Translate this page into:
Ultrasound-Guided Real-Time Pterygopalatine Block for Analgesia in an Oral Cancer Patient
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Oral cancers are one of the most common cancers in India. These patients have pain during the course of the disease. Various drugs including opioid and nonsteroidal anti-inflammatory drug have been used to manage pain. However, these are associated with side effects such as constipation and vomiting. An early interventional block may decrease the requirement for analgesics and improve the overall quality of life. We describe a case of oral carcinoma successfully managed with ultrasound-guided pterygopalatine block.
Keywords
Oral cancer
pain management
pterygopalatine block
ultrasound
INTRODUCTION
Oral cancer is one of the most common cancers in India occurring in four out of every ten cancer case.[1] Head and neck cancers have the highest prevalence of pain surpassing other malignancies.[2] It may be due to tumor invasion leading to inflammation and neuropathy. Inadequate pain relief may affect the functional capability, nutritional intake, and sleep pattern of the patients and increases the caregiver burden. Hence, optimal pain management is essential to improve the quality of life, nutrition, mobility, and the physical rehabilitation of patients. Opioids play a significant role in cancer pain management, although they are not free from adverse effects, especially nausea, vomiting, constipation, and reduced compliance due to frequent dosing. An early use of interventional nerve block may help to decrease the requirement of opioids and the associated side effects. Moreover, early intervention is also preferred as it may not be technically feasible at a later stage due to tumor invasion or fibrosis following radiotherapy. Trigeminal nerve block via pterygopalatine approach can be performed for orofacial pain involving the area distribution of this nerve. Use of ultrasound (US) for peripheral nerve blocks provides a greater accuracy, increases safety, allows real-time visualization of structures, and increases the success rate of the block.[3] We are describing pterygopalantine trigeminal nerve block in a case of carcinoma (CA) of the right gingivobuccal sulcus (GBS) for pain management for the first time.
CASE REPORT
A 50-year-old male patient, a case of CA GBS awaiting surgery, presented with the chief complaint of pain (numeric rating scale [NRS] 8/10) on the right side of the face. The pain extended from below the eyes up to the upper part of the neck, was throbbing in nature, and increased with jaw movements. His pain was not relieved with tablet tramadol 100 mg tid, tablet ibuprofen 400 mg tablet, paracetamol 500 mg tid, and tablet gabapentin 100 mg once at night. He also had nausea and occasional vomiting.
Computerized tomography scan was suggestive of soft-tissue thickening in right buccal mucosa and base of the second and third molar with focal destruction of the cortex.
A written informed consent was obtained and the US-guided trigeminal nerve block via pterygopalatine fossa for adequate pain management was planned.
The patient was placed in the left lateral decubitus position, and electrocardiogram, pulse oximeter, and noninvasive blood pressure cuff were attached. A 20G intravenous line was secured, and fentanyl 1 mcg/kg was given. Under all aseptic precautions, the linear transducer probe was placed longitudinally on the lateral side of the face below the zygomatic bone, above the mandibular notch, and in front of mandibular condyle with a cephalad angulation. The maxilla, lateral pterygoid plate, and lateral pterygoid muscle were identified. The surrounding vasculature including maxillary artery was visualized in pterygopalatine fossa and confirmed using color Doppler. An insulated needle was advanced parallel to the transducer probe (in-plane technique) visualizing the entire trajectory of the needle [Figure 1]. Bupivacaine 0.25% with triamcinolone 40 mg was deposited deep to the lateral pterygoid muscle and anterior to the lateral pterygoid plate after negative aspiration. The good local anesthetic spread was visualized. The NRS was 3/10 after 30 min of procedure. No complications, for example, paresthesia, were reported during follow-up in the outpatient department after 2 weeks.
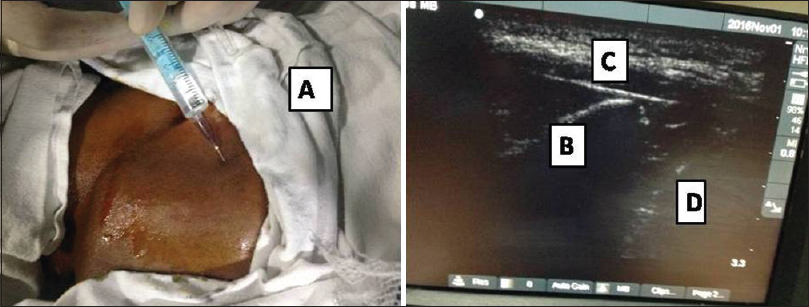
- (A) Patient positioned for the block and local anesthetic being infiltrated in skin and subcutaneous tissue; Needle (B) seen in situ lying between the lateral pterygoid plate (C) and the maxilla (D)
DISCUSSION
Oral cancers have the highest prevalence of pain among all cancers and are localized due to dense trigeminal nerve innervations of the oral cavity. The pain in oral cancer patients is multifactorial and may be caused by release of chemical mediatorsthat sensitize the nociceptors in cancer microenvironment, dense trigeminal innervation, and continuous functionaluse with mechanical stimulation of oral structures duringspeech, mastication, and swallowing.[4] It can also occur following chemotherapy and radiotherapy. Pain may lead to speech impairment and also difficulty in eating, drinking, swallowing, and maintaining interpersonal relations. Untreated pain may also lead to anxiety and depression and have a negative impact on the quality of life. Hence, optimal pain management is essential.
Cancer pain is managed according to the WHO pain ladder which includes nonsteroidal anti-inflammatory drug, opioids, adjuvants, and interventional modality.[5] Opioids being the mainstay of cancer pain treatment are not without adverse effects. This includes nausea, vomiting, constipation, sedation, respiratory depression, pruritus, and poor compliance due to frequent dosing which limits its use.
Early use of interventional modality like nerve block helps to overcome the adverse effects of opioids by reducing the requirement of these drugs. Furthermore, radiotherapy to the head and neck area and tumor progression may cause fibrosis and distort the airway anatomy. Hence, the intervention for nerve block may be difficult at a later stage, and an early intervention is warranted.[6]
Trigeminal nerve block using local anesthetics and steroids can be performed for the relief of cancer pain in the area of distribution of these nerves. Trigeminal nerve can be blocked by different approaches like classic approach via foramen ovale or indirectly via pterygopalatine fossa. It can be performed using landmark technique or fluoroscopy or computerized tomography (CT). Depending on the site of pain, the block can be performed on the Gasserian ganglion or one of the major divisions or smaller branches. Pterygopalatine fossa contains the pterygopalatine ganglion and its branches, maxillary branch of the trigeminal nerve, and maxillary artery and communicates with superior orbital fissure, foramen rotendum, foramen ovale, and vidian canal.[7] It is a very compact space, and injection into this space directly places the injectate close to foramen rotendum. The block is performed under X-ray guidance in fluoroscopy suite or using CT guidance in the radiology department or by paresthesia technique for blocking the branches of trigeminal nerve. These techniques rely on identification of bony landmarks which may be difficult to interpret. Furthermore, there is radiation exposure as in CT or fluoroscopy. Use of US allows for real-time visualization of soft-tissue, bony, and vascular structures. Real-time visualization of vasculature minimizes the risk of inadvertent puncture and intravascular injection. It also helps in visualizing the needle trajectory and thus helps in fine adjustment of the needle tip and direct observation of the injectate, confirming the spread of injectate in the target area.
The US-guided trigeminal nerve block via pterygopalatine fossa was used in patients with refractory trigeminal neuralgia and atypical facial pain.[8910] It provided sustained effective pain relief and could be performed even in the outpatient department. The disadvantage is that it requires skill and expertise in using US and also the availability of US machine.
We used US-guided pterygopalatine block for effective pain relief in a case of oral cancer, which provided a good visualization of structures and good pain relief with no complications. Use of US for block placement is much useful in oral cancer patients as the presence of edema, fibrosis, and tumor invasion could distort the anatomy, making the block placement using landmark technique difficult. This is the first report of ultrasonography-guided trigeminal nerve block via pterygopalatine fossa being used in cancer pain management.
Hence, US-guided pterygopalatine block could be an alternative approach for blocking trigeminal nerve branches in cancer pain management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Oral cancer in India continues in epidemic proportions: Evidence base and policy initiatives. Int Dent J. 2013;63:12-25.
- [Google Scholar]
- Ultrasound guidance for deep peripheral nerve blocks: A brief review. Anesthesiol Res Pract. 2011;2011:262070.
- [Google Scholar]
- Biologic mechanisms of oral cancer pain and implications for clinical therapy. J Dent Res. 2012;91:447-53.
- [Google Scholar]
- The WHO analgesic ladder for cancer pain control, twenty years of use. How much pain relief does one get from using it? Support Care Cancer. 2006;14:1086-93.
- [Google Scholar]
- Long-term changes induced by high-dose irradiation of the head and neck region: Imaging findings. Radiographics. 1997;17:5-26.
- [Google Scholar]
- The pterygopalatine fossa: Imaging anatomy, communications, and pathology revisited. Insights Imaging. 2016;7:589-99.
- [Google Scholar]
- Ultrasound-guided trigeminal nerve block via the pterygopalatine fossa: An effective treatment for trigeminal neuralgia and atypical facial pain. Pain Physician. 2013;16:E537-45.
- [Google Scholar]
- Ultrasound guided trigeminal nerve block: A new technique via pterygopalatine fossa. Neurol Asia. 2015;20:101-2.
- [Google Scholar]
- Ultrasound-guided pulsed radiofrequency application via the pterygopalatine fossa: A Practical approach to treat refractory trigeminal neuralgia. Pain Physician. 2015;18:E411-5.
- [Google Scholar]






