Translate this page into:
Empowering Nurses in Providing Palliative Care to Cancer Patients: Action Research Study
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Chronic diseases such as cancer would lead to various health needs in patients and their families. To meet needs, developing new educational nursing courses is necessary. Therefore this study was conducted to empower nurses through designing and conducting short-term educational courses for training palliative care nurses.
Materials and Methods:
This study was a community-based action research which was conducted at Isfahan hospitals that provide services for cancer patients during 2015 at four stages (planning, acting, reflection, and evaluation). Participants (33 samples) included nurses, head nurses, managers of nursing services, nursing professors and professors of oncology department. Data were gathered through individual and group interviews and analyzed using content analysis.
Results:
Data analysis resulted in 3 categories of "professional development of nursing in palliative care" which included subcategories of: knowledge-based performance and positive change in attitude, "obstacles to provide palliative care" with subcategories of: insufficient professional responsibility, insufficient ability in managing some of patients’ symptoms and inappropriate interaction between nurses and physicians and "strategies for improving provision of palliative care" with subcategories of: improving the interactions between physicians and nurses, continuous trainings for palliative care and the necessity of developing palliative care in the country.
Conclusions:
To facilitate the process of providing palliative care to cancer patients, necessary actions and measures must be conducted including improvement of interaction between the members of health team, organizing continuing educational courses on palliative care and development of providing palliative care all over the country by managers of health centers.
Keywords
Action research
cancer
educational program
holistic care
nurse
palliative care
INTRODUCTION
Nursing, as a scientific discipline and profession, is responsible for providing the needs of patients in clinical environments and all the community. Nowadays, in the era of technology and knowledge explosion, along with an increase in chronic diseases and societies’ need for receiving professional services all around the world, especially in developing countries, health systems would encounter various challenges in the near future. One of them would be the outbreak of noncommunicable diseases, especially cancer.[1]
The World Health Organization has predicted that >15 million people would develop cancer by 2020 and about 10 million people would die because of cancer every year.[2] Cancer patients would experience many problems that, if not relieved, could lead to suffering, discomfort and emotional, social and spiritual consequences, and cause patients and their family disability. By providing comprehensive care, the quality of life in patients and their families could be improved and dignified, and comfortable death would be provided for the patient, and a support system would be provided for their family.[23]
Palliative care is a comprehensive care that could be applied at all the stages of the disease and patients could receive them along with receiving therapeutic measures such as chemotherapy, radiotherapy, and surgery. Palliative care is a holistic interprofessional care approach. In holistic approaches, all the dimensions of care would be considered as an integrated whole to reduce and relieve patients’ pain and suffering. Palliative care has a holistic approach toward all the dimensions of humans’ existence and also families and could be provided with different methods in different settings such as a house, hospitals, palliative care special centers, and other care centers by members of health team.[245]
Studies have shown that patients and their families have received poor services which are indicated by untreated symptoms and unmet personal, mental and social needs, also increased burden of care on caregivers and decreased satisfaction of patients and their families. The National Consensus Project for Quality Palliative Care has demonstrated that one of the main principles of palliative care is the presence of trained and licensed staff in the field of palliative care.[6] Considering the holistic nature of nursing and paying attention to all the aspects of human life, the role of palliative care nurse in evaluating all the aspects of personal needs and designing, conducting, and evaluating interventions are of great importance. Therefore, nurses should have sufficient and appropriate knowledge about educating and applying nonmedicinal therapies like palliative care so that they could provide clinical interventions and educate patients and their families about them.[57]
Since in Isfahan nurses’ participation in treatment programs and palliative care is insufficient and health system needs trained nurses for providing palliative care, therefore, it is necessary to execute and develop new nursing educational courses so that nurses, by gaining necessary and appropriate knowledge, attitude, and skills, would be able to provide comprehensive and standard care for patients in need of palliative care and their families. Therefore, this study was conducted to empower nurses in providing palliative care to cancer patients and their families.
Considering the fact that, in Iran, sufficient measures have not been conducted for empowering nurses in providing palliative care, and on the other hand, the number of cancer patients who would require palliative cares is increasing, designing, and executing educational courses for the empowerment of nurses is necessary, so that nurses, by gaining sufficient knowledge, attitude, and skills would be able to provide comprehensive care for the patients who need palliative cares and their families. This study was conducted to empower nurses for providing palliative cares to cancer patients and their families.
MATERIALS AND METHODS
In this study, for empowering nurses in providing palliative care for cancer patients, a community-based action research was conducted at selected hospitals of Isfahan which provide services for cancer patients during 2015. Action research is a form of social research which would be conducted by the participation of a professional action research is a form of social research which would be conducted by the participation of a professional research team and members of an organization or community, to improve and enhance their condition.[8] This study had 33 participants including twenty nurses, three head nurses, one nursing services manager, four oncologists, and five nursing lecturers as researcher team. Based on the stages of action research, this study was conducted through five stages.
First stage (determining the gaps and the need for a plan)
At this stage, three hospitals and private health center were selected for providing health-care services to cancer patients. Since nurses working at these centers had no previous training about palliative care, therefore, research that could empower these nurses was an educational necessity in these centers. To get an agreement on the necessity of conducting a short-term palliative care nursing educational program first, the priorities of nurse's educational needs were determined. The research team conducted a number of group discussion sessions with the participants about the necessity of training palliative care nurses and their educational needs. At these sessions, caring for patients and their families who needed palliative care, sufficiency and efficiency of nurses’ professional duties, and the quality of provided care by nurses were discussed.
Second stage (planning)
For planning, eight 2-h sessions were held between the research team and the participants about the goals of the study; its method and the method of evaluation of results. Then, based on previous studies and literature review, the suggested content for this course was presented by the research team and was prioritized by a panel of experts including the research team and the physicians and nurses who provide services for cancer patients and their families based on decision matrix.
The main goal of the program was gaining knowledge and skills about the principles of holistic care for cancer patients by the nurses.
The educational content of nurses’ empowerment program included two sections: theory course (80 h for 8 weeks) and clinical course (50 h for 5 weeks).
Third stage (act)
At this stage, 24 nurses participated in 80 h of theory classes through 8 weeks. This course included sessions of basic courses, main courses, and specialized courses. Basic courses included nursing concept, nursing ethics, principles of educating patients, the principles of consultation and communication, and the importance of clinical research. Main courses included the concepts of caring for the caregiver, quality of life, chronic and incurable diseases, palliative care, resiliency, stability, spiritual care, and caring at home. Specialized courses included palliative care for pain management, managing physical symptoms, managing cognitive symptoms, and different stages of life. After theoretical course, participants were divided into three groups and participated in 50 h of clinical training at patients’ bedside which was aimed for being introduced to the principles of caring for cancer patients according to palliative care approach.
Fourth stage (reflection)
At all the stages, review meetings were held with participants to study implementation method, program and related issues, and problems of project implementation were discussed and necessary corrections were applied. Sessions were conducted based on participants’ needs and team's decision every 3 weeks.
Fifth stage (evaluation)
To evaluate the program qualitative approach was used. Data were gathered through semi-structured individual and group interviews. About 15 individual interviews with an average time of 35 min and 2 group interviews with an average time of 60 min were conducted.
In individual interviews, interview's guide included a number of open questions about the effect of this program on their performance and to express their perceptions and experiences of the program in detail.
All of the raised discussions at individual and group interviews were recorded on tape. Data were analyzed using content analysis. Through this method, coding and categorization were directly and deductively extracted from raw data.[9] Performed stages included 1-writing down the interviews, finding a general sense about the data, and extracting semantic units, 2-summarizing and categorizing semantic units into compressed semantic units (coding), 3-summarizing and categorizing similar primary codes based on their relations into subcategories, and 4-organizing subcategories by comparing their similarities and differences and creating the main categories.[10] In this study, ethical considerations including explaining the goals of the study and the methods of data gathering for participants and attracting their cooperation, taking informed consent form and considering essential points like the goals of the study, the benefits of participation, answering the questions, the right to refuse the continuation of the study, and ensuring for keeping their data safe and confidential were all regarded.
RESULTS
The aim of this study was empowering nurses in providing palliative care for cancer patients, which was manifested in participants’ expressions in the evaluation stage of the study. Participants’ experiences about this study contained three main categories of "professional development of nursing in palliative care," "obstacles for providing palliative care," and "solutions for improving the provision of palliative care" [Table 1].
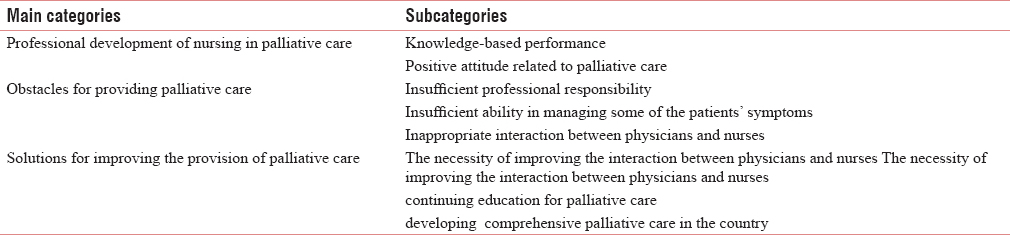
Professional development of nursing in palliative care
One of the main categories was "professional development of nursing in palliative care." This concept was created from two subcategories: Knowledge-based performance and positive change in attitude. Professional development in nursing would improve the quality of nursing cares. Participants expressed that taking part in empowerment program have improved their knowledge, attitude, and performance in the field of palliative care including management of physical symptoms and pain management. Furthermore, they have learned more knowledge about the role of nurses in palliative care team which resulted in improved interaction and provision of care for patients. Participants believed that empowered nurses in the field of palliative care could improve the quality of provided care for patients and consequently nursing profession would be improved.
In this regard, a nurse with 4 years of experience mentioned:
“I used to do a lot of things for my patients but I had no information about their scientific basis. Now, when I do something, I know about its process and mechanism…"
Another nurse with 2 years of experience expressed:
“I was not familiar with the method of pain management for these patients. I never thought that nonmedicinal methods could be so effective in pain management. But now I have a good feeling and feel more useful…"
One of the head nurses with 15 years of experience said:
“I had heard about spiritual care before, but I never believed it was possible because I had never done it. But now I believe that this aspect of care must be considered more…"
Obstacles for providing palliative care
This concept was created from three subcategories: Insufficient professional responsibility,
Insufficient ability in managing some of the patients’ symptoms, and Inappropriate interaction between physicians and nurses.
Empowerment of nurses is a challenging process toward improving nursing cares. One of the major challenges is the obstacles for providing palliative care which could be discussed in subcategories of insufficient professional responsibility and insufficient ability of nurses in managing some of the patients’ symptoms.
One of the nurses with 12 years of experience mentioned:
“Most of us, nurses, believe that we must work by the instructions but our job is more than that. Especially when caring for cancer patients. We might not pay enough attention to many of the necessary stuff. For example, the patients and their families might have questions and instead of answering, we just refer them to the physician and we probably think that it is not our job to answer their questions…"
Furthermore, another nurse with 3 years of experience said:
“When we just start working, we do not know many of the routines. Also nurses might face a case which is new to them. Sometimes, I really do not know how to control patients’ pain…"
Solutions for improving the course of palliative care
The category of solutions for improving the course of palliative care contained three subcategories: Improving the interaction between physicians and nurses, constant training of palliative care, the necessity of developing palliative care around the country.
One of the nurses with 5 years of experience in cancer wards mentioned:
“You know that in cancer patients different organs and systems are involved in the disease. One of the roles of us, nurses, is coordination. When we have a good relation with other team members, especially physicians, and they also have an appropriate relation with us, we have a constructive interaction and so we could expect to be successful in providing palliative care and solving patients’ problems…"
Another participant who was a head nurse with 20 years of experience said:
“We should not think that a short-term professional program has been conducted and that's all…This is good for the start but it is not the end of the road. For having successful palliative care, this type of programs must continue…"
One of the nurses with 14 years of experience expressed:
“Some of the participants in this program were really eager and some, who live in other cities, are still in touch with us, and we use their help for patients who live in other cities. This indicates that if we execute good programs we will get good results and we would be able to develop palliative care in other places too…"
DISCUSSION
As it could be concluded from participants’ statements, professional development is one of the consequences of empowerment. The American Nurses Association has defined professional development as the lifelong process of nurses’ active participation in learning that would help the constant improvement of competence and enhancement of professional performance.[11] For this matter, health team staff must improve their professional competence through empowerment[12] and by providing high quality and safe care.[13] Participants in the present study mentioned that professional development was the most important consequence of empowerment program because it made them have a more effective interaction and relation with patients and answer patients’ questions more accurately. Through appropriate interaction with patients, nurses could improve patients’ knowledge about their disease, its complications, its treatments, and their own care so that patients would become an active part in their own treatment.[14]
In this study, professional development, by providing science and knowledge about palliative care at different stages of life and management of physical and cognitive symptoms in patients and its appropriate execution, improved professional competency in participated nurses and the quality of care that was provided by them. In this regard, Glasson et al., through an action research, conducted a study to improve the quality of nursing cares for elderly patients with medical problems, which by participation of nurses, presented new design, execution and evaluation of nursing care models; based on their results, it was revealed that reinforcement and improvement of nurses’ abilities would improve the quality of care for patients, increase nurses’ satisfaction, and give nurses a sense of empowerment and authority.[15]
As the participants expressed, for developing and spreading palliative care, necessary actions and measures must be conducted. Providing palliative care is considered an interprofessional teamwork and achieving the objectives of care; there must be coordination and mutual respect between different professions, especially nurses and physicians. Meier et al. also in their study mentioned that participation and active interaction between the members of health team including physicians, nurses, social workers, spiritual advisers, and other members are the main necessities for providing palliative care.[6] Furthermore, Mardani Hamooli mentioned that the conflict between physician and nurse is one of the greatest obstacles to providing palliative care; therefore, improving the relations could help improving the provision of palliative care.[16] In a study by Brueckner et al., conflicts between physicians and nurses and lack of effective teamwork have been mentioned by the participants as the main problems; therefore, improving the relations and enhancing team works could be advancement in providing palliative care.[17] In the study of Mundy et al., in the UK, it was also revealed that palliative care processes required effective interprofessional relations and defined it as an important facilitator.[18]
Another recommended solution by the participants was holding continuous educational courses about palliative care. Participants stated that palliative care should not be summarized in taking part in one short-term professional course; this program was necessary for the beginning but is not sufficient. Hence, accurate planning is required for conducting constant educational courses about palliative care. In this regard, Wiener et al. mentioned a combination of educational interventions, experiential learning, creating learning opportunities, and constant training for improvement of palliative care as the improving factors for providing palliative care.[3] Developing educational palliative care program all around the country was another solution which was recommended by the participants. Meier et al. also in their study revealed that availability of palliative care at different locations across the country must be increased and for reaching this goal, they recommended to increase the number of expert teams on palliative care and making sure that the provided service by them has been necessary.[6]
As it could be realized from participants’ statements, nurses are facing some obstacles in providing palliative care; in a way that these obstacles could prevent them from the transition of their science and skills. Health-care centers should provide necessary conditions for professional improvement and gaining credibility and professional competence in the field of palliative care for health-care staff so that the health team would provide palliative care with more responsibility, knowledge, and confidence. Participants’ experiences showed that when patients had many questions, nurses did not feel it to be their duty to answer them, therefore, they usually refused to answer them. In this regard, Walshe et al., in a qualitative content analysis study in the UK for evaluating the judgment of health team (physicians and nurses) about palliative care resulted that in the participants’ point of view, judgments based on professional responsibility, respect, and mutual communication were effective factors on palliative care.[19] Nurses must have sufficient professional responsibility toward patients to be able to provide holistic care, which is associated with nursing. In this study, nurses’ insufficient ability in managing some of the patients’ symptoms prohibited them from providing appropriate care to these patients. In this regard, Jünger et al. also mentioned that nurse’ challenges in managing patients’ symptoms are one of the main obstacles to providing palliative care.[20] Furthermore, Meier et al. indicated that lack of related skills and expertise about palliative care among health team staff was one of the main obstacles to providing palliative care; in a way that, due to unavailability of expert physicians and nurses, providing palliative care had been limited.[6] Hence, considering the changing condition of cancer patients, it is possible that different symptoms would occur in the patients so that nurses, especially those with insufficient experience in the field of cancer, would face some problems in managing some of the symptoms.
CONCLUSION
With the development of interprofessional cooperation and the necessity of using this approach for providing holistic care, the ground has been set for providing palliative care as an undeniable necessity for the health team to manage cancer patients. Through accurate planning for creating the necessity infrastructures to train expert and skilled resources in the palliative care, we could be hopeful to provide appropriate care for cancer patients and their families. Putting palliative care courses in the curriculum of nursing, medicine, and other health majors’ students, as much as needed, could be helpful in advancing the goals of palliative care. Therefore, health-care providers and managers of health centers must provide the necessary time and finance for this purpose and pursue empowerment programs for professional health-care teams to improve and enhance the quality of palliative care services for needful patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the Nursing and Midwifery Care Research Center of Isfahan University of Medical Sciences and also all the participants, which the results of this study are the outcome of their sincere cooperation. We also would like to appreciate the managers of Seyyed-Al-Shohada educational hospital and Ala charity center for their cooperation.
REFERENCES
- Oncology Nursing Advisor Comprehensive Guide to Clinical Practice. Vol 456. Philadelphia: Mosby Elsevier; 2009.
- What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J. 2010;16:423-35.
- [Google Scholar]
- Threading the cloak: Palliative care education for care providers of adolescents and young adults with cancer. Clin Oncol Adolesc Young Adults. 2015;5:1-8.
- [Google Scholar]
- Hospital-Based Palliative Medicine: A Practical, Evidence-Based Approach. London: Willey Blackwell; 2015.
- [Google Scholar]
- Palliative Caring for Suffering Patients. London: Jones & Bartlett Learning; 2012.
- Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Q. 2011;89:343-80.
- [Google Scholar]
- The nursing metaparadigm concept of human being in islamic thought. Nurs Inq. 2014;21:121-9.
- [Google Scholar]
- Action Research in Healthcare. London: Willey Blackwell; 2011.
- Nurse-led action research project for expanding nurses’ role in patient education in Iran: Process, structure, and outcomes. Iran J Nurs Midwifery Res. 2015;20:387-97.
- [Google Scholar]
- Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-88.
- [Google Scholar]
- Clinical nurses’ perception of continuing professional education as a tool for quality service delivery in public hospitals Calabar, cross river state, Nigeria. Nurse Educ Pract. 2013;13:328-34.
- [Google Scholar]
- Action research for closing theory practice gap by nurse-researchers. Q J Nurs Midwifery. 2011;12:68-80.
- [Google Scholar]
- Strategies for continuing professional development among younger, middle-aged, and older nurses: A biographical approach. Int J Nurs Stud. 2015;52:939-50.
- [Google Scholar]
- Barriers and facilitators of patient's education: Nurses’ perspectives. Iran J Med Educ. 2012;11:620-34.
- [Google Scholar]
- Evaluation of a model of nursing care for older patients using participatory action research in an acute medical ward. J Clin Nurs. 2006;15:588-98.
- [Google Scholar]
- Interpretation of palliative care concept, its barriers and facilitators using meta-synthesis. Mod Care Sci Q Birjand Nurs Midwifery Fac. 2015;11:316-29.
- [Google Scholar]
- Palliative care for older people - exploring the views of doctors and nurses from different fields in Germany. BMC Palliat Care. 2009;8:7.
- [Google Scholar]
- Facilitating good process in primary palliative care: Does the gold standards framework enable quality performance? Fam Pract. 2007;24:486-94.
- [Google Scholar]
- Judgements about fellow professionals and the management of patients receiving palliative care in primary care: A qualitative study. Br J Gen Pract. 2008;58:264-72.
- [Google Scholar]
- Barriers and needs in paediatric palliative home care in Germany: A qualitative interview study with professional experts. BMC Palliat Care. 2010;9:10.
- [Google Scholar]






