community subjects with carcinoma breast. Third, all the symptoms were not measured using reliable and validated scales. The drawback of this is that we could have failed to recognize clinical details that might be added to the research. The way forward may be to target to use validated measurement scales for different symptoms and also to develop specific treatments for subgroups.
CONCLUSION
The current study provided empirical evidence that Bangladeshi BC patients experience multiple symptom clusters. Future study could be done to verify these three symptom clusters and identify underlying mechanism. The findings suggested that these women experienced multidimensional symptoms together that were interrelated and aggregated in three major groups. Health professionals could pay more attention to more specific assessment and management to these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Symptoms, clusters and quality of life prior to surgery for breast cancer. J Clin Nurs. 2014;23:2491-502.
- [Google Scholar]
- 2010. Cancer Incidence and Mortality Worldwide: IARC Cancer Base GLOBOCAN. Available from: https://www.iarc.fr/en/media-centre/iarcnews/2010/globocan2008.php
- Living with breast cancer: Thai women's perspective. Thai J Nurs Res. 2004;8:208-22.
- [Google Scholar]
- Differences in symptom clusters identified using occurrence rates versus symptom severity ratings in patients at the end of radiation therapy. Cancer Nurs. 2009;32:429-36.
- [Google Scholar]
- Symptom, symptom experiences, and symptom distress encountered by women with breast cancer undergoing current treatment modalities. Cancer Nurs. 2005;28:382-9.
- [Google Scholar]
- Factors associated with fatigue after surgery in women with early-stage invasive breast cancer. Oncologist. 2013;18:467-75.
- [Google Scholar]
- Trajectories of sleep disturbance and daytime sleepiness in women before and after surgery for breast cancer. J Pain Symptom Manage. 2013;45:244-60.
- [Google Scholar]
- Breast cancer wait times: The journey from detection to adjuvant treatment. J Clin Oncol. 2010;28:60-70.
- [Google Scholar]
- Presurgery psychological factors predict pain, nausea, and fatigue one week after breast cancer surgery. J Pain Symptom Manage. 2010;39:1043-52.
- [Google Scholar]
- Predictors of depressive symptoms 12 months after surgical treatment of early-stage breast cancer. Psychooncology. 2009;18:1230-7.
- [Google Scholar]
- An explanatory model of fatigue in women receiving adjuvant breast cancer chemotherapy. Nurs Res. 2001;50:42-52.
- [Google Scholar]
- Fatigue in breast cancer survivors: Occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743-53.
- [Google Scholar]
- Symptom clusters in oncology patients and implications for symptom research in people with primary brain tumors. J Nurs Scholarsh. 2004;36:197-206.
- [Google Scholar]
- Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97:2919-25.
- [Google Scholar]
- Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nurs. 2005;28:219-25.
- [Google Scholar]
- Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28:465-70.
- [Google Scholar]
- Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999;22:185-94.
- [Google Scholar]
- Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: A cluster analysis. Oncol Nurs Forum. 2006;33:E79-89.
- [Google Scholar]






