Translate this page into:
The Effect of Honey on Radiation-induced Oral Mucositis in Head and Neck Cancer Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
The aim of this study is to evaluate the effect of honey on clinically scoring grades of oral mucositis.
Materials and Methods:
This interventional study was carried out in Radiation Oncology Department of Mayo Hospital, Lahore. In this study, 82 patients of both genders, of head and neck cancer, planned for radiotherapy, were divided into two groups by random sampling numbers. Patients in both groups were treated with a total dose of 60–78 Grays in 4–6 weeks. In treatment group, patients were instructed to take 20 mL of honey. In control group, they were advised to rinse with 0.9% of saline. Patients were evaluated every week to assess the grades of oral mucositis up to 6 weeks. The assessment tool was Radiation Therapy Oncology Group Grading System. The statistical analysis was done by Chi-square test.
Results:
In honey-treated group, the proportion of mucositis (Grades 3 and 4) was lower and statistically significant as compared to control group at the end of 6 weeks of radiation.
Conclusion:
This study showed that oral intake of honey during radiotherapy is valuable in the reduction of severity of oral mucositis.
Keywords
Honey
oral mucositis
Radiation Therapy Oncology Group
radiotherapy
INTRODUCTION
Head and neck cancer is the eighth common type among all cancer types all over the world.[1] The treatment comprises surgery, radiotherapy, chemotherapy or a combination escorted by restoration therapy, and social support.[2] Radiotherapy leads to irreversible loss of the reproductive integrity, the cell cycle necessary for cell growth, apoptosis, and necrosis of cancer cells.[3] Conventional fraction size ranges from 1.8 to 3 Grays (Gy) per fraction over 4–6 weeks.[4] The accumulative dose of radiation for the primary treatment of head and neck cancer treatment is 60–70 Gy, depending on the irradiation of the tumor.[5]
Radiation affects malignant cells and is also absorbed by the oral mucosa and gastrointestinal mucosa, especially in rapidly dividing cells.[6] Oral mucositis is the most frequent, distressing, painful, clinical side effect of radiotherapy.[7] It is defined as an inflammatory lesion of oral mucosa resulting from the cancer therapy typically manifesting as atrophy, swelling, erythema, ulceration, and pseudomembrane formation.[89] It is described in five overlapping stages: initiation, upregulation, message generation, ulceration, and healing.[910]
Radiation-induced oral mucositis shows hyperkeratosis of the oral mucosa after the dose of 10–20 Gy.[68] Erythema is the first clinical sign seen on the oral mucosa, and severity of mucositis reaches at a dose of 30 Gy. After the completion of radiotherapy, the symptoms abate in 2–6 weeks.[1112] Effective management of oral mucositis is very important.[1314]
Honey is an important traditional medicine and prophylactic agent that has numerous beneficial health properties including its ability to facilitate healing.[1516] Honey helps in the reduction of ulceration and inflammation of the biological process of mucositis.[1718] Honey has been used to manage burns, oral infections, surgical wounds, and pressure wounds.[1920] In this study, honey was obtained from the Zoology Department, The University of Punjab. Honey was applied to the oral mucosa of patients undergoing radiotherapy which is beneficial in limiting the severity of oral mucositis. Honey is a natural product with rich nutritional properties that is economical and a pleasant agent for managing mucositis.
MATERIALS AND METHODS
A unicenter, randomized controlled, clinical human study was conducted at Clinical Oncology Department of Mayo hospital, Lahore, Pakistan. The study protocol was approved by the Advanced Studies and Research Board of University of Health Sciences, Lahore, and Ethical Committee of PGMI, Lahore. It was carried out from January 2014 to January 2015.
Inclusion criteria
Patients with histologically confirmed head and neck cancer planned for external beam radiotherapy, with a total radiation dose of 60–70 Gy (in 5–6 weeks).
Exclusion criteria
Patients having xerostomia, systemic diseases, and oral sores due to ill-fitting dentures were excluded from the study.
Eighty-two patients were selected for the study, divided into two groups as control and treatment groups by computer-generated random numbers. Complete history taking of patients and physical examination were done including oral and dental evaluation before radiotherapy. Signatures on the consent form were obtained as per ethical requirement of the study after explaining the whole procedure. All patients were strictly instructed to avoid smoking, chewing pan and spicy food, and to maintain oral hygiene during the study.[16] Areas exposed to radiation were marked by surface marking in both groups. Both single- and multi-fields were used in this study. The radiations were delivered at a dose of 1.8–2 Gy 5 days in a week. Equinox and Telecobalt Theratron 780C machines were used.
In the treatment group, patients were given 20 mL of Ziziphus honey, 15 min before and after the radiotherapy.[1221] They were instructed to swallow slowly to smear the layer of honey on the oral and pharyngeal mucosa. Patients were also advised to take 20 mL of Ziziphus honey before sleeping in the night.[22] This treatment protocol of honey was followed from day 1 of radiation till the end of 6th week. They were instructed to take meals in the early morning, noon, and night not to interfere in such a manner not to interfere with ingestion of honey. ingestion of honey at least ½ h ingestion of honey. In the control group, patients were given 20 mL of 0.9% of saline 15 min before and after radiotherapy.[22] They were advised to rinse saline. They were instructed to keep saline for at least 5 min duration and then to spit it out. They were advised to rinse 20 mL of saline in the same manner before sleeping. This treatment protocol of saline was followed from day 1 of radiation till 6 weeks.
All patients were evaluated subjectively and clinically for the development of oral mucositis. The evaluation of oral mucosa of the patients was done with a battery-operated torch after every week for grading of oral mucositis in both groups. The assessment scale used in this study was Radiation Therapy Oncology Group (RTOG) Grading System.[1218] All patients were given dietary counseling throughout the course. A nasogastric tube was placed in patients with severe Grade 4 mucositis. Statistical analysis was done by Chi-square method using SPSS software version 20.0 (IBM, Chicago, Illions).
Saline was the therapeutic agent in control group. Ziziphus honey used in this study was analyzed by the Pakistan Council of Scientific and Industrial Research. The moisture content of this honey was 17.34%. Specific gravity was 1.420. Hydroxymethylfurfural was 28.42 mg kg, pH was 6.05, and diastase number was 44.
RESULTS AND DATA ANALYSIS
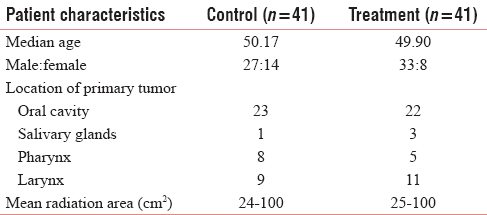
The characteristics of patients including sex, age, and location of primary tumor are presented in Table 1.
In the control group, four patients in the 4th week and two patients in the 5th week took nystatin along ibuprofen tablets. One patient in control group in 3rd week and two patients in study arm group refused to continue their radiotherapy treatment.
The oral cavity of all the patients was examined weekly up to 6 weeks in both control and honey-treated groups. The examination was done with the help of a battery-operated torch. The grading of oral mucositis was assessed by Radiation Therapy Oral Mucositis Grading (RTOG).
In treatment group, twenty lesions of Grade 0 mucositis in week 1 were observed. This number decreased by the end of 6th week. In control group, however, 32 lesions of Grade 0 mucositis were observed in week 1. This number decreased till week 3, but increased from week 3 till 6. In week 1, the number of Grade 1 oral mucositis was 7 and its frequency increased till the end of 6th week in treatment group [Table 2].

Grade 3 oral mucositis was observed at the end of 3rd week of radiotherapy when compared to control group where it was observed at the end of 2nd week. The total number of Grade 3 oral mucositis in treatment group at the end of 6th week was 17 less than control group Grade 3 lesions (50). At the end of week 3, only 1 Grade 4 mucositis was observed in treatment group, but in control group, the number was 2. In control group, the number increased in week 4 and week 5. In total, after 6 weeks, 19 Grade 4 oral mucositis were present in control group and 3 in treatment group.
During the course of radiotherapy in weeks 4 and 5, there was a significant reduction of oral mucositis in treatment group as compared to control group as illustrated in Tables 3 and 4. At the end of 6th week, the difference of Grades 3 and 4 was statistically significant among control and treatment groups (P value of Grade 3 mucositis: 0.016 and P value of Grade 4 mucositis: 0.032).


DISCUSSION
Radiotherapy rays are absorbed by the oral mucosal cells which leads to the development of a debilitating condition which is known as oral mucositis.[9] The symptoms begin with erythema, diffuse ulcers leading to pseudomembrane formation. Gram-negative bacilli in oral flora release endotoxins that contribute as potent mediators in the inflammatory process of mucositis. Patients are unable to chew and swallow in case of acute oral mucositis.[10] Swallowing difficulties lead to weight loss, dehydration, and also need for nutritional support. It has an impact on the treatment plan and prognosis of the disease, both affecting the efficacy of radiotherapy.[7]
The basic management of oral mucositis is still symptomatic with the aim to relieve pain and discomfort associated with it, comforting of the oral mucosa by applying a chemical agent to eradicate the microorganisms, and stimulation of epithelization.[23] The most common controlling pathway of oral mucositis is use of saline mouth rinses, opioid analgesics, ice chips, and topical applications of lidocaine and benzydamine hydrochloride mouth washes (anti-inflammatory agents) and cytoprotective agents.[23] Nystatin and lignocaine are the most common agents used in Mayo Hospital, Lahore, for the treatment of mucositis.
Honey is a heterogeneous mixture of proteins, flower nectar sugars, and glandular secretions produced by honey bees. It has a powerful impact on the proliferation of B-lymphocytes and T-lymphocytes and also in the activation of macrophages.[16] It inhibits inflammatory process by inhibiting cyclooxygenase pathway because it is the main pathway of inflammation. It stimulates the process of granulation tissue, angiogenesis, rapid epithelization and proliferation of fibroblasts.[21] Certain enzymes, phytochemical agents (methylglyoxal and methyl syringate), low pH, defensin, a peptide, and high osmolarity are distinct mechanisms involved in the bactericidal activity of honey.[23]
The present study showed promising effects of honey for substantial reduction in the severity of RTOG Grade 3 and 4. The findings of this study were also comparable with the positive results of Biswal. The results of Biswal's study revealed that there was statistically significant reduction in patients with Grade 3 and 4 mucositis.[12] Another study conducted in 2004 by Motallebnejad et al. portrayed that mucositis score at the end of each week was lower than the control group.[16] A study by Khannal et al. (2010)[24] described the importance of honey on limitation of radiation-induced mucositis and showed that only one patient developed intolerable mucositis in study group as compared to 15 intolerable mucositis in lignocaine group.[21]
There are some limitations to our study. The study was unicentric in nature and patients were heterogeneous regarding cancer treatment (fractioned and hyperfractioned radiation therapy), age, and tumor location. There is disparity in assessment and management of oral mucositis due to complex multi-factors related to the patients and treatment to the complex multifactorial patient and treatment factors related to oral mucositis, there is disparity in the assessment and management of oral mucositis. The data available on effect of honey on limitation of radiation-induced oral mucositis depicted that honey had promising effects on protection of oral mucosa from radiations.
CONCLUSION
The results of this study showed that Ziziphus honey significantly reduced the severity of mucositis in treatment arm. It is really encouraging to note that patients of head and neck cancer suffering from severe mucositis due to radiotherapy can be lessened to a great extent simply by such a feasible and affordable option.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
All authors would like to thank Professor Khalid Masood Gondal, Head of Department of Radiotherapy, King Edward Medical University; Professor Fozia Farzana, Head of Anatomy Department, Postgraduate Medical Institute, Birdwood, Lahore; and Professor Riaz Ahmed Warraich, Head of Department of Oral and Maxillofacial Surgery, for their guidance and encouragement, in carrying out this project.
REFERENCES
- Molecular pathology of head and neck cancer: Implications for diagnosis, prognosis, and treatment. Annu Rev Pathol. 2009;4:49-70.
- [Google Scholar]
- Value considerations in the treatment of head and neck cancer: Radiation, chemotherapy, and supportive care. Am Soc Clin Oncol Educ Book. 2014;16:e296-303.
- [Google Scholar]
- Cell death pathways in directly irradiated cells and cells exposed to medium from irradiated cells. Int J Radiat Biol. 2013;89:182-90.
- [Google Scholar]
- Conventional radiotherapy with concurrent weekly cisplatin in locally advanced head and neck cancers of squamous cell origin – A single institution experience. Asian Pac J Cancer Prev. 2013;14:6883-8.
- [Google Scholar]
- Altered and conventional fractionated radiotherapy in locoregional control and survival of patients with squamous cell carcinoma of the larynx, oropharynx, and hypopharynx. Croat Med J. 2006;47:42-52.
- [Google Scholar]
- Cancer treatment-induced oral mucositis: A critical review. Int J Oral Maxillofac Surg. 2012;41:225-38.
- [Google Scholar]
- Oral mucositis in patients undergoing radiation treatment for head and neck carcinoma. Cancer. 2006;106:329-36.
- [Google Scholar]
- Local and systemic pathogenesis and consequences of regimen-induced inflammatory responses in patients with head and neck cancer receiving chemoradiation. Mediators Inflamm 2014 2014:518261.
- [Google Scholar]
- Topical application of honey in the management of radiation mucositis: A preliminary study. Support Care Cancer. 2003;11:242-8.
- [Google Scholar]
- New developments in management of oral mucositis in patients with head and neck cancer or receiving targeted anticancer therapies. Am J Health Syst Pharm. 2012;69:1031-7.
- [Google Scholar]
- Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2010;8:CD001973.
- [Google Scholar]
- The effect of topical application of pure honey on radiation-induced mucositis: A randomized clinical trial. J Contemp Dent Pract. 2008;9:40-7.
- [Google Scholar]
- Moisture content in honey determination with a shear ultrasonic reflectometer. J Food Eng. 2010;96:93-6.
- [Google Scholar]
- Honey as topical prophylaxis against radiochemotherapy-induced mucositis in head and neck cancer. J Laryngol Otol. 2009;123:223-8.
- [Google Scholar]
- The evidence supporting the use of honey as a wound dressing. Int J Low Extrem Wounds. 2006;5:40-54.
- [Google Scholar]
- Comparative in vitro study of honey based and silver based wound preparations on cell viability. Burns. 2010;36:1036-41.
- [Google Scholar]
- Evaluating the effectiveness of topical application of natural honey and benzydamine hydrochloride in the management of radiation mucositis. Indian J Palliat Care. 2012;18:190-5.
- [Google Scholar]
- Prevention and management of radiation-induced dermatitis, mucositis, and xerostomia. Am J Health Syst Pharm. 2013;70:1025-32.
- [Google Scholar]
- Effect of topical honey on limitation of radiation-induced oral mucositis: An intervention study. Int J Oral Maxillofac Surg. 2010;39:1181-5.
- [Google Scholar]






