Translate this page into:
Development and Psychometric Assessment of a Spirituality Questionnaire for Indian Palliative Care Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
There are only a few studies on spirituality among palliative care patients in India. This gap in research may be caused by the absence of relevant questionnaires and scales specifically designed for Indian palliative care populations. In this study, we describe the development of such a questionnaire and explain its psychometric characteristics.
Methods:
We designed a questionnaire on the basis of a systematic review of the literature. After a review of the questionnaire by specialists and a subsequent pilot study, the questionnaire was amended. The final questionnaire consisted of a list of 36 spirituality items. It was administered to a sample of 300 cancer patients attending the pain clinic of a tertiary hospital in New Delhi.
Results:
A factor analysis led to four factors explaining 54.6% of variance: Shifting moral and religious values (Factor 1), support from religious relationship (Factor 2), existential blame (Factor 3), and spiritual trust (Factor 4). The skewness and kurtosis for Factors 1, 3, and 4 were within a tolerable range for assuming a normal distribution, but Factor 2 was skewed. The alphas showed that the four factors have an acceptable internal consistency. Statistically significant associations were observed for age and Factor 3 (P = 0.004), gender and Factor 4 (P = 0.014), marital status and Factors 3 (P = 0.002) and 4 (P = 0.001), educational level and Factors 3 (P < 0.001) and 4 (P < 0.001), and pain scores and Factors 1 (P < 0.001), 2 (P < 0.001), and 3 (P = 0.001).
Conclusion:
The questionnaire offers promising prospects for the study of spirituality among palliative care patients in India.
Keywords
Factor analysis
India
Palliative care patients
Psychometric assessment
Questionnaire
INTRODUCTION
In palliative care research and among palliative care providers, a consensus has grown regarding the importance of spirituality. The need to pay attention to palliative care patients’ spiritual needs and concerns is generally recognized. Therefore, it is no surprise that in the World Health Organization (WHO)'s well-known definition of palliative care spirituality is mentioned as one of the main problems that should be addressed by palliative care teams.[1] Also, the Indian Association of Palliative Care has recognized the necessity to address spiritual distress by explicitly mentioning it in its contextualized definition of palliative care.[2]
Given this broad consensus, it is surprising to note that only limited attention has been paid to the study of spirituality in palliative care in India. Among Indian palliative care patients or patients with palliative care needs, spirituality has most often been studied as an aspect or domain of quality of life,[345678] as one of the coping mechanisms used by patients,[910] or as part of psychosocial problems faced by them.[111213] Spirituality has been the main topic in very few empirical studies.[141516171819] The limited attention that has been paid to spirituality in palliative care research in India is even more surprising given the fact that India is a very large country with its own distinctive cultures, social organization, and religions. Therefore, it can be surmised that observations regarding spirituality in palliative care in other countries cannot necessarily be applied to India.
One of the factors that may explain the limited attention to spirituality in Indian palliative care research is the lack of validated research tools or scales regarding spirituality in this setting. There are no spirituality scales specifically designed and validated for the Indian palliative care context. Questionnaires and scales that are developed elsewhere and then validated in Indian palliative care populations may still be helpful. However, given the particularities of the Indian palliative care context, specific questionnaires especially designed for palliative care patients in India can be expected to represent better their spiritual issues and concerns.
With this study, we intended to develop a questionnaire and undertake a psychometric assessment of it. The outcome of the study would be a coherent spirituality questionnaire that could be directly used in future studies, and it would be a reliable starting point for the development of a more condensed spirituality scale for the study of spirituality among palliative care patients in India.
METHODS
Development of the questionnaire
To enable us to design appropriate items for the questionnaire, we undertook a systematic review of the literature following the recommendations of the PRISMA statement.[2021] The review of the literature led to two important observations that guided the development of the questionnaire. First, a distinction was made between three-dimensions of spirituality in Indian palliative care: the relational dimension, the existential dimension, and the values dimension. The review of the literature made clear that these three-dimensions constitute a meaningful way of looking at spirituality in Indian palliative care. We, therefore, decided to use these three-dimensions to construct our questionnaire. The three-dimensions were used as benchmarks to cover comprehensively spirituality in Indian palliative care. We did not hypothesize beforehand that a factor analysis would lead to these three-dimensions, because many of the developed items could potentially load on various dimensions. Also, there was no compelling evidence from the literature that these dimensions were effective distinctive facets of spirituality among patients.
Second, the review showed that belief in the existence of a power, force, principle, dimension or entity that transcends human life and the world plays a very important and decisive role in spirituality in Indian palliative care. This finding stimulated us to focus on this transcending aspect in the development of the questionnaire. By emphasizing this aspect, we would also be able to make a distinction between spirituality and other aspects of health care, such as the physical, ethical, psychological and social. For instance, when a patient expresses his desire for reconciliation with his estranged brother, this could be seen as mainly a social issue, if it is accepted that transcendence is a central aspect of spirituality. When this same patient states that the love he feels for his family is stronger than death, this could be interpreted as an expression of spirituality, because the patient refers to “a power, force, principle, dimension or entity that transcends human life and the world,” that is, a particular kind of love.
As shown by Walter,[22] in many more encompassing interpretations of spirituality the borders of spirituality have become so ill-defined that it becomes virtually impossible to distinguish spirituality from other aspects of healthcare or even science. For a focused empirical study, a more restrictive interpretation may, therefore, be helpful. Since the literature review had shown that belief in the existence of a power, force, principle, dimension, or entity that transcends human life and the world is central in spirituality in Indian palliative care, an interpretation that focuses on transcendence was deemed culturally appropriate.
Using the literature, we developed a set of statements for each of the three spirituality dimensions. This resulted in a list of 28 statements. Participants were able to express their view on these statements through a five-point Likert scale. In the questionnaire that we designed, the spirituality items were preceded by questions soliciting demographic information, including age, gender, marital status, diagnosis, prognosis, educational level, and religious affiliation. Participants were also requested to indicate their experience of pain on a numerical rating pain scale.
In September 2013, the list with items was sent out to an international team of experts with research expertise in palliative care, psychology, (pastoral) theology, and religious studies. With their input, the questionnaire was amended, and spirituality items were altered, deleted, or added. The outcome was a modified list of 37 spirituality items. To the questionnaire, we added a participant information sheet and a participant informed consent form. In the participant information sheet, we explained in an easy-to-understand way the purpose and aims of the study, the interview procedure, confidentiality issues, and expected long-term benefits to palliative care.
In order to facilitate discussion among the scholars who were involved in the preparation of the questionnaire and who had different mother tongues, all documents that we had generated were in English. Since the questionnaire was going to be administered to patients who could be expected to be fluent in Hindi, we had the questionnaire, participant information sheet, and a participant informed consent form translated into Hindi by a professional translator. The investigators checked this translation for accuracy and made changes when the translated text was deemed inaccurate or too difficult to be understood by a substantial number of patients.
When the questionnaire had been finalized, we applied for ethical clearance from the Ethics Committee (Institutional Review Board) of the All India Institute of Medical Sciences (AIIMS, New Delhi) where the study would be conducted. The Ethics Committee granted ethical approval.
In April 2014, the questionnaire was piloted among 30 patients attending the pain clinic of the Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, AIIMS. Two trained interviewers administered the questionnaire. The interviewers were asked to indicate the questions that patients found difficult to understand, and they were to propose changes based on their interactions with the patients during the interviews. As a result, some items were changed, and one spirituality item was dropped because that item turned out to be too abstract to be comprehended by a majority of the patients.
In the demographic section, we decided not to ask the patients to give their diagnosis and prognosis. In Indian healthcare, patients are often not properly informed about their diagnosis and prognosis.[232425] Instead, for the data collection with the final questionnaire the interviewers completed the information on diagnosis and prognosis on the basis of the patient's medical file, to which the patients had granted them access in the informed consent form. Then, the patients were asked to rate their prognosis choosing from the options “I do not know anything about my prognosis,” “Very poor,” “Poor,” “Neither poor, nor good,” “Good,” and “Very good.” They were also asked to tell what they knew about their illness.
The interviewers also observed difficulties when they inquired about the participants’ religious affiliation. In the questionnaire, religion was translated into Hindi with the word dharm. However, the word dharm is a philosophical term that has a broader meaning than just religion, and it can also refer to concepts such as duty, morality, or law of nature. In this way, the term confused several participants. Unfortunately, a substantially better translation for the English term “religion” is not available in Hindi.[26] Therefore, the interviewers were instructed first to inquire about the patient's religion or dharm. In cases that the patient did not mention a general religious tradition, the interviewers were to determine the patient's religious affiliation on the basis of sociocultural characteristics, such as particular first names and surnames that are bound to religious communities.
In the final questionnaire, the number of answer categories in the Likert scale for the spirituality items was reduced. The interviewers had noticed that many participants found it hard to distinguish between strongly agree and agree, and between disagree and strongly disagree. Therefore, we decided to reduce the answer categories to agree, neither agree nor disagree, and disagree. The final 36 spirituality items are shown in Table 1.
Data collection and analysis
From September to December 2014, Hindi-speaking patients, who were 18 years or older and attended the pain clinic of the Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, AIIMS, were requested to participate in the study. We excluded patients who were showing signs of extreme pain, who were visibly too distressed, who had a history of neurological or psychiatric impairment, cognitive dysfunction, or alcohol or substance abuse, and patients who had received treatment with investigational drugs within the last 30 days preceding the interview. Patients who initially agreed received more information about the study, were given the participant information sheet, and were asked to sign the informed consent form. Having done that, the patients were interviewed by one of the two trained interviewers who had previously been involved in the pilot study. On average, patients completed the questionnaire in 10 min. Data collection went on until data of 300 patients had been collected. Subsequently, the collected data were entered into an Excel file.
When all data had been entered into the file, it was imported into IBM SPSS Statistics 22, which was used for the data analysis. A factor analysis was performed with M. Basto's and J.P. Pereira's SPSS R-Menu for Ordinal Factor Analysis, because in SPSS the Pearson's correlation matrix is the only correlation matrix that is available to perform exploratory factor analysis. This is not a suitable correlation matrix when dealing with ordinal Likert-type data.[27] Subsequently, we undertook a descriptive analysis of the factors, and we searched for associations between the factors, demographic variables, and pain scores using relevant statistical tests, that is, Pearson's correlation co-efficient, the Mann–Whitney test, and the Kruskal–Wallis test.
RESULTS
Hundred and fifty-two patients (50.7%) were male, and 148 (49.3%) were female. The mean age was 47.5 (standard deviation 12.4). A large majority of the patients (n = 271, 90.3%) were married at the time of the interview, a few were either unmarried (n = 19, 6.3%) or widowed (n = 9, 3%), and one was divorced (0.3%). More than one in four patients (28%, n = 84) indicated to have had no formal education. 21.3% (n = 64) had studied up to 7th grade (12 years) or less. 23% (n = 69) had studied until 10th grade (16 years). 11.7% (n = 35) had completed intermediate education (18 years). 10.7% (n = 32) had an undergraduate degree, and 5% (n = 15) had completed a postgraduate course. Upon comparison of the two items regarding religious affiliation (cf. supra), 80.3% of the patients (n = 241) were classified as Hindu, 13.7% (n = 41) Muslim, 2.7% (n = 8) Sikh, 1.3% (n = 4) Jain, 1% (n = 3) Christian, and 0.7% (n = 2) Buddhist.
As the survey was undertaken in the out-patient pain clinic of a cancer hospital, all patients were suffering from cancer-related pain. Pain scores varied from one (“no pain”) to 10 (“worst possible pain”) with the mean at 3.22 (standard deviation 2.10). The most common cancers were CA breast (n = 45, 15%), CA lung (n = 26, 8.7%), CA gallbladder (n = 15, 5%) and CA rectum (n = 13, 4.3%). As per the medical files, the prognosis of almost two-thirds of the patients was poor (n = 192, 64%) or very poor (n = 6, 2%). However, when the patients were asked to rate their own prognosis, 40.3% (n = 121) stated that their prognosis was either “Good” or “Very good”, while only 28.4% (n = 85) thought that their prognosis was “Poor” or “Very poor.” 14% (n = 42) believed that their prognosis was “Neither poor, Nor good,” and 16% (n = 48) attested that they did not know anything about their prognosis. When the patients were requested to discuss what they knew about their disease, it turned out that most did not know much about their disease other than that they had some kind of cancer, although a few patients did not even know that much.
For the factor analysis, we used the above mentioned SPSS menu for ordinal factor analysis with the orthogonal varimax rotation. Initial eigenvalues indicated that the first factor explained 26% of variance, the second 14.63%, the third 7.2%, and the fourth 6.8%. The total variance explained by four factors was 54.6%. We opted to retain this four-factor solution because the slope of the curve in the scree plot clearly leveled off after the fourth factor, and this solution yielded a meaningful interpretation that could be theoretically supported.
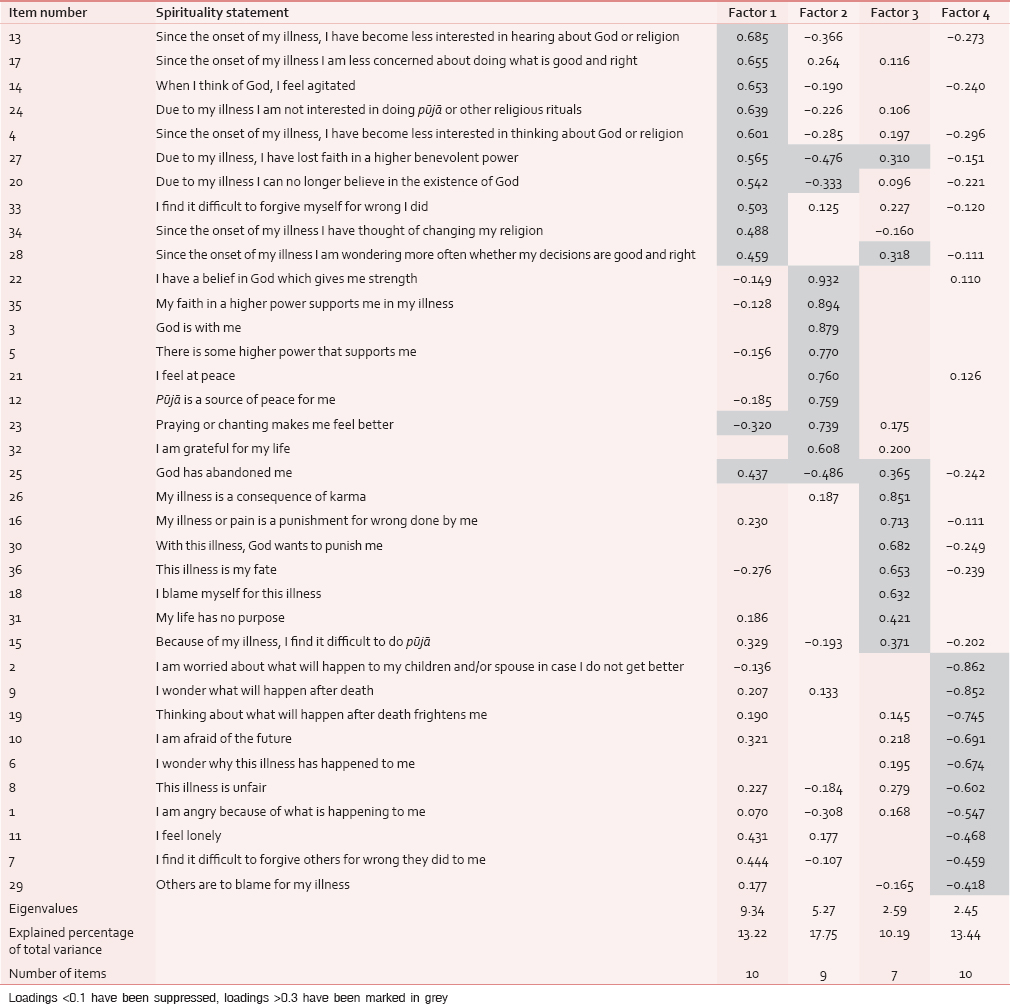
Loadings for the four factors are shown in Table 1. Loadings <0.1 have been suppressed. Loadings >0.3 have been marked in gray.
The factors represent four spiritual demeanors that can be frequently perceived among palliative care patients in India: Shifting moral and religious values (Factor 1), support from religious relationship (Factor 2), existential blame (Factor 3), and spiritual trust (Factor 4). In the names of these factors, the three-dimensions of spirituality that we had used to construct the questionnaire (values dimension, relational dimension, and existential dimension) resurface in a modified form, although during the factor analysis a fourth factor (spiritual trust) appeared.
Items that loaded on the first factor (shifting moral and religious values) showed that values that had earlier been important to patients had become less central since the onset of the illness, or patients at least seriously pondered upon the meaning of these values. There were items that assessed to what extent patients were displeased with their religious views and considered changing their religion or felt agitated when they thought of God. Other items indicated that patients had lost interest in religion. Clearly related to these last items were items that showed loss of faith in God or a higher benevolent power. Last, items showed confusion and concern about which personal acts were good and right.
Items that loaded on the second factor (support from religious relationship) assessed to what extent patients felt supported in their illness by God or a higher power. Besides items that directly inquired about that feeling of support, there were items that assessed whether patients felt better or at peace due to religious activities. Indulgence in such activities can be seen as an expression of a supportive relationship with an ultimate reality.
Items that loaded on the third factor (existential blame) illustrated that patients answered existential questions by blaming themselves for their illness. Relevant items addressed self-blame, belief in karma, belief in illness as a (divine) punishment for sin, and consideration of the illness as personal fate.
In the fourth factor (spiritual trust), the relevant items loaded negatively. Therefore, items that assessed fear and frustration implied trust when they loaded on the fourth factor. Originally, these items inquired about worry and fear about what would happen to themselves or their family in the future or after they had died. The items also assessed the feeling of unfairness: Were others to blame for the illness or had they committed unforgivable sins? Did patients keep wondering why the illness had happened to them? When these items are interpreted reversely, they indicate that patients are at ease with existential answers and feel confident about the future.
After interpreting the four-factor solution, composite scores were created for each of the four factors, based on the mean of the items that had their primary loadings on each factor. Lower scores indicated greater inclination toward the spiritual demeanor. This enabled us to compute descriptive statistics for the four factors [Table 2].

The skewness and kurtosis for factors one, three, and four were within a tolerable range for assuming a normal distribution. However, Factor 2 appeared to be highly skewed toward greater inclination to the demeanor support from religious relationship. The alphas ranged from moderate (0.64 for Factor 3) to good (0.78 for Factor 4), suggesting that the four factors have an acceptable internal consistency.
In a next step, we tested associations between the four factors and demographic variables and pain scores. P < 0.05 was considered statistically significant. For age, there was only significant correlation with Factor 3 (r = −0.67, n = 300, P = 0.004). Higher age was associated with increased existential blame (cf. Graph 1 below).

- Scatter plot with Loess curve for age and Factor 3
A Mann–Whitney test indicated a significant association between gender and Factor 4 (spiritual trust: U[299] = 9283, Z = −2448, P = 0.014). Women showed less spiritual trust (median = 2.33, mean = 2.21, standard deviation = 0.49) than men (median = 2.09, mean = 2.06, and standard deviation = 0.50).
Since the number of patients who were either unmarried, widowed, or divorced was small (n = 29), we decided to treat these patients as one group for marital status, and we checked whether there were differences between these not-married patients on the one hand and married patients on the other hand at the level of the four factors. Mann–Whitney tests showed significant associations between marital status and Factors 3 (existential blame: U[299] =2565.5, Z = −3.106, P = 0.002) and 4 (spiritual trust: U[299] =2420, Z = −3.414, P = 0.001). Married patients showed higher degrees of existential blame (median = 1.47, mean = 1.55, and standard deviation = 0.45) than not-married patients (median = 1.79, mean = 1.85, and standard deviation = 0.51), while patients who were not married scored better, that is, lower scores, for Factor 4 (spiritual trust: Median = 1.84, mean = 1.81, and standard deviation = 0.44) than married patients (median = 2.27, mean = 2.17, and standard deviation = 0.50).
Kruskal–Wallis tests revealed no significant associations for prognosis as rated by patients and the four factors. Also, for religious affiliation there were no significant associations. However, Kruskal–Wallis tests did indicate significant associations between educational level and Factors 3 (existential blame: χ2 = 37.86, df = 5, P < 0.001, with a mean rank factor score of 122.74 for uneducated, 135.43 for less than class 7, 140.26 for until 10th, 186.06 for inter, 202.28 for undergraduate, and 213.97 for postgraduate) and 4 (spiritual trust: χ2 = 32, df = 5, P < 0.001, with a mean rank factor score of 180.34 for uneducated, 158.65 for less than class 7, 152.43 for until 10th, 125.93 for inter, 88.80 for undergraduate, and 118.73 for postgraduate). Table 3 shows that patients who had had less formal education displayed more existential blame (Factor 3) and less existential trust (Factor 4) in comparison to more educated patients.

Pain scores were significantly correlated with Factors 1 (r = −0.24, n = 299, P < 0.001), 2 (r = 0.23, n = 299, P < 0.001), and 3 (r = −0.20, n = 299, P = 0.001). As shown in Graph 2, patients with higher pain scores were more likely to be reconsidering their moral and religious values (Factor 1), derived less support from a religious relationship (Factor 2), and more strongly experienced existential blame (Factor 3).

- Scatter plots with Loess curve for pain and Factors 1-3
DISCUSSION
The present study found four factors representing four spiritual demeanors in Indian palliative care patients. These factors are shifting moral and religious values, support from religious relationship, existential blame, and spiritual trust. The first three factors correspond to the three-dimensions that were used to construct the questionnaire (i.e., values dimension, relational dimension, and existential dimension). The fourth factor, that is, spiritual trust, is a new factor. It includes items probing about fear and worries regarding what will happen to the patients themselves or their families in the future or after their death. It also includes items measuring the feeling of unfairness and injustice, such as: Why did they fall sick? Are the sins committed by patients unforgiveable? Or, who is to blame for this illness: The patients themselves or others? In our study, this fourth-dimension turned out to be an important aspect of spirituality among Indian palliative care patients. Therefore, this dimension should be considered in future research and scale development.
By contrast, the skewness and kurtosis were outside a tolerable range for Factor 2 (support from religious relationship). The observations were skewed toward greater support from religious relationship. This means that virtually without exception Indian palliative care patients derive support from their relationship with the divine or ultimate reality. This corresponds to earlier observations that in Indian palliative care belief in God is almost universal,[11] and most patients are convinced that God will help them overcome their disease.[10] Therefore, in future research the predictive value of the factor support from religious relationship may be limited, and researchers developing more condensed spirituality scales should consider omitting or refocusing it.
Nevertheless, overall, it can be argued that the current study has led to the discovery of significant spirituality factors. This claim can be further supported by referring to the meaningful associations of the factors with demographic variables and pain scores. The present study observed a significant association of increasing age with increasing existential blame. At first, this finding may seem at odds with the observations from earlier studies. Hui et al., noted a signification association of spiritual distress with younger age in a sample of advanced cancer patients admitted to an Acute Palliative Care Unit.[28] Likewise, studies with the WHO Quality of Life (QOL)-HIV instrument showed that spiritual quality of life was better in elderly people than in younger HIV/AIDS patients.[2930] However, there need not be a contradiction between these findings and ours. Although the name of Factor 3 “existential blame” may evoke negative associations, as such the factor does not refer to distress or poor spiritual quality of life. Patients who are more inclined to existential blame were more likely to see their disease as a consequence of karma, punishment for sin, or the result of their own wrongdoing. It can be argued that elderly patients may find such views easier to accept than younger patients, who may be more likely to see their illness as unfair and unjust because they see that most people their age are healthy. So, actually this latter group can be expected to be more prone to existential distress.
Also, the observation that women showed less spiritual trust makes sense when we analyze the items that loaded on Factor 4 (spiritual trust). Several of these items can be related to fear for what will happen to one's children and spouse. Indian palliative care patients have indeed been found to worry about what will happen to their children and partner after their death.[103132] Given the traditional caring roles of women in Indian society, this may be a greater concern for women than men. Indeed, the WHOQOL-HIV Group, which studied quality of life in six countries, including India, reported that females were more fearful of the future and reported poorer spirituality than men.[29]
The fact that the absence of fear for what will happen to their children and spouse constitutes an important aspect of the demeanor of spiritual trust also helps to explain why married patients scored less well on this factor than not-married patients. Married patients have a spouse, and they often also have children for whom they care and worry about. Patients who are not married are thus less likely to have similar worries. Therefore, at first it may seem strange that Marashi et al. did not find an association of the spirituality domain of quality of life with gender and marital status among a sample of HIV-positive patients in India.[33] Their findings can be explained by the fact that they used the WHOQOL-HIV instrument for their study. The concerns about the future that are addressed in that questionnaire have more to do with the respondents’ specific HIV status and seem to exclude anxiety about the future of loved ones.
The association of educational level with Factors 3 (existential blame) and 4 (spiritual trust) may be related to the generally worse socioeconomic condition of the patients with lower levels of education. Since they are economically less well off, they may worry more often about what will happen in the future to their family or who is going to pay the medical bills. Such considerations can have an impact on spiritual trust. Poorer living conditions may lead to a less healthy living environment and substance abuse for which the patients might blame themselves. This, in turn, may result in existential blame.
Also, the association of pain scores with the first three factors lies within the line of expectations and shows the interconnection between physical pain and spirituality. Sometimes, the direction of this association may not be clear. Spirituality may help patients to cope better with pain, and in this way reduce their experience of physical pain. The role of spirituality as a coping mechanism for pain has been well described in the literature.[3435] Yet, at the same time physical symptoms may be so severe that they make patients to question the validity of existential answers, and in this way lead to a spiritual crisis.
To be sure, not all earlier studies on spirituality and physical pain have noted a clear association between the two. In the study of Hui et al., pain was significantly associated with spiritual distress in univariate analysis, although in multivariate analysis this association was no longer significant.[28] Likewise, Mako et al., did not observe a correlation between spiritual pain and physical pain among advanced cancer patients in palliative care.[36]
The contrasting observations regarding the association between physical pain and spirituality may be due to the complexity of the phenomenon spirituality. As a coping mechanism, spirituality can lead to both adaptive or positive coping and maladaptive or negative coping. For example, positive coping entails feelings of divine support, while negative coping can include feeling abandoned by God.[34] Such opposite coping strategies can have a very different impact on the ways in which patients experience their disease and pain. Therefore, while studying spirituality, it is better to look at specific dimensions of spirituality as we did in the current study. Our observations that patients with higher pain scores were more likely to be reconsidering their moral and religious values, felt less supported by a religious relationship, and more strongly experienced existential blame do show that in this population spiritual insecurity and blame are associated with higher levels of physical pain.
Although we have been able to show that we have developed an appropriate questionnaire for the study of spirituality in Indian palliative care, researchers should apply some caution when using the observations in future research, as our study has some limitations. First, the patients were interviewed only when they indicated that their pain was stable. The mean pain score was 3.22 on a scale of 10. However, spirituality in patients with severe pain may vary substantially from those with adequate pain relief. Second, patients were recruited from a single cancer hospital. The external validity of single-center studies is limited. The studied hospital largely caters to the needs of North Indian patients; thus, our observations may not be valid for non-Hindi speaking populations in South India. Moreover, the questionnaire may not lead to equally meaningful results among palliative care patients suffering from diseases other than cancer. Last, in our sample, the number of participants from religious minorities was small. Since religion is an important aspect of spirituality in palliative care in India, the results could have been different if the share of religious minorities in the studied sample had been more substantial.
CONCLUSION
In this study, we have shown that the developed spirituality questionnaire is a good starting point for further studies on spirituality in Indian palliative care. The questionnaire has acceptable psychometric characteristics, and it has revealed four spirituality factors out of which at least three, that is, shifting moral and religious values, existential blame and spiritual trust, deserve elaborate attention in future studies. We recommend that the presented results are used for the development of a brief scale, which can then be tested among larger samples and in more palliative care centers in different parts of India.
Financial support and sponsorship
Joris Gielen is a postdoctoral fellow of the Research Fund – Flanders (FWO). This fellowship enabled him to work on this study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank Anchal Satija and Surajpal Singh, research staff at Dr. B. R. Ambedkar Institute Rotary Cancer Hospital, for administering the questionnaire to the patients and entering the data in the Excel file. They would also like to extend their gratitude to Jordan Potter, graduate assistant at the Center for Healthcare Ethics of Duquesne University, for editing the manuscript
REFERENCES
- WHO definition of palliative care. 2015. Available from: http://www.who.int/cancer/palliative/definition/en/#
- [Google Scholar]
- Psychological well-being among cancer patients receiving radiotherapy – A prospective study. Qual Life Res. 1998;7:495-500.
- [Google Scholar]
- What's important for quality of life to Indians-in relation to cancer. Indian j Palliat Care. 2003;9:62-70.
- [Google Scholar]
- Quality of life and its determinants in people living with human immunodeficiency virus infection in puducherry, India. Indian J Community Med. 2011;36:203-7.
- [Google Scholar]
- Determinants of quality of life in HIV-infected patients receiving highly active antiretroviral treatment at a medical college ART center in Kolkata, India. J Int Assoc Provid AIDS Care. 2013;12:284-90.
- [Google Scholar]
- Psychosocial Determinants of Health-Related Quality of Life of People Living with HIV/AIDS on Antiretroviral Therapy at Udupi District, Southern India. Int J Prev Med. 2014;5:203-9.
- [Google Scholar]
- Quality of life among people living with HIV/AIDS (PLHA) J Psychosoc Res. 2014;9:285-97.
- [Google Scholar]
- Life after cancer in India: Coping with side effects and cancer pain. J Psychosoc Oncol. 2009;27:344-60.
- [Google Scholar]
- Coping mechanisms among long-term survivors of breast and cervical cancers in Mumbai, India. Asian Pac J Cancer Prev. 2005;6:189-94.
- [Google Scholar]
- Psychosocial concerns in patients with advanced cancer: An observational study at regional cancer centre, India. Am J Hosp Palliat Care. 2010;27:316-9.
- [Google Scholar]
- Fighting cancer is half the battle. living life is the other half. J Cancer Res Ther. 2005;1:98-102.
- [Google Scholar]
- Distress screening using distress thermometer in head and neck cancer patients undergoing radiotherapy and evaluation of causal factors predicting occurrence of distress. Indian J Palliat Care. 2013;19:88-92.
- [Google Scholar]
- Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integr Cancer Ther. 2007;6:242-50.
- [Google Scholar]
- Spirituality, distress, depression, anxiety, and quality of life in patients with advanced cancer. Indian J Cancer. 2011;48:55-9.
- [Google Scholar]
- ‘A softening of edges’: A comparison of yoga classes at palliative care services in New Delhi and London. Int J Palliat Nurs. 2010;16:548-54.
- [Google Scholar]
- Spiritual concerns in hindu cancer patients undergoing palliative care: A qualitative study. Indian J Palliat Care. 2013;19:99-105.
- [Google Scholar]
- Exploring the meaning of spiritual care in the Indian context: Findings from a survey and interviews. Prog Palliat Care. 2004;12:221-6.
- [Google Scholar]
- Spiritual well-being and its influence on fatigue in patients undergoing active cancer directed treatment: A correlational study. J Cancer Res Ther. 2014;10:676-80.
- [Google Scholar]
- The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009;151:W65-94.
- [Google Scholar]
- PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264-9.
- [Google Scholar]
- Spirituality in palliative care: Opportunity or burden? Palliat Med. 2002;16:133-9.
- [Google Scholar]
- East meets West: Cross-cultural perspective in end-of-life decision making from Indian and German viewpoints. Med Health Care Philos. 2008;11:165-74.
- [Google Scholar]
- The changing scenario in oncologist-patient communication: We need to adapt. Oncology (Williston Park). 2012;26:48, 54-5.
- [Google Scholar]
- Ethical dilemmas in palliative care in traditional developing societies, with special reference to the Indian setting. J Med Ethics. 2008;34:611-5.
- [Google Scholar]
- God in India. Diversiteit en devotie in de Indische religies. Tielt: LannooCampus; 2013.
- [Google Scholar]
- The frequency and correlates of spiritual distress among patients with advanced cancer admitted to an acute palliative care unit. Am J Hosp Palliat Care. 2011;28:264-70.
- [Google Scholar]
- WHOQOL HIV Group. WHOQOL-HIV for quality of life assessment among people living with HIV and AIDS: Results from the field test. AIDS Care. 2004;16:882-9.
- [Google Scholar]
- Is quality of life poorer for older adults with HIV/AIDS?. International evidence using the WHOQOL-HIV. AIDS Care. 2012;24:1219-25.
- [Google Scholar]
- An exploration of socioeconomic, spiritual, and family support among HIV-positive women in India. J Assoc Nurses AIDS Care. 2004;15:37-46.
- [Google Scholar]
- Breast cancer survivorship and South Asian women: Understanding about the follow-up care plan and perspectives and preferences for information post treatment. Curr Oncol. 2013;20:e63-79.
- [Google Scholar]
- Assessment of quality of life among HIV positive people attending tertiary hospital of Delhi, India. J Commun Dis. 2009;41:101-8.
- [Google Scholar]
- Exploring the relationship between spirituality, coping, and pain. J Behav Med. 2007;30:311-8.
- [Google Scholar]
- Does spirituality as a coping mechanism help or hinder coping with chronic pain? Curr Pain Headache Rep. 2009;13:127-32.
- [Google Scholar]
- Spiritual pain among patients with advanced cancer in palliative care. J Palliat Med. 2006;9:1106-13.
- [Google Scholar]






