Translate this page into:
Palliative Care for Patients with Nonmalignant Respiratory Disease
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nonmalignant respiratory diseases are chronic and life-limiting conditions that need holistic palliative care. Such patients not only have a variety of physical symptoms such as dyspnea, pain, cough, depression, and anxiety, but also have a number of psychosocial and spiritual issues, which are not addressed to by us. This leads to a poor quality of life. Hence, these patients require supportive palliative care to relieve their sufferings, but unfortunately such care is not available to them in our country. In this article, we have tried to discuss the barriers to the provision of palliative care to such patients and suggested some measures to overcome them.
Keywords
Chronic
need
palliative care
respiratory diseases
INTRODUCTION
Chronic respiratory diseases (CRDs) are diseases affecting the respiratory tract and lungs and include common ailments such as chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis, interstitial lung disease, and pneumoconiosis. Most of the research and guidelines are available for COPD patients, but these can also be applied to other diseases such as pulmonary fibrosis which are relatively less common.[1]
CRDs account for up to 8.3% of the overall burden of chronic diseases and adversely affect the quality of life (QoL) of suffer. It also leads to disability, loss of productivity, and increases economic burden for the sufferer and community.[2]
In recent years, due to rapid urbanization in the Asia Pacific region, the CRDs such as asthma, allergic disorders, and COPD are becoming a major health priority for the region.[3]
CRDs are progressive and irreversible, and available medical and surgical care facilities cannot completely cure it.[4] The prevalence of CRDs in India is difficult to estimate due to the size and diversity of the Indian population.[5] Recent reviews have reported allergies in 3% and COPD in 5%–8% of patients.[235] We can try to reduce the symptom severity without affecting long-term lung function or survival, but many of these patients continue to have symptoms despite best treatment modalities.[4] These patients also suffer from depression, reduces mobility, dyspnea, and inadequate social support, and leads to poor health-related QoL (HRQOL).[6] Various questionnaires like St. George's Respiratory Questionnaire and the CRD Questionnaire have been frequently used to assess HRQOL in respiratory diseases.[78] Interventions such as rehabilitation and improvement in interpersonal relationships improve the QoL in these patients. Various recent studies have suggested that the health status of patients with CRDs is as worse than death because of significantly reduced daily activities, severe dyspnea, fatigue, pain, anxiety, and depression.[146] The burden on the economy of CRDs as estimated by the number of patients presenting for treatment is comparable to lung cancers.[89]
Palliative care takes care of not only physical symptoms, but also psychosocial and spiritual components of suffering and it is required to improve HRQOL in these patients. However, despite best of the efforts, traditional practice of curative intent with provision of palliative care during the terminal phase of life is virtually nonexistent.
By the virtue of this article, we have tried to highlight the palliative and end-of-life care needs for patients with CRDs. A PubMed search conducted by the authors of this review in January 2017 found 200 articles related to palliative care in nonmalignant respiratory disease. Out of these, 152 articles were published after January 2000.
PALLIATIVE CARE NEEDS IN PATIENTS WITH RESPIRATORY DISEASE
CRDs not only affect the patient but also the near relatives and friends. The various treatment needs of the patient (physical, social, psychological, and spiritual) will vary according to disease type.[1011] Patients with CRD have an “organ system failure” trajectory and typically have a waxing and waning type of disease progression with repeated attacks of acute exacerbation along with chronic respiratory failure.[1011] The patients’ symptoms are partly controlled with treatment, but their psychological suffering and disease severity progress with every acute exacerbation. Prognosis of the disease has been taken as a benchmark for allocating palliative care services worldwide.
The patients expected to live <6 months should be given benefits to have a peaceful death. However, this prognosis is easier to estimate for patients with cancer than the patients with CRD. The decision to introduce palliative care services in a COPD patient may be taken on the basis of a flowchart [Figure 1].[12]
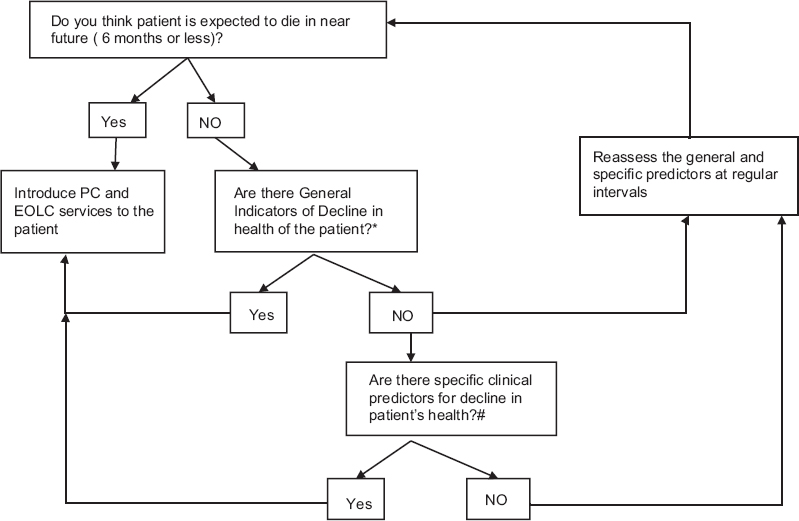
- When to introduce palliative care services to a patient with chronic respiratory disease. *General indicators of decline: ↓ Functional performance status, ↑ bed or chair (50% of day) and dependence in most activities of daily living, advanced unstable, deteriorating symptom burden, ↓ response to treatments and reversibility, absence of further active treatment, progressive weight loss (>10%) in the past 6 months, repeated emergency admission and low serum albumin (<2.5 mg/dl). #Specific predictors (at least two of the below): severe disease (FEV1 < 30%); recurrent hospital admission due to chronic obstructive pulmonary disease (>3 in the last 12 months); cor pulmonale; requirement of oxygen therapy; Medical Research Council Dyspnea Scale 4 or 5; previous admission to Intensive Care Unit for noninvasive ventilation; depression; systemic steroids given for more than 6 weeks in the preceding 12 months
Some of these may be useful in identifying palliative care needs of patients with other CRDs also. However, the accuracy of these indicators is still limited and research is still continuing. Recent studies have suggested that the mortality of patients admitted in the Intensive Care Unit (ICU) with exacerbation is high, and one should consider patients admitted with acute exacerbation for palliative care and end-of-life counseling.[1314]
Most of the physicians can effectively manage the clinical symptomatology but they hardly discuss the long-term prognosis and the end-of-life issues with the patients. Moreover, there are a lot of ethical problems while treating acute exacerbation of end-stage disease. It is always a difficult decision to intubate the patient because various factors such as age, respiratory muscle weakness, hypercapnia, hypoxia, malnutrition, and treatment with corticosteroids or other agents may decrease the possibility of weaning.[15] A recent retrospective study evaluating long-term survival in patients showed that 5-year survival in patients treated with noninvasive ventilation (NIV) for the first time was only 26% only, which is comparable to many of the cancers.[16] Moreover, after recovering from acute phase, they still require intensive nursing and respiratory physiotherapy for months. Most patients after discharge consider their life as rather poor and are depressed and most of these patients die in restricted environment of hospital ICU's away from their relatives.[17] Various authors have reported that the health status (physical, social, and emotional) of patients with severe COPD and activities of daily living were significantly worse than those with lung cancers. Moreover, the psychological symptoms of anxiety and depression were also significantly greater than the patients with lung cancer. Despite a high incidence of psychological disturbance (90%) in these patients, only a few (4%) of these receive pharmacological treatment. The depressed patients may refuse life-sustaining treatment and have a higher mortality (adjusted hazard risk 1.93).[18] Treatments of psychological symptoms may make them change their preference about end-of-life treatment.[19]
Despite the ever-increasing population of patients, patients of elderly age, and difficulties in predicting the disease progression, these patients never receive palliative care in our country. The palliative care services are in the early stage of development and are mainly concentrated for cancer patients. Hospices in other parts of the world do consider the admission of such patients for care. Recently published NICE guidelines have also addressed palliative care needs of such patients.[20] Hence, we should also address palliative care needs of these patients and have guidelines for the same. Moreover, it is important to discuss end-of-life issues with these patients well in advance so that they have a peaceful and less stressed death. Hence, a holistic approach toward treatment of such patients is the need of the hour along with symptom control.
SYMPTOMS AND THEIR MANAGEMENT
Chronic end-stage respiratory diseases are commonly associated with symptoms such as breathlessness, cough (productive/nonproductive), hemoptysis, anxiety, stridor, fever, infection, and chest pain. The complete cure of these symptoms may not be possible in most of the cases, but the overall physical and psychological improvement does occur with pharmacological interventions and counseling.
Breathlessness or dyspnea
This term is used to describe difficult, uncomfortable, or labored breathing. This is one of the most distressing symptoms of patients with CRDs. Prolonged hypoxia, hypercapnia, and acidosis stimulate the respiratory receptors in the brain stem leading to increased ventilation and sensation of awareness of breathing. The severity of dyspnea depends on patient's psychology, personality, and cognitive function and is often related to previous experiences. In the Study to Understand Prognoses and Preferences for Outcomes and Risks Treatment (SUPPORT), most of the patients had dyspnea in the last 3 days of their lives.[202122]
Assessment of dyspnea
A good history and physical examination should be done to rule out the nonrespiratory causes of dyspnea (heart, neuromuscular, and psychological). Common clinical indicators such as arterial blood gas, pulse oximetry, and spirometry values (baseline and postbronchodilator) do not correlate well with the severity of dyspnea. Many scales are now available to quantify dyspnea such as the Medical Research Council dyspnea scale, visual analog scale (1 to 10), and verbal numerical.[232425] However, none of them measures patient-reported outcome measures due to breathlessness in patients during their activities of daily living (ADL). Hence, objective assessment of therapy in such patients is difficult. Recently, the London Chest Activities of Daily Living Scale (LCADL) questionnaire was tested in 105 patients with refractory breathlessness of any cause and found it reliable and valid to measure the effect of refractory breathlessness on their ADLs.[26] Authors also demonstrated that LCADL correlated well with other scores such as HRQL, functional status, and exercise capacity. However, they could not find any correlation between pulmonary function tests (PFTs) and the LCADL and further supported that the PFTs do not correlate with the severity of dyspnea and are not a good measure to guide the treatment.
Symptomatic relief of dyspnea is best by the treatment of the underlying pathophysiology. But, as the terminal phase of the patient approaches, our therapy should be focused on providing symptomatic relief to the patient not cure.
Treatment
The treatment modalities of breathlessness should be discussed with the patient before he/she reaches the terminal stages. The breathlessness can increase in severity over time and patients often fear that they will be struggling to breathe before their death. There is a strong emotional and psychological component that leads to fear and anxiety in these patients. Every effort should be done to reduce the distress and counsel the patient. The physiological symptom can be primarily treated by oxygen supplementation and drugs such as opioids (oral, intravenous, subcutaneous, and nebulized) and anxiolytics which tend to decrease central drive and give symptomatic relief.[272829] Most of the physicians are concerned that opioids may cause respiratory depression and hasten death. However, various studies have suggested that there is no evidence to suggest this. Hence, relief of suffering from dyspnea by the use of opioids justifies their use in appropriate doses.[30] The health-care provider should titrate the doses of opioids (quantity and frequency) to relieve dyspnea and avoid using excessive doses. A recently published systematic review has suggested that oral or injectable opioid drugs may help in the treatment of the symptoms of breathlessness with some associated side effects such as nausea, drowsiness, and vomiting.[31] However, it has been suggested that there is no evidence for the effectiveness of nebulized opioids in terminal dyspnea. Furthermore, due to lack of quality evidence, more research is needed on the usage of opioids in terminal dyspnea to observe its effects on QoL.
Inhaled bronchodilator medications (b2 agonists, steroids, and muscarinic receptor agonists) along with ventilatory support (continuous positive airway pressure, NIV, and bilevel positive airway pressure) tend to reduce the work of breathing. Nonpharmacological measures such as acupuncture, breathing exercises, proper nutrition, desensitization, and counseling of patients have also been effective.[323334]
The patients should also be encouraged to take good nutrition and join pulmonary rehabilitation programs in the early stages of their disease.[3536]
Cough
Cough is an uncommon yet distressing symptom in end-stage nonmalignant respiratory diseases. In patients with CRDs, the mucociliary transport is impaired and cough is responsible for the airway clearance. It is a protective mechanism initiated by receptors in the large airways and helps in clearing secretions and prevents foreign material entry into lower respiratory tract. However, excessive cough can be distressing to the patients and needs to be investigated for proper management.
This can be effectively managed by multimodal approach which includes:
-
Proper hydration and steam inhalation
-
Physiotherapy[37] and suctioning
-
Mucolytics: N- acetylcysteine, etc.[38]
-
Minitracheostomy to facilitate clearing of tracheal secretions
-
Antitussive agents: Various drugs such as opioids (morphine, methadone, codeine, and dextromethorphan), oral local anesthetics, inhaled local anesthetics, sodium cromoglycate, theophylline, and bronchodilator agents may be useful for the treatment of cough.[35394041]
Chest pain
Chest pain is a common symptom of CRDs and may add to the agony of the patient, decrease ventilatory excursion, and may impair the ability to cough. This may be due to musculoskeletal disorders (rib fractures, muscle fatigue, localized inflammation, etc.), pleuropulmonary (inflammation of parietal pleura) or visceral (ischemic heart disease, esophagitis, cholecystitis, anxiety, etc.). A thorough assessment of pain (onset, severity, localization, character, time course, and exacerbating and reliving factors) should be done before starting any therapy. Irrespective of the cause, the WHO guidelines for analgesic prescription in pain needs to be followed.[42] Local nerve blocks; epidural, oral nonsteroidal antiinflammatory drugs, and opioids have all been tried effectively.[43]
Hemoptysis
It is a life-threatening complication which occurs commonly in bronchiectasis and mostly due to infection.[44] Hemoptysis >600 ml in 4 h is associated with a high mortality. The initial resuscitation to maintain the airway and circulation is required to stabilize the patient. Due to the terminal nature of the disease, the medical management (bronchoscopic cold saline lavage, balloon tamponade, tranexamic acid, etc.) is deployed to control the bleeding.[45]
Respiratory failure
All the nonmalignant respiratory diseases are associated with episodes of respiratory failure. These patients typically undergo ICU admissions and ventilatory support to tide over-tide crisis. The need for advanced life support measures need to be discussed in advance with the patients and their family.
Psychological symptoms
Anxiety and depression may be increased in CRD due to an inability to go out socially, affected ADL, and loss of muscle strength (LCADL).[46] Anxiety is found to be more common in patients with CRD such as COPD and may increase the rates of exacerbations leading to hospitalization, decreased HRQOL, and affect survival rates after emergency treatment.[4748]
One should try to assess and improve mental health by psychological therapy to improve HRQOL in patients with CRD.[49]
BARRIERS TO EFFECTIVE PALLIATIVE CARE IN CHRONIC NONMALIGNANT RESPIRATORY DISEASES
The decision to switch from curative treatment to palliative care in nonmalignant respiratory diseases is often difficult. This is because of a number of reasons mentioned below.
Unlike malignant diseases, the course of disease and its prognosis in patients with nonmalignant respiratory disease is often unpredictable. The SUPPORT study over 4000 patients with one or more of nine life-threatening diagnoses was analyzed.[39] The patients with COPD were much more likely to die in the ICU on mechanical ventilation. Moreover, the prediction of survival using APACHE II score was overestimated for CRDs. Even as close as 5 days before death, patients with COPD were predicted to have a >50% chance of surviving for 6 months whereas those with lung cancer were predicted to have a <10% chance.
Not only timing the death is difficult, but withdrawing life support may also not be easy. There is always a hope of recovery of the patient, the team members often do not agree on the patients’ treatment plan and are reluctant to communicate the poor prognosis of the patient.
The health-care professionals often are reluctant to discuss the prognosis in the absence of objective criteria and also not prepared to discuss such issues with the patients and their family. Hence, the communication of bad news is avoided till the end of life.
The patients also are not comfortable discussing the issues related to their death. They prefer to go to only those physicians who tend to falsely provide the hope for treatment and complete cure.
Worldwide, the access to palliative care services to the patients with nonmalignant respiratory disease is limited because of lack of resources and nonavailability of palliative care programs for nonmalignant conditions. Wong et al. have found that COPD patients had significantly worse ADL and physical, social, and emotional functioning than malignant lung cancer patients.[3] However, only a few of them were counseled or received care of palliative care specialist.
COMMUNICATION
Physicians providing palliative care for patients with CRD should communicate with the patients and their family to discuss appropriate treatment plan. The sensitive issues such as patient concerns regarding end-of-life care and withholding or withdrawing medical treatment should be discussed in detail. Every effort should be made to counsel the patients psychologically and remove their misconceptions about getting complete cure and eventual death. These issues are important for the patients and should be handled sensitively. The decision arrived should be well communicated to the family, the treating team, and hospital.
The patients should also be made to understand that it is difficult to separate palliative care from curative care. In fact, the curative and palliative needs in chronic nonmalignant respiratory diseases run parallel throughout the course of the specific disease and need to be addressed simultaneously. We should try to develop a holistic care model integrating the principles of palliative and curative care and establish a co-ordination between the primary, secondary, and tertiary care providers.
FUTURE RECOMMENDATIONS
The principles of palliative care should be included in the management framework of CRDs. This will ensure that the palliative needs of the patient are addressed at the time of presentation to the physician. The palliative care services must accept referrals based on need of the patient rather than diagnosis, i.e., the facilities should not be restricted to only cancer patients.
Undergraduate medical and nursing students should be sensitized to the core principles of palliative care for patients with and without malignant diseases. At our institute, we have started the basic teaching in palliative care to undergraduate students. This will go a long way in sensitizing the young doctors toward amalgamating the palliative care goals in the curative strategies at early stage of patient treatment.
The certificate courses should be developed to help physicians in dealing with palliative issues of nonmalignant respiratory diseases. We can have a basic module common for all variety of diseases and an advanced system-specific module to help all the medical fraternity be appraised with palliative care principles.
The palliative management of various nonmalignant diseases should be included in the curriculum of the postgraduates, irrespective of the specialty.
Public health awareness campaigns should be done throughout the country from time to time to sensitize them with palliative care needs of various diseases, the importance of discussing the end-of-life care, and home-based care of patients with chronic diseases. This becomes important, especially for our country, where the number of patients is much more than available health-care services. This can reduce the unnecessary burden on health-care services and also help the patients with acute decomposition to get the required attention.
CONCLUSION
As health-care professionals, we should increase public awareness on palliative needs of CRDs. The patients and their relatives should be counseled about end-of-life care and must be given support if they choose to die at home. The physicians should be trained to improve communication with the patients and their relatives. Systematic approach should be designed to help physicians in decision-making for symptomatic relief of patients regardless of diagnosis.
More studies are required to find the needs of patients and their relatives near the end of life and methods to achieve them.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Living with severe chronic obstructive pulmonary disease (COPD): Perceptions of patients and their carers. An interpretative phenomenological analysis. Palliat Med. 2004;18:619-25.
- [Google Scholar]
- World Health Organization. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Report. Geneva: World Health Organization; 2007.
- Changing prevalence of allergic diseases in the Asia-Pacific region. Allergy Asthma Immunol Res. 2013;5:251-7.
- [Google Scholar]
- Palliative care for patients with chronic respiratory disease. Nurs Stand. 2011;26:41-6.
- [Google Scholar]
- Prevalence of COPD in India: A systematic review. Prim Care Respir J. 2012;21:313-21.
- [Google Scholar]
- How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer. Thorax. 2000;55:1000-6.
- [Google Scholar]
- A self-complete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis. 1992;145:1321-7.
- [Google Scholar]
- A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773-8.
- [Google Scholar]
- Palliative care for patients with non-malignant end stage respiratory disease. Thorax. 2000;55:979-81.
- [Google Scholar]
- Perspectives on care at the close of life. Serving patients who may die soon and their families: The role of hospice and other services. JAMA. 2001;285:925-32.
- [Google Scholar]
- Prognostic Indicator Guidance. The Gold Standards Framework Centre in End of Life Care. 2011
- [Google Scholar]
- 2008. On Behalf of the National COPD Audit 2008 Steering Group. Report of the National Chronic Obstructive Pulmonary Disease Audit 2008: Resources and Organisation of Care in Acute NHS Units Across the UK. Available fron: http://www.tinyurl.com/3qwok82
- Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax. 2004;59:1020-5.
- [Google Scholar]
- Weaning through noninvasive mechanical ventilation. In: Hill N, Levy MM, eds. Ventilatory Management Strategies for Critical Care. New York: Dekker Inc; 2001. p. :579-609.
- [Google Scholar]
- Five-year outcome in COPD patients after their first episode of acute exacerbation treated with non-invasive ventilation. Respirology. 2010;15:1084-91.
- [Google Scholar]
- Last 3 months of life in home-ventilated patients: The family perception. Eur Respir J. 2010;35:1064-71.
- [Google Scholar]
- Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167:60-7.
- [Google Scholar]
- Factors associated with change in resuscitation preference of seriously ill patients. The SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Arch Intern Med. 1996;156:1558-64.
- [Google Scholar]
- 2004. NICE Guideline (G12): Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care. Available from: http://www.guidance.nice.org.uk/CG12
- Perceptions by family members of the dying experience of older and seriously ill patients. SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med. 1997;126:97-106.
- [Google Scholar]
- Dying with lung cancer or chronic obstructive pulmonary disease: Insights from SUPPORT. Study to understand prognoses and preferences for outcomes and risks of treatments. J Am Geriatr Soc. 2000;48(5 Suppl):S146-53.
- [Google Scholar]
- Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581-6.
- [Google Scholar]
- Assessment of dyspnea in advanced cancer patients. Support Care Cancer. 1999;7:229-32.
- [Google Scholar]
- Verbal numerical scales are as reliable and sensitive as visual analog scales for rating dyspnea in young and older subjects. Respir Physiol Neurobiol. 2007;157:360-5.
- [Google Scholar]
- Breathlessness during daily activity: The psychometric properties of the London chest activity of daily living scale in patients with advanced disease and refractory breathlessness. Palliat Med 2016 pii: 0269216316680314
- [Google Scholar]
- Subcutaneous morphine for dyspnea in cancer patients. Ann Intern Med. 1993;119:906-7.
- [Google Scholar]
- Continuous intravenous infusion of morphine for severe dyspnea. South Med J. 1991;84:229-34.
- [Google Scholar]
- Nebulised morphine for severe interstitial lung disease. Cochrane Database Syst Rev. 2002;3:CD002872.
- [Google Scholar]
- Narcotic and benzodiazepine use after withdrawal of life support: Association with time to death? Chest. 2004;126:286-93.
- [Google Scholar]
- Opioids for the palliation of refractory breathlessness in adults with advanced disease and terminal illness. Cochrane Database Syst Rev. 2016;3:CD011008.
- [Google Scholar]
- Noninvasive mechanical ventilation via face mask in patients with acute respiratory failure who refused endotracheal intubation. Crit Care Med. 1994;22:1584-90.
- [Google Scholar]
- Cold facial stimulation reduces breathlessness induced in normal subjects. Am Rev Respir Dis. 1987;136:58-61.
- [Google Scholar]
- Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life. A systematic review. J Pain Symptom Manage. 2000;20:374-87.
- [Google Scholar]
- Randomized controlled trial of pulmonary rehabilitation in severe chronic obstructive pulmonary disease patients, stratified with the MRC dyspnoea scale. Eur Respir J. 1998;12:363-9.
- [Google Scholar]
- Pulmonary Rehabilitation for Chronic Obstructive Pulmonary Disease. Cochrane Database Syst Rev. 2002;3:CD003793.
- [Google Scholar]
- Managing cough as a defense mechanism and as a symptom. A consensus panel report of the American College of Chest Physicians. Chest. 1998;114(2 Suppl):133S-81S.
- [Google Scholar]
- Recommendations for the management of cough in adults. Thorax. 2006;61(Suppl 1):i1-24.
- [Google Scholar]
- ABC of palliative care. Breathlessness, cough, and other respiratory problems. BMJ. 1997;315:931-4.
- [Google Scholar]
- Benzoate for opioid resistant cough and other respiratory problems. Palliat Med. 1998;12:55-8.
- [Google Scholar]
- 2011. World Health Organization: WHO's Pain Ladder. Available from: http://www.who.int/cancer/palliative/painladder/en/
- Treating severe pain in advanced lung disease. In: Ahmedzai SH, Muers MF, eds. Supportive Care in Respiratory Disease. Vol 1. Oxford: Oxford University Press; 2005. p. :439-52.
- [Google Scholar]
- Hemoptysis: Etiology, evaluation, and outcome in a tertiary referral hospital. Chest. 1997;112:440-4.
- [Google Scholar]
- Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205-11.
- [Google Scholar]
- Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8:108.
- [Google Scholar]
- Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122:1633-7.
- [Google Scholar]
- Effects of medical and psychological treatment of depression in patients with COPD – A review. Respir Med. 2011;105:1422-33.
- [Google Scholar]






