Translate this page into:
Defining the Role of Physiotherapy in Palliative Care in Multiple Sclerosis
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
With increasing prevalence of multiple sclerosis worldwide, India too has transitioned from low to medium prevalence region. This increases the overall burden of a number of people suffering from a chronic progressive disorder. Such scenario underlines the need for an early comprehensive and holistic patient management plan, aiming to provide a better quality of life. The presented case is one such example of a patient-centered, and interdisciplinary team approach for better management of a patient suffering from an incurable, progressive disorder. As physiotherapists tend to spend a considerable amount of time with their patients on a regular basis, it becomes imperative to view all the patient related problems from a wider angle and endeavor to address each of them individually/collaboratively. In a palliative care setting, physiotherapy can no longer be considered as only physical symptom management approach but a patient care approach considering their entire physical, emotional, psychosocial, and spiritual needs. This novel case report shall serve as a guiding strategy for physiotherapists to work in the domain of palliative care.
Keywords
Interdisciplinary approach
Multiple sclerosis
Palliative care
Patient-centered physiotherapy
INTRODUCTION
Traditionally palliative care has focused on oncology patients, WHO defines palliative care as “an approach that improves the quality of life (QOL) of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”[1] Non oncology patient groups with rapidly progressing disorders also need palliative care. Multiple sclerosis (MS) is a chronic, inflammatory, incurable disease of the central nervous system The amount of sufferings in MS patients' from their “burden of symptoms” is comparable with that of cancer patients requiring palliative care.[2] Hence, it is imperative to recognize the needs of MS patients.[3] In nutshell neurorehabilitation and palliative care play a vital role beyond disease modifying treatments in addressing regularly changing physical, social, psychological and spiritual needs of MS patients. We highlight a case of MS, who suffered from a wide array of symptoms, affecting her overall QOL. In our opinion, such patients are apt candidates for palliative care from the physiotherapeutic aspect.
CASE REPORT
A 40-year-old homemaker presented with a history of relapsing-remitting MS from past 6 years. She had her third relapse in November 2014, which resulted in reduced vision in left eye and an overall decrease in her physical abilities. Prior to this recent attack she was an avid Zumba dancer and could manage household work without assistance. However, now she complained of difficulty in walking independently, frequent urination, and increasing brain dullness. Her magnetic resonance imaging revealed two periventricular noncontrast-enhancing lesions in addition to a contrast-enhancing lesion in the left optic nerve. There was a contrast-enhancing partial segmental lesion in the mid-thoracic spinal cord at the level of T7–T10. Her physical examination revealed paresthesia in both her feet, impaired balance on ambulation. She scored 6 on the Kurtzke expanded disability status scale.[4] The score indicated her condition as requiring “a walking aid-cane, crutch, etc. To walk about 100 m with or without resting.” Her functional assessment was performed by measuring her ambulatory status[5] and QOL. The measures included the timed up and go for ambulatory status and fatigue severity scale to measure her fatigue levels, one of the major symptom affecting QOL in MS.[6] Balance[7] was tested by Berg balance scale and activities-specific balance confidence scale. Her QOL was evaluated using 29 item MS impact scale.[8] While performing these tests and acknowledging her MS related concerns, certain “triggers” were identified. These included: Her increasing dependence on others for doing her daily chores; minimizing role as a family member; unrelieved psychological, social, and spiritual stress; concerns about dying process in MS; increasing financial stress, depression and/or suicidal ideation; and concerns about advancing symptoms. These concerns led to the evaluation of her palliative care needs through palliative outcome scale MS symptoms.[9]
Interventions
Considering the global requirements of the patient a five-member palliative care team was made which included physiotherapist, psychologist, vocational therapist, a nurse, and a counselor. This protocol was based on previously published literature on MS.[1011] Over the next 12 weeks, the patient and their family was informed of this kind of care. The five-member team assessed the patient and suggested ways to improve physical, emotional, psychological, financial, spiritual, and other problems within the financial constraints of the patient.
Physiotherapeutic intervention
Weeks 1 through 4 consisted of lower extremity stretching exercises, followed by aerobic training completed by static cycling with least resistance. Initially, she limited her cycling time to 8 min based on her fatigue but increased cycling time to 20 min at the end of the 4-week session.
At the end of 4 weeks, she shifted on a treadmill to build her aerobic capacity. Her treadmill walking intensity was progressed using the 20-point rate of perceived exertion (RPE) scale. She was instructed to maintain his RPE between 11 and 13 on the scale.
The intervention was based on recommendations in literature, modified according to the goals of the patient who preferred a treatment emphasis on aerobic conditioning.[12] Given a choice of varied techniques, the patient felt treadmill walking most closely reflected her past interests as a Zumba exerciser.
To reduce muscle fatigue while exercising, eccentric activity approach was adopted. The treadmill was adapted such that the patient was walking on a 3° decline surface. In addition, because she had balance challenges that made walking on a treadmill a little risky activity; hence, a customized body support system[13] was used as a safety device. This was used during the entire training program, and she completed all sessions of the exercise program.
Balance retraining exercises were performed either in seated or standing in a corner with a chair placed in front of her. She was also given two sessions of Tai-chi per week.[14] Emphasis was laid on improving static postural control during vestibular/visual challenges and facilitation of eye or head coordination.[15]
For managing her bladder issues, pelvic floor strengthening exercises were taught.
At the 8th week, a reassessment of her physical abilities was made, and her aerobic and progressive resistance training was redesigned accordingly. The physiotherapy sessions were given for 4 days/week.
Cognitive rehabilitation
The patient expressed about her declining mental abilities and feeling of brain fog; hence, she was tested through standard neuropsychological tests for MS that is symbol digit modality test[16] and Montreal cognitive assessment battery.[17] She underwent two cognitive therapy sessions per week for the duration of 8 weeks. The sessions emphasized on improving her attention span, working memory, and executive functioning.
Vocational therapist
Since the last relapse had affected her vision, hence, the vocational therapist advised her activities considering her physical abilities, her interests, and her visual limitations to undertake Zumba classes for elderlies, as for elderlies she need not use very tiring moves and this will address her financial issues to a certain extent. Moreover, this kind of engagement for 2 days a week will keep her psychosocial issues at bay.
Nurse
A home nurse visit was arranged once per week to address any self-care issues by the patient and the caregivers.
Counseling
Sessions were held every Sunday for 12 weeks.
RESULTS
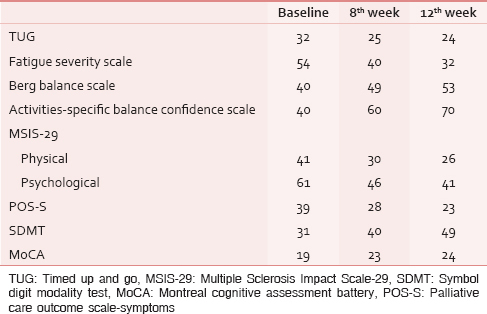
Apart from baseline evaluations, the tests were repeated at the end of 8th week and 12th week. The results of these evaluations are described in Table 1
DISCUSSION
The goal of the interventions was to provide our patient with the training strategies and supports, so as to facilitate a successful transition to independent living given the relatively new physical, medical, and psychological challenges associated with her diagnosis and last relapse of MS.
People with MS often have poor postural control, which makes them more susceptible to falls. Based on several studies of balance and gait in MS, it appears that the principal mechanisms underlying the observed changes are slowed somatosensory conduction and impaired central integration.[18] Hence, balance retraining is an important domain to be managed in MS.
Physical activity results in improved overall QOL and sense of well-being in persons with neurodegenerative disorders like MS.[19] Besides regular medications, physiotherapy is a mainstay to manage motor problems like spasticity in people with MS.[20]
For cognitive rehabilitation, a lot of emphasis was put on cued mental practice or motor imagery of desired physical activities.[21] This type of rehabilitation helps in increasing the spatial accuracy of the imagined movements. Motor imagery is a cognitive process in which a subject is asked to imagine oneself performing a movement without actually performing the movement and without even tensing the muscles. In other words, motor imagery requires the conscious activation of brain areas that are also involved in movement preparation and execution, accompanied by a voluntary inhibition of the actual movement.[22] Motor imagery strategy also plays a vital role in fatigue management in MS patients.[23]
Vocational training in the form of counseling and guidance according to the patients interest was provided. This helped her to choose a resource considering her physical limitations. Such kind of assistance is shown to be positively associated with employment outcomes in MS patients.[24]
While palliative care in MS has some features in common with comprehensive MS care, which most of the physiotherapists working in this sector tend to provide to their patients at the earliest. However, palliative care can be differentiated from traditional MS physiotherapy care by its multifaceted approach, which includes not only traditional disease-symptom management but also improving overall QOL for the patient and the family; managing distressing symptoms; facilitating communication, assisting in decision-making along with advance care planning; and providing opportunities for personal growth throughout the entire disease course. Thus, a physiotherapist can play an important role in becoming a liaison between the patient and other health care providers for optimum patient care.
Furthermore, palliative care can be provided in all care settings (home, outpatient clinic, long-term care facility, hospital, or Intensive Care Unit). Since MS remains an incurable progressive disease, it is often associated with varying presentation of symptoms, disability, and losses of physical, psychological, and social role functioning over time. Hence, it is appropriate to offer a palliative care approach to MS patients and their families whenever their physical, psychosocial, and spiritual needs require such support.[25] Moreover, a home based, patient-centered, and an interdisciplinary approach is more cost effective and tends to provide greater emotional, social, and psychological support to the patient.[26]
Thus, a palliative care approach has much to offer the people in the advanced stages of neurodegenerative diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Available from: http://www.who.int/cancer/palliative/definition/en/
- Symptom prevalence and severity in people severely affected by multiple sclerosis. J Palliat Care. 2006;22:158-65.
- [Google Scholar]
- Palliative care in patients with severe multiple sclerosis: Two case reports and a survey among German MS neurologists. Palliat Med. 2007;21:109-14.
- [Google Scholar]
- Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444-52.
- [Google Scholar]
- Evaluating walking in patients with multiple sclerosis: Which assessment tools are useful in clinical practice? Int J MS Care. 2011;13:4-14.
- [Google Scholar]
- The relationship between fatigue and other clinical features of multiple sclerosis. Mult Scler. 2011;17:604-12.
- [Google Scholar]
- Sensory integration balance training in patients with multiple sclerosis: A randomized, controlled trial. Mult Scler. 2015;21:1453-62.
- [Google Scholar]
- Multiple sclerosis impact scale (MSIS-29): Reliability and validity in hospital based samples. J Neurol Neurosurg Psychiatry. 2002;73:701-4.
- [Google Scholar]
- A psychometric validation of two brief measures to assess palliative need in patients severely affected by multiple sclerosis. J Pain Symptom Manage. 2013;46:406-12.
- [Google Scholar]
- Home-based palliative approach for people with severe multiple sclerosis and their carers: Study protocol for a randomized controlled trial. Trials. 2015;16:184.
- [Google Scholar]
- Palliative care for people severely affected by multiple sclerosis: Evaluation of a novel palliative care service. Mult Scler. 2010;16:627-36.
- [Google Scholar]
- The positive effects of negative work: Increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol A Biol Sci Med Sci. 2003;58:M419-24.
- [Google Scholar]
- Treadmill training in multiple sclerosis: Can body weight support or robot assistance provide added value. A systematic review? Mult Scler Int 2012 2012 Article ID 240274, 15 pages
- [Google Scholar]
- Mental Tai-Chi based exercise programme Vs Tai-chi for Indian multiple sclerosis patients: A pilot study. Int J Curr Res Rev. 2014;6:24-30.
- [Google Scholar]
- Home balance training intervention for people with multiple sclerosis. Int J MS Care. 2007;9:111-7.
- [Google Scholar]
- The symbol digit modalities test as sentinel test for cognitive impairment in multiple sclerosis. Eur J Neurol. 2014;21:1219.
- [Google Scholar]
- Value of the MoCA test as a screening instrument in multiple sclerosis. Can J Neurol Sci. 2013;40:410-5.
- [Google Scholar]
- Postural control in multiple sclerosis: Implications for fall prevention. Curr Neurol Neurosci Rep. 2010;10:407-12.
- [Google Scholar]
- Physical activity and quality of life in multiple sclerosis: Possible roles of social support, self-efficacy and functional limitations. Rehabil Psychol. 2007;52:143-51.
- [Google Scholar]
- Rehabilitation in palliative care: Physiotherapy. In: Doyle D, Hanks GW, MacDonald N, eds. Oxford Textbook of Palliative Medicine. Oxford: Oxford University Press; 1997.
- [Google Scholar]
- Cued motor imagery in patients with multiple sclerosis. Neuroscience. 2012;206:115-21.
- [Google Scholar]
- Treatment of fatigue in multiple sclerosis patients:A neurocognitive approach. Rehabil Res Pract. 2011;2011:670537.
- [Google Scholar]
- State vocational rehabilitation services and employment in multiple sclerosis. Mult Scler. 2013;19:1655-64.
- [Google Scholar]
- Center to Advance Palliative Care. Available from: http://www.capc.org
- Home based management in multiple sclerosis: Results of a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2002;73:250-5.
- [Google Scholar]






