Translate this page into:
Complementary Therapies for Symptom Management in Cancer Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cancer patients are often poly-symptomatic which distressingly affects their quality of lives (QOLs). Alhough, conventional management provides adequate symptom control, yet is coupled with some limitations. Complementary therapies (CTs) have shown beneficial effects in cancer patients for symptomatic relief. The aim of this article is to provide evidence-based review of commonly used CTs for symptom management in cancer care. Hypnosis has promising evidence to be used for managing symptoms such as pain, chemotherapy-induced nausea/vomiting, distress, fatigue, and hot flashes. Guided imagery increases comfort and can be used as a psycho-supportive therapy. Meditation substantially improves psychological function, mental health, and QOL. Cognitive behavioral therapies effectively reduce pain, distress, fatigue, anxiety, and depression; and improve subjective sleep outcomes along with mood and QOL. Yoga has short term beneficial effects for anxiety, depression, fatigue, perceived stress, QOL, and well-being. T'ai Chi and qigong are beneficial adjunctive therapies for supportive cancer care, but their role in reducing cancer pain is not well proven. Acupuncture is effective for reducing treatment related side-effects, pain and fatigue. Other therapies such as massage techniques, energy therapies, and spiritual interventions have also demonstrated positive role in managing cancer-related symptoms and improve overall well-being. However, the clinical effectiveness of these therapies for symptom management in cancer patients cannot be concluded due to poor strength of evidence. Nonetheless, these are relatively free from risks and hence can be given along with conventional treatments. Only by tailoring these therapies as per patient's beliefs and preferences, optimal patient-centered holistic care can be provided.
Keywords
Cancer
complementary therapies
mind-body therapies
pain
quality of life
INTRODUCTION
Survival rates of cancer patients are rapidly increasing over the last decade due to the advent of multi-modal anti-cancer treatments.[1] The newer treatments have shifted the disease paradigm from a serious fatal illness to a chronic illness.[2] During illness, survivors experience multitude of distressing symptoms such as pain, fatigue, anxiety, depression, insomnia, lymphedema, hot flashes, and nausea/vomiting.[3]
The conventional treatment for managing these symptoms is often unacceptable due to associated side-effects. With the increased longevity after cancer diagnosis, patients prefer to take treatments which improve their quality of lives (QOLs).[4] The use of complementary/alternative therapies to improve health and QOLs is increasing among both general population and cancer patients.[56] National Institute for Clinical Excellence describes complementary therapies (CTs) as those which are “used alongside orthodox treatments with the aim of providing psychological and emotional support through the relief of symptoms.”[7] For around two decades, CTs have been integrated with palliative care (PC) services as both intend for holistic patient care.[89] Nonetheless, these therapies are coupled with some anecdotal or hearsay misunderstandings and lack of scientific evidence. Thus, despite the fact that the patients show noteworthy interest in using these therapies, they may remain deprived of their benefits.[79] In this article, we aim to provide an evidence based review of commonly used CTs available for symptomatic relief in cancer patients.
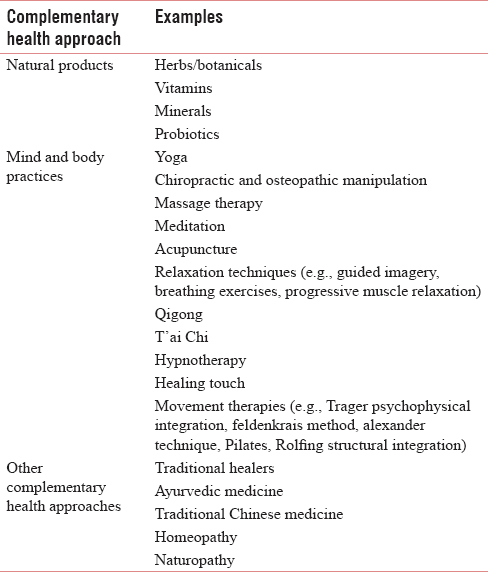
The National Institute of Health Center for Complementary and Alternative Medicine (NCCAM) classified CTs into five domains-Mind-Body Medicine, Natural Product Based Therapies, Manipulative and Body-Based Practices, Energy Medicine and Whole Medical Systems.[10] NCCAM, later renamed as National Center for Complementary and Integrative Health,[11] classified complementary health approaches into two subgroups-natural products, and mind and body practices. The approaches which could not fit into both of these were grouped as other complementary health approaches [Table 1].[12]
COMMON COMPLEMENTARY THERAPIES USED FOR CANCER-RELATED SYMPTOMS
Mind-body therapies
Mind-body therapies focus on the bodily interactions with the mind, brain and behavior in a way to augment mind's capacity to improve body's symptoms and functions.[1314] It includes both concentration based and movement based therapies. The former includes techniques such as hypnosis, guided imagery, and cognitive behavioral therapy (CBT), while the latter includes techniques such as yoga, qigong, and T'ai Chi.[15] These therapies are used for managing symptoms such as pain, fatigue, nausea, dyspnea, and sleep disturbances.[1416] These interventions are inexpensive, have negligible side-effects and can be taught to patients to practice independently. These enrich and refine the thought process, induce optimism for coping with symptoms, improve mood, reduce anxiety, and stress due to illness and increase relaxation.[17] Pain perception, thus, gets reduced due to the effect on psychological factors such as stress, anxiety, anger, depression, and fear.[18]
Biofeedback
It is a therapeutic tool by which an individual learns to control autonomic physiological activities to improve health. Validated instruments measure physiologic changes such as skin temperature, brain waves, pulse rate, heart function, breathing pattern, and muscle tension. Based on the activity measured, biofeedback is of five major types-thermal, electro-myographic, electro-dermal, respiration, and finger pulse. The audio/visual changes of physiological functions that result from altered behavior and thoughts are noted by the instruments and interpreted by trained therapists. The process is repeated as needed to achieve required control of symptoms.[19] It has been demonstrated that biofeedback is useful for improving QOL and reducing cancer-related pain.[20]
Hypnosis
It is a psychotherapeutic practice where a health-care hypnotist induces a highly relaxed mental state whereby patient's mind is receptive for therapeutic suggestions.[16] Distractions are prevented in this state of altered consciousness. This allows the patient to focus attention on a particular symptom, illness, or problem.[14] Components of hypnosis interventions are described in Figure 1.[21]

- Components of hypnosis interventions
Hypnosis had been introduced around 200 years ago[2021] and has been researched extensively for variety of health conditions such as skin disorders,[16] temporomandibular disorders,[22] fibromyalgia syndrome,[23] insomnia,[24] anxiety,[25] irritable bowel syndrome,[26] smoking cessation,[27] labor/childbirth,[28] reducing body weight,[29] hot flashes,[30] tinnitus,[31] asthma,[32] headaches/migraines,[33] pain,[34] hypertension[35] and cancer.[35]
Although hypnosis is not widely practised in clinical set-up, yet evidence suggests that nearly 90% of patients would prefer to use this technique for managing side-effects manifesting due to cancer treatment.[36] In 1996, National Institute of Health technology assessment panel declared strong evidence for using hypnotherapy to reduce cancer pain.[37] A plethora of evidence is available to demonstrate its efficacy in alleviating cancer pain in both adults and children.[38] A summary of systematic reviews (SRs)/meta-analysis for the use of hypnosis in oncology settings is described in Table 2. It is affirmed that hypnotherapy has sufficient evidence to be used for symptom control in cancer patients.[43]

Guided imagery
It is a psychotherapeutic technique in which an individual creates images to visualize the desired outcome. It is defined as “any of various techniques (as a series of verbal suggestions) used to guide another person or oneself in imagining sensations and especially in visualizing an image in mind to bring about a desired physical response (as a reduction in stress, anxiety, or pain).”[44] Generally, it begins with relaxation, releasing distractions from the mind and then visualizing images related to physical and mental healing. It can be performed individually or in group settings, can be self-conducted or performed under the observation of trained guide, can be practised alone or with music and other relaxation therapies.[45]
Interactive-guided imagery is an approach whereby patients are evoked by a practitioner to use their inner resources for creating images to heal their bodies.[46] During this process, one connects with the subliminal mind[45] and emotions felt during visualization modulate the neuro-active peptides secreted by the body in a similar fashion as it would to an actual event.[46] Factors affecting outcomes from this therapy are – imaging ability, outcome expectancy,[47] and time spent for practice.[45]
It has been extensively used to determine the effects on various physiological systems[46] and health conditions such as fibromyalgia, cardiac disorders, stroke rehabilitation, multiple sclerosis, interstitial cystitis, cancer, and pain.[4548] Studies have been conducted to demonstrate the role of imagery in managing cancer-related symptoms such as pain, QOL, nausea/vomiting, anxiety, fatigue, and stress.[17454749505152] However, SR by Roffe et al.,[53] portrayed that it increases comfort and can be used as a psycho-supportive therapy. Later, a review stated that in three out of five studies pain intensity and distress due to pain was reduced when guided imagery was given as an intervention in cancer patients.[54]
Progressive muscle relaxation
Introduced in the early 1900s by Jacobson, progressive muscle relaxation (PMR) is one of the techniques used to evoke “relaxation response” of the body. “Relaxation response” comprises of various physiological and psychological events resulting from an overall reduction in sympathetic nervous system activity. During PMR major muscles of the body are systematically tensed and relaxed, and attention is paid on the sensations felt during the process.[55] This technique has evolved to various modifications such as jaw relaxation, abdominal breathing, or focused breathing.[17]
PMR alone has shown beneficial results for chemotherapy-induced nausea/vomiting,[56] mental health, QOL,[57] pain, and fatigue.[1758] Similar results are observed when PMR is given along with guided imagery[5960] or biofeedback.[61] However, SR of seven studies by Jane et al.,[62] did not yield promising results for effects of PMR given along with guided imagery for alleviating pain in cancer patients.
Meditation/mindfulness-based stress reduction
Meditation is a mental exercise which increases the awareness of thoughts running in mind and empowers mind to focus on a single target for as long as desired. Its cultural roots are embedded in the traditional Eastern systems. Mindfulness-based stress reduction (MBSR) is a meditation technique usually explored in the oncology setting.[1620] It was initiated at the Stress Reduction Clinic at the University of Massachusetts Medical Center in 1979. It is based on the principle of “Present Moment Awareness” which allows one to pay attention on present moment only and be nonjudgmental to new situations arising in the next moment.[63]
A meta-analysis of 29 studies demonstrated moderate effect of MBSR in reducing anxiety, stress, distress, and depression; and in enhancing QOL of healthy individuals.[64] Another meta-analysis of studies from the diverse clinical population (i.e., anxiety, depression, pain, cancer, and cardiovascular disorders) depicted medium statistically significant effect of MBSR on both physical and mental health of the population studied.[65]
Previous literature in cancer population demonstrates that MBSR is associated with enriched QOL[66] and sleep quality[6768] reduced stress,[666768] fatigue,[67] sleep disturbances,[67] mood fluctuations,[6768] and caregiver stress.[69] A summary of studies based on mindfulness-based interventions in cancer patients is provided in Table 3. It can be implicated that MBSR can substantially improve psychological function, mental health and QOL in cancer patients.[727374]

Although effects of MBSR have been studied for alleviating chronic pain, yet its role on cancer-related pain is not widely researched.[14] Semi-structured interviews conducted by Kvillemo and Bränström[75] described less physical pain experienced by cancer patients receiving MBSR intervention. Body scan meditation of MBSR not only substantially reduced pain but also improved overall physical health in terminally ill cancer patients.[76] Supportive therapy based on mindfulness has recently been proposed to address sufferings of PC patients.[77]
Cognitive-behavioral therapy
Thought process of an individual has a direct and sequential effect on his/her feelings, emotions and behavior. CBT is based on the concept that to change patients' behavior, their emotions need to be changed.[78] A trained therapist assists the patients in identifying challenging thoughts and then altering them to control the response towards disease symptoms. This is done using counseling approach or programmed education.[17] It involves techniques such as autogenic training, biofeedback, hypnosis, imagery, meditation, problem-solving, and systematic desensitization.[79]
In 14 out of 21 studies reviewed, Kwekkeboom et al.,[17] demonstrated that CBT was effective in improving pain, fatigue, or sleep disturbances in cancer patients. Table 4 summarizes studies demonstrating the use of CBT in oncology settings. Considering the burden of the disease, special requirements in advanced cancer patients, and effectiveness of psychosocial interventions like CBT there is a need to individualize them for patients.[8586]

Music therapy
Music has been used extensively since ages for its healing and curative power towards disease or distress. The scientific basis of music therapy (MT) evolved after World War II. Since then, the meaning and scope of application of MT have undergone many developments. However, the emergence of MT as a discipline is relatively new.[87]
American MT Association defines MT as “the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved MT program.”[88] Patients are engaged by trained music therapist in activities like listening to music, singing, etc.[89] Music produces multi-dimensional effects on body functions. It stimulates autonomic nervous system and releases endorphin from the brain. It allows spiritual strengthening at a psychological level.[51] This allows expressing oneself, easing communication and increases relaxation.[89]
It is now being extensively practised in various fields of medicine and rehabilitation.[5187] Kamioka et al.,[90] depicted in their summary of SRs that MT has potential to improve the quality of sleep, symptoms of depression, and other bodily functions.
MT has gained popularity in PC setting as it provides patients' comfort, relaxation, reducing symptoms and allows them to face end-of-life with dignity.[91] It has been used during anti-cancer treatments, for symptomatic relief, improving QOL and providing spiritual healing.[92] MT coupled with guided imagery, shows beneficial effects on chemotherapy-induced nausea/vomiting.[51] Many SRs and meta-analysis have been performed which demonstrate the role of MT in improving cancer-related symptoms [Table 5].

Yoga
The origins of yoga can be traced to more than 4000 years ago in India. It is a Sanskrit based word (yuj) meaning to unite, join or bind. It promotes health by uniting mind and body. The key elements of yoga are pranayama (breathing exercises), asanas (postures), and dhyana (meditation).[98] It focuses on four main principles - (1) the human body is a holistic entity, (2) every individual is unique, (3) empowers self and (4) healing depends on individuals' state of mind.[99] Some of the styles of yoga are hatha yoga, tibetan yoga, restorative yoga, iyengar yoga, sudarshan kriya yogic breathing and vinyasa yog.[16]
It has been extensively used by both healthy and sick individuals to alleviate stress, improve flexibility, and enhance relaxation and muscular strength. Its benefits are evident at the cellular, physiological and psychological levels.[100] It reduces stress which is responsible for exacerbating tumor growth. It also improves overall well-being, QOL and promotes healing.[99]
The majority of the studies for the role of yoga in symptom management involves breast cancer patients. Evidence from ten SRs suggests that yoga has short term beneficial effects for anxiety, depression, fatigue, perceived stress, QOL and well-being. Mixed effects are demonstrated for distress and nonsignificant results for physical health and sleep problems.[101] Yoga has shown positive effect for reducing pain[5102103] and lymphedema,[104105] but the sustainability of these results after yoga based intervention needs more investigation.
T'ai Chi and Qigong
T'ai Chi chuan (abbreviated as T'ai Chi, also known as taiji) has originated from traditional Chinese martial arts.[106] This Chinese phrase symbolizes “supreme ultimate.” It embraces the concept of chi or qi and Yin–Yang forces.[107] Qigong (known as Qi Qong/Chi Kung) is an ancient Chinese practice similar to T'ai Chi. It means cultivating qi (energy) through gong (i. e., skills gained by practice). Medically, qigong is described as “coordination of gentle exercise and relaxation through meditation and breathing exercise based on the Chinese medicine theory of energy channels.”[108]
Both are designated as 'meditative movement' or mindful exercises, as the body movements are performed along with deep breathing and awareness.[107109] They are considered both as mind-body therapies and energy therapies (ET).[108] They encourage the flow of qi (life force or vital energy) by integrating mind, body and soul, and restore balance in them. When the energy flows freely, blockage/stagnation of energy in body's energy channels is cleared. Restoring the energy balance restores health and even prevents diseases.[107110] Though, both share the common principle of regulating the body, breath and mind,[109111] yet are dissimilar in the level of complexity and ease of learning. T'ai Chi is relatively lengthy and involves complex movements, but qigong is easy to learn, simpler and a repetitive process.[111]
Both have significant and consistent evidence for improving an array of health conditions like bone and brain health, cardiovascular health, cognitive functioning, diabetes and metabolic syndrome, functional balance, fatigue, immune function, musculoskeletal disorders, obesity, pulmonary conditions, psychological symptoms, QOL, self-efficacy, sleep disorders, pain and cancer.[106107108109] Table 6 summarizes studies employing T’ai Chi/qigong in oncology settings. Despite the limitations of the research evidence, it can be stated that T’ai Chi and qigong are beneficial adjunctive therapies for supportive cancer care.[116117] Further studies should be based on stringent research methodology, and their role for alleviating cancer pain should also be investigated.

Acupuncture
It originated from traditional Chinese medicine over 2000 years ago.[14118] It involves insertion of hair-thin needles deep into the skin by skilled practitioners at specific sites known as acupuncture points.[118119] After inserting the needles, the acupuncture points are stimulated through manual manipulation (acupressure), electrical pulses (electro-acupuncture), heat (moxibustion) or laser light (laser acupuncture).[14119]
It is based on the philosophy of balancing yin and yang energies[119120] which correspond to the theory of balancing sympathetic and parasympathetic activity.[120] The literature demonstrates its benefit in managing medical conditions such as rheumatoid arthritis, epilepsy, back pain, labor pain, drug addiction, headaches, and postoperative nausea/vomiting.[121] It has been intensely used in cancer patients for management of symptoms such as pain, fatigue, xerostomia, nausea/vomiting, hot flushes, insomnia, anxiety, depression, dyspnea, and leucopenia.[122]
A large number of studies have been performed to support the role of acupuncture in managing pain and other cancer-related symptoms [Figure 2]. Due to the heterogeneity of methodologies of studies, cancer populations and techniques used, Cochrane SR concluded that the evidence is insufficient to predict its effectiveness in reducing cancer pain.[123] Later, Hu et al.,[124] revealed that cancer pain is better alleviated when acupuncture is given along with pharmacotherapy rather than pharmacotherapy alone. Chiu et al.,[125] also demonstrated its effectiveness in relieving cancer pain related to the tumor itself or resulting from surgery. Results for relieving pain due to chemotherapy or radiotherapy or hormonal therapy were ineffective. Studies demonstrate positive effects of acupuncture for managing cancer-related fatigue as well. Various SRs[126127128] and meta-analysis[129] suggest possible benefits of acupuncture as CT, but the evidence is insufficient to draw a significant conclusion for relieving fatigue. Garcia et al.,[130] highlighted its role to control hot flashes in breast cancer patients, but the strength of the evidence was unconvincing. Similarly, it has shown favorable effects for managing hiccups[131] and preventing and/or treating xerostomia,[132] but the methodological quality of studies was low. Stimulation of point Pericardium 6 (P6) by acupressure or needle can reduce chemotherapy-induced nausea/vomiting. However, current evidence from literature provides mixed results.[133]

- Role of acupuncture in managing cancer-related symptoms
More recent SRs have depicted that acupuncture is effective in cancer patients for reducing side-effects due to chemotherapy or radiotherapy,[134] pain,[134135] and fatigue;[135] thereby improving QOL.[135] It is a safe therapy[133] with rare complications and has a promising potential as CT for symptom control. Methodologically, strong studies are indicated for future to provide concrete evidence.
Trans-cutaneous electrical nerve stimulation and scrambler therapy
Trans-cutaneous electrical nerve stimulation (TENS) is an electro-analgesic technique which reduces pain on the basis of pain gate mechanism. Electrical impulses stimulate A-beta nerve fibers which in-turn inhibits transmission via A-delta and C-fibers, thereby alleviating pain.[136] It has been used on a variety of painful conditions such as neurogenic, musculoskeletal, visceral, and cancer pain.[137] Although the Cochrane SR of three RCTs was inconclusive to depict the value of TENS in managing cancer-related pain,[138] yet its role as an adjunct for cancer pain management cannot be denied.[139] Giuseppe Marineo developed a similar approach known as Scrambler therapy, also known as MC5-A or Calmare Therapy.[140] Mixing or “scrambling” of painful and nonpainful information is the underlying mechanism for this therapy to alleviate pain. It comprises five sets of electrodes that are placed around the painful site on nonpainful dermatome. The therapy is given for ten consecutive days for 30–45 min/day.[136140] It has been used for a variety of malignant and nonmalignant painful conditions with substantial benefits. However, the outcomes are dependent on practitioners' skills; and multi-center, placebo-controlled, double-blinded studies are needed to strengthen its effectiveness.[140]
Massage techniques
Ancient scriptures from India, China and Japan, refer to the use of massage. It refers to pressure application by trained therapist to soft tissues of the body by pressing, rolling, kneading, rubbing or other movements.[141] Stimulation of pressure receptors increases vagal activity and reduces cortisol levels.[142] It is used for promoting circulation, reducing pain, eliminating waste products from the body, and relaxing muscles and nervous tissue.[14141143] A meta-analysis of 37 studies by Moyer et al.,[144] demonstrated that massage therapy significantly reduces anxiety and depression. Concurrently, a recent review demonstrated its favorable effects on various pain syndromes, autoimmune conditions, hypertension, prenatal and postnatal developmental conditions etc., as well.[142]
Commonly used therapeutic massage techniques in oncology are aromatherapy, acupressure, Swedish massage, and reflexology.[14] With debunking of myth of metastasis due to massage,[145] its use in oncology community for symptom management is increasing. It helps in alleviating both physical and psychological symptoms due to cancer and its treatment.[146] It is a skilled and systematic touch which needs to be delivered by trained hands in cancer patients as they are vulnerable for blood clot risk, easy bruising, osteoporosis, peripheral neuropathy or lymphedema.[145] Evidence from three SRs[147148149] is encouraging but inconclusive for role of massage in managing symptoms like pain, nausea, depression, anxiety, stress, anger, and fatigue in cancer patients.
Aromatherapy incorporates essential oils derived from plant sources having therapeutic benefits and is given through massage, inhalation or other means for both specific effects and overall well-being of an individual.[150] It has shown short-term benefits in improving anxiety and depression in cancer patients[150] but does not significantly reduce cancer pain.[150151] Reflexology has been used for alleviating pain, nausea, anxiety and depression in cancer patients.[152] The meta-analysis by Lee et al.,[153] specified that surgery-related pain is effectively reduced by massage, and foot reflexology is more effective than aroma or body massage. The clinical effectiveness of massage techniques for symptomatic cancer care cannot be concluded due to poor strength of evidence of studies performed.[154155]
Energy therapies and spiritual interventions
Healing can be induced by specific internal (intrapersonal) and external (interpersonal) techniques that assert to use subtle energy (known as prana, ch'i, qi or spirit) for curing self and another individual respectively.[156] Biofield or ETs unblock energy centers of the body and promote physical healing and mental, emotional and spiritual balance.[157] Moreover, these therapies cause direct effects by inducing relaxation response which blocks neuroendocrine stress response, thus enhancing immunity and other body functions[158] [Table 7].

Reviews demonstrate the potential of ET for cancer care, symptomatic relief and managing side-effects due to cancer treatment. The benefits observed from these therapies include reduction in pain scores, fatigue, anxiety and stress, and improvement in mood, overall wellbeing and QOL.[157159163164165] Pedro et al.,[166] concluded that there is some evidence to support the efficacy of ET for reducing pain and fatigue and promoting relaxation in cancer patients. Furthermore, a review of 30 studies by Henneghan and Schnyer[167] supported the use of ET for reducing pain and stress, and enhancing QOL in patients needing PC at end-of-life. Similar positive effect of therapeutic touch on symptom management in cancer patients has been reported by Tabatabaee et al.,[168] in their review of six studies. Similar to the CTs described earlier, the use of ETs is supported by limited evidence only and requires high quality systematic empirical research to be conducted.
Spiritual or existential concerns are inevitably associated with life-limiting disease like cancer. Spirituality helps patients in coping up with the emotional distress caused due to disease.[169170171] Better physical health is reported by cancer patients with greater spiritual well-being or religiosity.[172] CTs are often perceived to be a source of spiritual support[173] and are frequently used by those having more spiritual faith.[174] Patients' spiritual experiences are observed with healing due to ETs or other mindfulness-based CTs.[175176]
Oh and Kim[177] demonstrated in their meta-analysis of 15 studies that spiritual interventions have significant but moderate effect on spiritual well-being, meaning of life, anxiety and depression. Best et al.,[178] included six studies on spiritual interventions in their SR to treat holistic suffering in cancer patients. Though, results indicated positive effect for improving spiritual well-being but were inconsistent due to variability in population, modality and techniques used in the studies. Kruizinga et al.,[179] emphasized in their meta-analysis of 12 studies that spiritual interventions with narrative approach have moderate short term improvement in QOL immediately after the intervention. Sustainability of improved QOL after few months was not established. However, the evidence from all these studies was weak due to heterogeneity of studies involved.
CONCLUSION
The journey from diagnosis to treatment of cancer affects the patients' lives in a variety of ways. Debilitating symptoms arising both due to disease and its treatments consistently hamper their QOLs. CTs aim to provide holistic healing by addressing multivariate symptoms and hence have become popular in the oncology patient community. This extensive review of commonly used CTs is an attempt to provide evidence for suggesting and using them in oncology settings. It was identified that there is no clear-cut demarcation between some of the therapies. CBT includes techniques like hypnosis, imagery, meditation; which are considered as relaxation therapies as well; and have been considerably researched individually or in combination with other therapies. Similarly, spiritual healing is provided not only via spiritual interventions but also is experienced along with music interventions, yoga, meditation or energy healing. Therefore, the review performed for this article is based on the available literature which involves a variety of combination of CTs. All therapies described here have a potential for symptomatic care in cancer patients. However, recognition of effects of these therapies is barricaded by paucity of systematic high-quality research. Poor study designs with small sample size, varied cancer population, different outcome measures; statistically insignificant results and lack of unanimity on the mechanism of actions lead to limited scientific evidence. Despite the lack of strong evidence, the benefits pertained from CTs cannot be contravened. Acknowledging the need of patient-centered care and to address holistic suffering, the limitations of conventional treatments need to be accepted. It is suggested that high-quality research in this aspect is conducted to provide conclusive findings which will help in collective decision making by both patient and oncologist.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cancer survivorship: A positive side-effect of more successful cancer treatment. EJC Suppl. 2014;12:1-4.
- [Google Scholar]
- Anderson cancer center: Cancer as a chronic disease. Oncol Rep Physicians. 2008;53:1-5.
- [Google Scholar]
- Oxford Textbook of Palliative Medicine (5th ed). Oxford: Oxford University Press; 2015.
- Who accesses complementary therapies and why.: An evaluation of a cancer care service? Complement Ther Clin Pract. 2015;21:19-25.
- [Google Scholar]
- Breast cancer pain management - A review of current & novel therapies. Indian J Med Res. 2014;139:216-25.
- [Google Scholar]
- Working out of the 'tool box': An exploratory study with complementary therapists in acute cancer care. Complement Ther Clin Pract. 2014;20:207-12.
- [Google Scholar]
- National Institute for Clinical Excellence (NICE). Guidance on Cancer Services. Improving Supportive and Palliative Care for Adults with Cancer. 2004. The Manual. London: NICE; Available from: https://www.nice.org.uk/guidance/csg4/resources/improving-supportive-and-palliative-care-for-adults-with-cancer-773375005
- [Google Scholar]
- Complementary therapies: Making a difference in palliative care. Complement Ther Nurs Midwifery. 1998;4:77-81.
- [Google Scholar]
- Common misunderstandings about complementary therapies for patients with cancer. Complement Ther Nurs Midwifery. 1996;2:62-5.
- [Google Scholar]
- Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration. Altern Ther Health Med. 2011;17:50-9.
- [Google Scholar]
- National Center for Complementary and Integrative Health. NCCAM Has a New Name!. Available from: https://www.nccih.nih.gov/about/offices/od/nccam-new-name
- [Google Scholar]
- National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What's In a Name?. Available from: https://www.nccih.nih.gov/health/integrative-health
- [Google Scholar]
- Mind-body therapies – Use in chronic pain management. Aust Fam Physician. 2013;42:112-7.
- [Google Scholar]
- Complementary therapies in pain management. In: Cherny N, Fallon M, Kaasa S, Portenoy R, Currow DC, eds. Oxford Textbook of Palliative Medicine (5th ed). Oxford: Oxford University Press; 2015. p. :628-31.
- [Google Scholar]
- Mind body therapies in rehabilitation of patients with rheumatic diseases. Complement Ther Clin Pract. 2016;22:80-6.
- [Google Scholar]
- Mind-body therapies in integrative oncology. Curr Treat Options Oncol. 2010;11:128-40.
- [Google Scholar]
- Mind-body treatments for the pain-fatigue-sleep disturbance symptom cluster in persons with cancer. J Pain Symptom Manage. 2010;39:126-38.
- [Google Scholar]
- Management of total cancer pain: A case of young adult. Indian J Palliat Care. 2014;20:153-6.
- [Google Scholar]
- Biofeedback. In: Cassileth BR, ed. The Complete Guide to Complementary Therapies in Cancer Care: Essential Information for Patients, Survivors and Health Professionals. Singapore: World Scientific Publishing Co., Pte., Ltd.; 2011. p. :109-12.
- [Google Scholar]
- Mind-body therapies: Evidence and implications in advanced oncology practice. J Adv Pract Oncol. 2012;3:357-73.
- [Google Scholar]
- Hypnosis/Relaxation therapy for temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J Oral Facial Pain Headache. 2015;29:115-25.
- [Google Scholar]
- Efficacy of hypnosis/guided imagery in fibromyalgia syndrome – A systematic review and meta-analysis of controlled trials. BMC Musculoskelet Disord. 2011;12:133.
- [Google Scholar]
- Hypnotherapy for insomnia: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2015;23:719-32.
- [Google Scholar]
- The effectiveness of hypnosis for the treatment of anxiety: A systematic review. Prim Care Community Psychiatr. 2007;12:49-63.
- [Google Scholar]
- The efficacy of hypnotherapy in the treatment of irritable bowel syndrome: A systematic review and meta-analysis. J Neurogastroenterol Motil. 2014;20:152-62.
- [Google Scholar]
- A review of smartphone apps for smoking cessation available in portuguese. Cad Saude Publica. 2017;33:e00178215.
- [Google Scholar]
- Hypnosis for pain management during labour and childbirth. Cochrane Database Syst Rev. 2016;5:CD009356.
- [Google Scholar]
- Complementary therapies for reducing body weight: A systematic review. Int J Obes (Lond). 2005;29:1030-8.
- [Google Scholar]
- Can hypnosis reduce hot flashes in breast cancer survivors? A literature review. Am J Clin Hypn. 2004;47:29-42.
- [Google Scholar]
- Evidence-based hypnotherapy for asthma: A critical review. Int J Clin Exp Hypn. 2007;55:220-49.
- [Google Scholar]
- Hypnosis in the treatment of headache pain: A methodological review. Psychol Conscious (Washington DC). 2014;1:431-44.
- [Google Scholar]
- Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2014;5:CD003968.
- [Google Scholar]
- Hypnosis and music interventions (HMIs) inactivate HIF-1: A potential curative efficacy for cancers and hypertension. Med Hypotheses. 2015;85:551-7.
- [Google Scholar]
- Intentions to use hypnosis to control the side effects of cancer and its treatment. Am J Clin Hypn. 2010;53:93-100.
- [Google Scholar]
- Integration of Behavioral and Relaxation Approaches into the Treatment of Chronic Pain and Insomnia. NIH technology assessment panel on integration of behavioral and relaxation approaches into the treatment of chronic pain and Insomnia. JAMA. 1996;276:313-8.
- [Google Scholar]
- Hypnosis: Adjunct therapy for cancer pain management. J Adv Pract Oncol. 2013;4:83-8.
- [Google Scholar]
- Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol. 2012;30:539-47.
- [Google Scholar]
- Hypnosis for nausea and vomiting in cancer chemotherapy: A systematic review of the research evidence. Eur J Cancer Care (Engl). 2007;16:402-12.
- [Google Scholar]
- Systematic review of hypnotherapy for treating symptoms in terminally ill adult cancer patients. Palliat Med. 2005;19:418-26.
- [Google Scholar]
- Hypnosis in breast cancer care: A systematic review of randomized controlled trials. Integr Cancer Ther. 2015;14:5-15.
- [Google Scholar]
- Clinical hypnosis for the palliative care of cancer patients. Oncology (Williston Park). 2012;26:26-30.
- [Google Scholar]
- A pilot study to predict success with guided imagery for cancer pain. Pain Manag Nurs. 2003;4:112-23.
- [Google Scholar]
- A meta-analysis of the effect of guided imagery practice on outcomes. J Holist Nurs. 2004;22:164-79.
- [Google Scholar]
- Uses of guided imagery for pain control by african-american and white women with metastatic breast cancer. Integr Med. 2000;2:115-126.
- [Google Scholar]
- Imagery intervention for recovering breast cancer patients: Clinical trial of safety and efficacy. J Soc Integr Oncol. 2008;6:67-75.
- [Google Scholar]
- Effects of music therapy and guided visual imagery on chemotherapy-induced anxiety and nausea-vomiting. J Clin Nurs. 2013;22:39-50.
- [Google Scholar]
- The effect of guided imagery on stress and fatigue in patients with thyroid cancer undergoing radioactive iodine therapy. Evid Based Complement Alternat Med. 2013;2013:130324.
- [Google Scholar]
- A systematic review of guided imagery as an adjuvant cancer therapy. Psychooncology. 2005;14:607-17.
- [Google Scholar]
- A review of the effects of guided imagery on cancer patients with pain. J Evid Based Complement Alternat Med. 2010;15:98-107.
- [Google Scholar]
- Relaxation training as a technique for helping patients cope with the experience of cancer: A selective review of the literature. J Adv Nurs. 1987;12:583-91.
- [Google Scholar]
- A pilot study of a relaxation technique for management of nausea and vomiting in patients receiving cancer chemotherapy. Cancer Nurs. 2007;30:163-7.
- [Google Scholar]
- Impact of applied progressive deep muscle relaxation training on the health related quality of life among prostate cancer patients – A quasi experimental trial. Prev Med. 2013;57(Suppl):S37-40.
- [Google Scholar]
- Progressive muscle relaxation: An adjuvant therapy for reducing pain and fatigue among hospitalized cancer patients' receiving radiotherapy. Int J Adv Nurs Stud. 2013;2:58-65.
- [Google Scholar]
- Efficacy of progressive muscle relaxation training and guided imagery in reducing chemotherapy side effects in patients with breast cancer and in improving their quality of life. Support Care Cancer. 2005;13:826-33.
- [Google Scholar]
- Effect of relaxation with guided imagery on the physical and psychological symptoms of breast cancer patients undergoing chemotherapy. Iran Red Crescent Med J. 2015;17:e31277.
- [Google Scholar]
- Effects of electromyography biofeedback-assisted relaxation on pain in patients with advanced cancer in a palliative care unit. Cancer Nurs. 2007;30:347-53.
- [Google Scholar]
- The effects of progressive muscle relaxation and guided imagery in reducing cancer pain: A systematic review. Oncol Nurs Forum. 2005;32:189.
- [Google Scholar]
- Mindfulness-based stress reduction. In: Herbert JD, Forman EM, eds. Acceptance and Mindfulness in Cognitive Behavior Therapy: Understanding and Applying the New Therapies. New Jersey: John Wiley & Sons, Inc.; 2011. p. :132-63.
- [Google Scholar]
- Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res. 2015;78:519-28.
- [Google Scholar]
- Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57:35-43.
- [Google Scholar]
- Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571-81.
- [Google Scholar]
- Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278-85.
- [Google Scholar]
- Mindfulness-based stress reduction as supportive therapy in cancer care: Systematic review. J Adv Nurs. 2005;52:315-27.
- [Google Scholar]
- The effects of mindfulness-based stress reduction for family caregivers: Systematic review. Arch Psychiatr Nurs. 2016;30:292-9.
- [Google Scholar]
- Mindfulness-based stress reduction and cancer: A meta-analysis. Psychooncology. 2009;18:571-9.
- [Google Scholar]
- Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Curr Oncol. 2012;19:e343-52.
- [Google Scholar]
- The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psychooncology. 2013;22:1457-65.
- [Google Scholar]
- Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: A meta-analysis. Medicine (Baltimore). 2015;94:e0897-0.
- [Google Scholar]
- A meta-analysis of the benefits of mindfulness-based stress reduction (MBSR) on psychological function among breast cancer (BC) survivors. Breast Cancer. 2016;23:568-76.
- [Google Scholar]
- Experiences of a mindfulness-based stress-reduction intervention among patients with cancer. Cancer Nurs. 2011;34:24-31.
- [Google Scholar]
- The benefit of mindfulness-based stress reduction to patients with terminal cancer. J Clin Nurs. 2012;21:2690-6.
- [Google Scholar]
- Mindfulness-based supportive therapy (MBST): Proposing a palliative psychotherapy from a conceptual perspective to address suffering in palliative care. Am J Hosp Palliat Care. 2015;32:144-60.
- [Google Scholar]
- Cognitive behavior therapy for patients with cancer. J Adv Pract Oncol. 2015;6:54-6.
- [Google Scholar]
- Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: A meta-analysis. J Behav Med. 2006;29:17-27.
- [Google Scholar]
- Cancer-related fatigue: A systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol Bull. 2008;134:700-41.
- [Google Scholar]
- Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev. 2013;6:CD004253.
- [Google Scholar]
- Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst Rev. 2015;5:CD008729.
- [Google Scholar]
- Sleeping well with cancer: A systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat. 2014;10:1113-24.
- [Google Scholar]
- A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med Rev. 2016;27:20-8.
- [Google Scholar]
- Tailoring cognitive-behavioral therapy to treat anxiety comorbid with advanced cancer. J Cogn Psychother. 2010;24:294-313.
- [Google Scholar]
- A pilot randomized controlled trial of brief cognitive-behavioral therapy for anxiety in patients with terminal cancer. Oncologist. 2012;17:1337-45.
- [Google Scholar]
- Music therapy – History, definitions and application. Arch Psychiatr Psychother. 2006;8:47-52.
- [Google Scholar]
- American Music Therapy Association. What is Music Therapy. Available from: http://www.musictherapy.org/about/musictherapy/
- [Google Scholar]
- Music therapy reduces pain in palliative care patients: A randomized controlled trial. J Pain Symptom Manage. 2013;45:822-31.
- [Google Scholar]
- Effectiveness of music therapy: A summary of systematic reviews based on randomized controlled trials of music interventions. Patient Prefer Adherence. 2014;8:727-54.
- [Google Scholar]
- Development and efficacy of music therapy techniques within palliative care. Complement Ther Clin Pract. 2016;23:125-9.
- [Google Scholar]
- The clinical effects of music therapy in palliative medicine. Support Care Cancer. 2006;14:859-66.
- [Google Scholar]
- Music interventions for psychological and physical outcomes in cancer: A systematic review and meta-analysis. Support Care Cancer. 2012;20:3043-53.
- [Google Scholar]
- The impact of music interventions on anxiety for adult cancer patients: A meta-analysis and systematic review. Integr Cancer Ther. 2013;12:393-403.
- [Google Scholar]
- Arts therapies for anxiety, depression, and quality of life in breast cancer patients: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2014;2014:103297.
- [Google Scholar]
- Effectiveness of music intervention in ameliorating cancer patients' anxiety, depression, pain, and fatigue: A meta-analysis. Cancer Nurs. 2014;37:E35-50.
- [Google Scholar]
- Music therapy for end-of-life care: An updated systematic review. Palliat Med. 2016;30:877-83.
- [Google Scholar]
- Yoga for persistent pain: New findings and directions for an ancient practice. Pain. 2011;152:477-80.
- [Google Scholar]
- Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49-54.
- [Google Scholar]
- CAM-Cancer Consortium. Yoga. Available from: http://www.cam-cancer.org/The-Summaries/Mind-body-interventions/Yoga
- [Google Scholar]
- Randomized controlled trial in advance stage breast cancer patients for the effectiveness on stress marker and pain through Sudarshan Kriya and Pranayam. Indian J Palliat Care. 2013;19:180-5.
- [Google Scholar]
- Yoga of awareness program for menopausal symptoms in breast cancer survivors: Results from a randomized trial. Support Care Cancer. 2009;17:1301-9.
- [Google Scholar]
- Yoga for women with breast cancer-related lymphoedema: A preliminary 6-month study. J Lymphoedema. 2012;7:30-8.
- [Google Scholar]
- Yoga management of breast cancer-related lymphoedema: A randomised controlled pilot-trial. BMC Complement Altern Med. 2014;14:214.
- [Google Scholar]
- Tai Ji Quan: An overview of its history, health benefits, and cultural value. J Sport Health Sci. 2014;3:3-8.
- [Google Scholar]
- Tai chi and qigong validated health benefits. Altern Complement Ther. 2014;20:263-9.
- [Google Scholar]
- A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010;24:e1-e25.
- [Google Scholar]
- Medical qigong for cancer patients: Pilot study of impact on quality of life, side effects of treatment and inflammation. Am J Chin Med. 2008;36:459-72.
- [Google Scholar]
- Health benefits of qigong or tai chi for cancer patients: A systematic review and meta-analyses. Complement Ther Med. 2014;22:173-86.
- [Google Scholar]
- Tai chi for breast cancer patients: A systematic review. Breast Cancer Res Treat. 2010;120:309-16.
- [Google Scholar]
- Effects of qigong exercise on upper limb lymphedema and blood flow in survivors of breast cancer: A pilot study. Integr Cancer Ther. 2014;13:54-61.
- [Google Scholar]
- Randomized controlled trial of qigong/Tai chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med. 2015;49:165-76.
- [Google Scholar]
- Tai chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: A randomized controlled trial. J Pain Symptom Manage. 2016;51:504-11.
- [Google Scholar]
- Qigong in cancer care: A systematic review and construct analysis of effective qigong therapy. Support Care Cancer. 2016;24:3209-22.
- [Google Scholar]
- Effects of acupuncture, tuina, tai chi, qigong, and traditional Chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: A meta-analysis. J Pain Symptom Manage. 2016;51:728-47.
- [Google Scholar]
- Acupuncture. In: Cassileth BR, ed. The Complete Guide to Complementary Therapies in Cancer Care: Essential Information for Patients, Survivors and Health Professionals. Singapore: World Scientific Publishing Co., Ptv., Ltd.; 2011. p. :5-12.
- [Google Scholar]
- Acupuncture: What does the most reliable evidence tell us? J Pain Symptom Manage. 2009;37:709-14.
- [Google Scholar]
- Acupuncture for cancer pain in adults. Cochrane Database Syst Rev. 2015;10:CD007753.
- [Google Scholar]
- Acupuncture for pain management in cancer: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2016;2016:1720239.
- [Google Scholar]
- Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care (Engl). 2017;26:e12457.
- [Google Scholar]
- Acupuncture for cancer-related fatigue: A systematic review of randomized clinical trials. Support Care Cancer. 2013;21:2067-73.
- [Google Scholar]
- Acupuncture and moxibustion for cancer-related fatigue: A systematic review and meta-analysis. Asian Pac J Cancer Prev. 2013;14:3067-74.
- [Google Scholar]
- Effects of acupuncture and acupressure on cancer-related fatigue: A systematic review. Oncol Nurs Forum. 2014;41:581-92.
- [Google Scholar]
- Meta-analysis of randomized controlled trials of acupuncture for cancer-related fatigue. Integr Cancer Ther. 2014;13:193-200.
- [Google Scholar]
- Systematic review of acupuncture to control hot flashes in cancer patients. Cancer. 2015;121:3948-58.
- [Google Scholar]
- Acupuncture for cancer patients suffering from hiccups: A systematic review and meta-analysis. Complement Ther Med. 2012;20:447-55.
- [Google Scholar]
- Acupuncture for xerostomia in patients with cancer: An update. Med Acupunct. 2015;27:158-67.
- [Google Scholar]
- CAM-Cancer Consortium. Acupuncture for Chemotherapy-Associated Nausea and Vomiting. Available from: http://www.cam-cancer.org/The-Summaries/Mind-body-interventions/Acupuncture-for-chemotherapy-associated-nausea-and-vomiting
- [Google Scholar]
- Effectiveness of acupuncture for palliative care in cancer patients: A systematic review. Chin J Integr Med. 2014;20:136-47.
- [Google Scholar]
- Acupuncture and related therapies for symptom management in palliative cancer care: Systematic review and meta-analysis. Medicine (Baltimore). 2016;95:e2901.
- [Google Scholar]
- Yoga and physical therapy: Integrating as a way of life in cancer patients. J Yoga Phys Ther. 2016;6:247.
- [Google Scholar]
- Transcutaneous electrical nerve stimulation. Contin Educ Anaesth Crit Care Pain. 2009;9:130-5.
- [Google Scholar]
- Transcutaneous electric nerve stimulation (TENS) for cancer pain in adults. Cochrane Database Syst Rev. 2012;3:CD006276.
- [Google Scholar]
- The use of transcutaneous electrical nerve stimulation (TENS) in a major cancer center for the treatment of severe cancer-related pain and associated disability. Pain Med. 2015;16:1204-10.
- [Google Scholar]
- Scrambler therapy for the management of chronic pain. Support Care Cancer. 2016;24:2807-14.
- [Google Scholar]
- Managing cancer pain with nonpharmacologic and complementary therapies. J Am Osteopath Assoc. 2007;107:ES15-21.
- [Google Scholar]
- The use of massage therapy in palliative care. Complement Ther Nurs Midwifery. 2000;6:77-82.
- [Google Scholar]
- Massage therapy in cancer care: An overview of the past, present, and future. Altern Ther Health Med. 2014;20(Suppl 2):12-5.
- [Google Scholar]
- Therapeutic massage for management of cancer related symptoms: The role of oncology nurses. J Yoga Phys Ther. 2014;4:166.
- [Google Scholar]
- Massage for symptom relief in patients with cancer: Systematic review. J Adv Nurs. 2008;63:430-9.
- [Google Scholar]
- Massage therapy for cancer palliation and supportive care: A systematic review of randomised clinical trials. Support Care Cancer. 2009;17:333-7.
- [Google Scholar]
- Massage therapy for breast cancer patients: A systematic review. Ann Oncol. 2011;22:1459-61.
- [Google Scholar]
- Aromatherapy as an adjuvant treatment in cancer care – A descriptive systematic review. Afr J Tradit Complement Altern Med. 2012;9:503-18.
- [Google Scholar]
- The clinical effects of aromatherapy massage on reducing pain for the cancer patients: Meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2016;2016:9147974.
- [Google Scholar]
- Reflexology for the symptomatic treatment of breast cancer: A systematic review. Integr Cancer Ther. 2010;9:326-30.
- [Google Scholar]
- Meta-analysis of massage therapy on cancer pain. Integr Cancer Ther. 2015;14:297-304.
- [Google Scholar]
- CAM-Cancer Consortium. Reflexology. Available from: http://www.cam-cancer.org/layout/set/print/The-Summaries/Manipulative-body-based/Reflexology
- [Google Scholar]
- Massage with or without aromatherapy for symptom relief in people with cancer. Cochrane Database Syst Rev. 2016;6:CD009873.
- [Google Scholar]
- Biofield therapies: Helpful or full of hype? A best evidence synthesis. Int J Behav Med. 2010;17:1-16.
- [Google Scholar]
- Biofield therapies and cancer-related symptoms: A review. Clin J Oncol Nurs. 2014;18:568-76.
- [Google Scholar]
- The use of healing touch in integrative oncology. Clin J Oncol Nurs. 2011;15:519-25.
- [Google Scholar]
- Reiki – Review of a biofield therapy history, theory, practice, and research. Altern Ther Health Med. 2003;9:62-72.
- [Google Scholar]
- Couple therapy and reiki: A holistic therapeutic integration. Fam J Alex Va. 2012;20:292-8.
- [Google Scholar]
- Energy therapies in advanced practice oncology: An evidence-informed practice approach. J Adv Pract Oncol. 2013;4:139-51.
- [Google Scholar]
- The application of techniques of reiki, therapeutic touch and healing touch in cancer: A systematic review. Eur J Integr Med. 2012;4S:132.
- [Google Scholar]
- Biofield therapies for symptom management in palliative and end-of-life care. Am J Hosp Palliat Care. 2015;32:90-100.
- [Google Scholar]
- Effect of therapeutic touch in patients with cancer: A literature review. Med Arch. 2016;70:142-7.
- [Google Scholar]
- Why Does Spirituality Matter in End of Life Care? In: Das R, Nayak S, eds. Concepts of Palliative Care. Cuttack: A.K. Mishra Publishers; 2014. p. :72-80.
- [Google Scholar]
- Respecting the spiritual side of advanced cancer care: A systematic review. Curr Oncol Rep. 2015;17:6.
- [Google Scholar]
- How spirituality helps cancer patients with the adjustment to their disease. J Relig Health. 2015;54:1249-65.
- [Google Scholar]
- Religion, spirituality, and physical health in cancer patients: A meta-analysis. Cancer. 2015;121:3760-8.
- [Google Scholar]
- Patients' views of CAM as spiritual practice. Complement Ther Clin Pract. 2011;17:221-5.
- [Google Scholar]
- Spirituality and use of complementary therapies for cure in advanced cancer. Psychooncology. 2011;20:746-54.
- [Google Scholar]
- A systematic review of spiritually based interventions and psychoneuroimmunological outcomes in breast cancer survivorship. Integr Cancer Ther. 2016;15:405-23.
- [Google Scholar]
- The effects of spiritual interventions in patients with cancer: A meta-analysis. Oncol Nurs Forum. 2014;41:E290-301.
- [Google Scholar]
- Treatment of holistic suffering in cancer: A systematic literature review. Palliat Med. 2015;29:885-98.
- [Google Scholar]
- The effect of spiritual interventions addressing existential themes using a narrative approach on quality of life of cancer patients: A systematic review and meta-analysis. Psychooncology. 2016;25:253-65.
- [Google Scholar]






