Translate this page into:
Myofacial Trigger Points in Advanced Cancer Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Myofascial pain syndrome is started to be recognized as one of important factors of pain in cancer patients. However, no reports on features of myofascial trigger points were found in terminally-ill cancer populations. This time, we encountered 5 patients with myofascial pain syndrome and terminal cancer in whom delirium developed due to increased doses of opioid without a diagnosis of myofascial pain syndrome on initial presentation. The delirium subsided with dose reductions of opioid and treatment of myofascial pain syndrome. The common reason for a delayed diagnosis among the patients included an incomplete palpation of the painful sites, which led to unsuccessful myofascial trigger points identification. The features of myofascial trigger points included single onset in the cancer pain management site with opioid and the contralateral abdominal side muscles of the non-common sites. Withdrawal reflexes associated with cancer pain in the supine position, which are increasingly seen in the terminal cancer patients, were considered to have contributed to this siuation. We consider that careful palpation of the painful site is important, in order to obtain greater knowledge and understanding of the features of myofascial trigger points.
Keywords
Delirium
Myofascial pain syndrome
Palpation
Trigger point
Withdrawal reflex
INTRODUCTION
An improper diagnosis of pain causes inadequate treatment. For example, commonly, opioid analgesics (Op) are effective for cancer pain. However, the pain associated with myofascial pain syndrome (MPS) is one that is unrelated to cancer or cancer treatment directly. Treatment for MPS includes myofascial trigger point (MTP) needling, myofascial release, and stretching exercises.[12] As far as we searched, we did not identify any study reports describing the effectiveness of Op for MPS.
Improper pain management causes a vicious circle of pain. Excessive dosing of Op inconsistent to the severity of cancer pain causes consciousness disorders, including delirium.[3] Op-induced delirium is an exacerbating factor for physical symptoms such as pain.[4] In addition, a previous study has reported that physical interventions to the patients by a physician increase in number with their physical complaints and decrease with psychological or mental complaints.[5] Briefly, Op-induced delirium interferes with detailed physical examinations and makes a proper diagnosis of pain more challenging. Dose reductions, changes in administration route, and switching of Op are recommended in patients with Op-induced delirium.[6] However, these recommendations should not be applied before establishing the complete and proper diagnosis of pain.
We often encounter patients with MPS in the clinical settings. A study has reported that approximately 10% of patients who suffer from pain complain of pain that is unrelated to cancer or cancer treatment directly, especially, myofascial pain.[7] Postmastectomy pain syndrome is one such example. The incidence rate of MPS within 1 year after a mastectomy has been reported to be 44.8%.[8]
It is important to understand the features of MTPs in order to diagnose MPS properly in terminally-ill cancer patients. MPS has a distinctive pathology called MTPs. MTPs are tender spots in palpable taut bands of skeletal muscle fibers.[9] As the underlying pathological mechanisms of MTPs, it is possible that the sensitization of the polymodal receptor causes inflammatory edema because of persistent myotonia and contraction of the skeletal muscle and myofascia.[10] In addition, a role of an overactive sympathetic nervous system in MTP formation has been reported.[11] MPS is started to be recognized as one of the most important causes of pain in cancer patients as well.[12] However, no reports on features of MTPs were found in terminally-ill cancer populations.
This time, we encountered 5 patients with MPS and terminal cancer in whom delirium developed secondary to increased doses of Op and who lacked a diagnosis of MPS at initial presentation. We report these cases here and discuss the common features of MTPs.
SUBJECTS AND METHODS
Materials
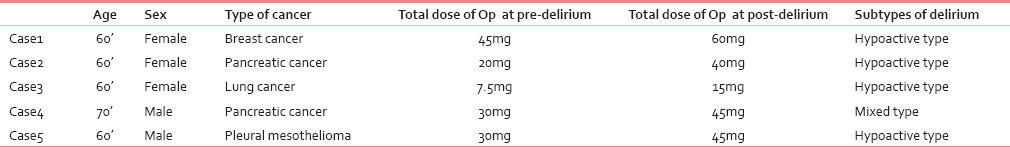
In this paper, we describe 5 patients with terminal cancer, who were referred to the Department of Palliative Medicine in Okayama Saiseikai General Hospital in Japan [Table 1]. All the patients presented with delirium secondary to increased doses of Op without receiving a diagnosis of MPS on initial presentation [Table 1]. The most common reasons for a delayed diagnosis among these patients were the lack of knowledge and an incomplete palpation of the painful sites, which led to unsuccessful MTP identification. All the patients were receiving best supportive care with a performance status of 3 or higher on an inpatient basis. They died at 40.6 ± 25.6 days on average after initial presentation.
Methods
We retrospectively investigated the features of MTPs, sites of pain, cancer pain management sites, sites of MTPs, and single and multiple onsets of MTPs. The diagnosis of MPS is based on the diagnostic criteria defined by Simons et al.[13] [Table 2]. Treatment for MPS included MTP needling; injections to the several local sites with 5–10 mL of 0.1% dibucaine per se ssion, and stretching exercises (passive physical therapy for patients with delirium). We used sharp needles, with a gage of 0.45 mm and a length of 13 mm. Patients were diagnosed as having delirium based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. None of the patients received psychoactive drugs for delirium. The delirium subsided with dose reductions of Op and treatment for MPS. All cases were explored by the two palliative care physicians.

RESULTS
The features of MTPs included single onset in the cancer pain management site treated with Op and the contralateral abdominal muscles of the noncommon sites [Table 3 and Figure 1].


- The sites of myofascial trigger points observed in our patients from top to bottom, ventral deltoid muscle (case 1), ventral intercostal muscle (case 5), ventral serratus anterior muscle (case 3), rectus abdominis muscle (case 2), and ventral external oblique muscle (case 4)
Case 1: A female patient with breast cancer in her 60's
History of present illness
Patient presented with pain on medial aspect of right arm. Palliative radiation therapy to the right scapular and humeral metastatic sites relieved her pain; however, pain relapsed. Increasing doses of oral sustained-release oxycodone were ineffective for pain relief.
Course after initial presentation
On initial presentation, the patient complained of exertional right brachialgia in the abdominal side. Somatalgia secondary to bone metastasis was considered as the cause based on magnetic resonance imaging findings. Increasing doses of oral immediate-release oxycodone led to delirium. On returning to our hospital, palpation of the painful site identified an MTP with a tender spot in the ventral deltoid muscle and referred pain at a distance was identified by palpation of the painful site; therefore, MPS was diagnosed. Delirium resolved with a reduction of the total dose of oral sustained-release oxycodone. The pain was relieved completely as quantified by the patient on a numeric rating scale (NRS) of 0 (ranging from 0 = no pain to 10 = worst pain) after treatment of MPS. She was treated by MTP needling once and passive stretching exercises for 2 weeks.
Case 2: A female patient with pancreatic cancer in her 60's
History of present illness
She presented pain in the upper quadrant pain, and initiation of oral sustained-release oxycodone relieved her pain. However, the upper quadrant pain relapsed. Despite increased doses of oral sustained-release oxycodone, delirium developed.
Course after initial presentation
On initial presentation, the patient complained of no pain because of delirium. Visceral pain secondary to the primary lesion was considered as the cause of pain based on computed tomography (CT) findings. Delirium resolved with additional doses of nonsteroidal anti-inflammatory drugs (NSAIDs) as well as switching from orally administered to injected oxycodone (the dose was lower at an equivalent concentration of Op). However, the patient complained again of right upper quadrant pain. A rescue treatment with oxycodone injections was ineffective. On returning to our hospital, palpation of the painful site identified the MTP as a tender spot in the rectus abdominis muscle and referred pain at a distance; therefore, MPS was diagnosed. Pain relief quantified as NRS 0–3 was achieved after treatment of MPS. She was treated by MTP needling during four consecutive days and passive stretching exercises for several weeks.
Case 3: A female patient with lung cancer in her 60's
History of present illness
Muscle rigidity predominantly on the left side of the body and cognitive impairment were present because of Parkinson's disease. The patient reported left lateral thoracic pain, which was relieved with NSAIDs and oral immediate-release oxycodone. However, pain relapsed.
Course after initial presentation
On initial presentation, pain assessment was not fully completed because of the patient's to cognitive impairment, but we noted that the patient rubbed on the painful left lateral thoracic region on exertion. Somatalgia secondary to pleural infiltration was considered as the cause of pain based on CT findings. Delirium developed after administration of oral sustained-release oxycodone. On returning to our hospital, palpation of the painful site identified the MTPs as a tender spot in the serratus anterior muscle and referred pain at a distance; therefore, MPS was diagnosed. Delirium resolved with a discontinuation of oral sustained-release oxycodone. Pain relief was achieved and quantified as NRS of 0 after undergoing MTP needling twice and passive stretching exercises for 1 week.
Case 4: A male patient with pancreatic cancer in his 70's
History of present illness
Patient presented with left upper back pain. During optimized Ops therapy, among other treatment, contralateral right hypochondrial pain began to develop. Op therapy was replaced with morphine injections, at increasing doses. However, his pain was not relieved, and consequently, delirium developed.
Course after initial presentation
On initial presentation, pain assessment was not fully completed because of delirium, but we noticed that the patient localized pain over right hypochondriac region. Visceral pain secondary to intra-abdominal lymph node metastases was considered as the cause of pain based on CT findings. Liver metastasis was ruled out based on CT findings. The condition remained unchanged even after investigations for delirium with blood tests. On returning to our hospital, palpation of the painful site identified the MTP as a tender spot in the right external oblique muscle and referred pain at a distance; therefore, MPS was diagnosed. Delirium resolved with a reduction of the total dose of morphine injections. Pain relief of an NRS of 0–3 was achieved after treatment of MPS. He was treated by MTP needling twice and passive stretching exercises for several weeks.
Case 5: A male patient with pleural mesothelioma in his 60's
History of present illness
Patient presented with right upper back pain. While pain subsided mainly with oral sustained-release oxycodone, contralateral upper right chest pain began to develop. Increasing doses of oral sustained-release oxycodone failed to relieve his pain.
Course after initial presentation
On initial presentation, the patient reported upper right chest pain. Somatalgia secondary to the primary lesion in the pleura was considered as the cause of pain based on CT findings. Delirium developed after further dose increases of oral sustained-release oxycodone for pain at rest. On returning to our hospital, palpation of the painful site identified an MTP as a tender spot in the 4th intercostal muscle on the mammillary line and referred pain at a distance; therefore, MPS was diagnosed. Delirium resolved with switching from oral to injected oxycodone (the dose was lower at an equivalent concentration of Op). Pain relief was achieved with a level of NRS 0 after treatment of MPS. He was treated by MTP needling once and stretching exercises by him for several weeks.
DISCUSSION
First, regarding common MTP features in our patients, all the patients had underlying cancer pain. Pain from MTPs developed after successful cancer pain treatment with Op. Cancer pain has been previously suggested to be complicated by MPS.[12] We considered that MTPs developed gradually after the unspecified development of cancer pain, and the patients became aware of the pain from the MTPs after successful cancer pain treatment with Op. The locations of the pain were consistent with cancer pain in affected areas or contralateral to the affected areas. Therefore, we improperly diagnosed the condition as an aggravation of cancer pain associated with cancer progression, which led to inadequate pain management, intensifying the successful Op therapy. Thus, Op-induced delirium was caused by these processes.
According to the polymodal theory, the causes of MTP formation in our patients were inflammatory edema and persistent myotonia secondary to a withdrawal reflex associated with cancer pain. A withdrawal reflex is a flexion reflex that evokes defensive responses to noxious stimuli and allows the occurrence of a contraction of the flexors ipsilateral to the stimuli and a relaxation of the extensors[14] One such example includes abdominal wall pain (AWP). The AWP observed commonly in MPS has been previously reported to occur in 11% of patients with abdominal pain of obscure origin.[15] A withdrawal reflex is considered one of MTP formation-causing factors. In addition, in cases 4 and 5, pain developed in the contralateral abdominal side while dorsal cancer pain was being treated with Op. Withdrawal reflexes associated with cancer pain in the supine position, which are increasingly seen in the terminally-ill cancer patients, were considered to have played an important role in these situations. The crossed extensor reflex usually produces a relaxation of the contralateral flexors and a contraction of the extensors to maintain the body in balance. However, regarding Cases 4 and 5, we considered that myotonia persistently occurred in the contralateral medial side because of withdrawal reflexes associated with dorsal side pain because the patients could not bend dorsally in the supine position.
Secondary, common features of MTPs in our patients include single onset in the abdominal muscles of the noncommon sites. In our patients, MTPs were identified in the muscles such as ventral deltoid muscle, rectus abdominis muscle, serratus anterior muscle, external oblique muscle and the ventral intercostal muscle. These muscles are noncommon sites of MTPs; therefore, it is possible to palpate these sites lightly or superficially, leading to an improper diagnosis of pain. The common sites of MTPs include the neck, shoulder, and lower back. A previous study reported that the locations of injection sites during MTP therapy for MPS included the neck and shoulder of 51.3% and lower back of 39.2% of cancer patients.[16] These results show that MTPs are likely to affect the dorsal pressure points and the surrounding areas when in the supine position. Here, the cause of MTPs is considered to be persistent myotonia of the erector spinae muscles (musculus erector spinae) secondary to protracted bed rest time resulting from cancer progression. Based on our hypothesis, the episodes in our patients were attributed to persistent myotonia of the abdominal muscles secondary to withdrawal reflexes associated with cancer pain, and differed in terms of onset sites. For the morphological differences, in general, MTPs develop in multiple muscles comprising the common sites within a beaded appearance. Conversely, in our patients, MTPs only developed in the abdominal muscles in associated with persistent myotonia/withdrawal reflexes.
Given that MTPs identification is indispensable for diagnosing of MPS, a diagnosis with aggressive physical examinations is considered necessary. A previous paper suggested the clinical significance of physical examinations in patients with advanced cancer, in which 83% of the patients showed a positive reaction to the examinations objectively as well as subjectively.[17] This time, we presented our case series with a small population. Therefore, our study results may not be robust enough to characterize the features of MTPs in terminal cancer populations. Nevertheless, we consider that careful palpation of the painful site is important, in order to obtain greater knowledge and understanding of the features of MTPs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Trigger point injections for chronic non-malignant musculoskeletal pain: A systematic review. Pain Med. 2009;10:54-69.
- [Google Scholar]
- Superficial dry needling and active stretching in the treatment of myofascial pain – A randomised controlled trial. Acupunct Med. 2003;21:80-6.
- [Google Scholar]
- Occurrence, causes, and outcome of delirium in patients with advanced cancer: A prospective study. Arch Intern Med. 2000;160:786-94.
- [Google Scholar]
- Effects of intermediate- and long-term use of opioids on cognition in patients with chronic pain. Clin J Pain. 2002;18(4 Suppl):S83-90.
- [Google Scholar]
- Why do primary care physicians propose medical care to patients with medically unexplained symptoms?. A new method of sequence analysis to test theories of patient pressure. Psychosom Med. 2006;68:570-7.
- [Google Scholar]
- A prospective study evaluating the response of patients with unrelieved cancer pain to parenteral opioids. Cancer. 2002;94:3049-56.
- [Google Scholar]
- Pain in cancer patients unrelated to the cancer or treatment. Cancer Invest. 2005;23:84-93.
- [Google Scholar]
- Incidence of myofascial pain syndrome in breast cancer surgery: A prospective study. Clin J Pain. 2010;26:320-5.
- [Google Scholar]
- How do acupuncture and moxibustion act? – Focusing on the progress in Japanese acupuncture research. J Pharmacol Sci. 2006;100:443-59.
- [Google Scholar]
- Phentolamine effect on the spontaneous electrical activity of active loci in a myofascial trigger spot of rabbit skeletal muscle. Arch Phys Med Rehabil. 1998;79:790-4.
- [Google Scholar]
- Injection, neural blockade and implant therapies for pain control. In: Swarm RA, Karanikolas M, Cousins MJ, eds. Oxford Textbook of Palliative Medicine (4th ed). Oxford: Oxford University Press; 2009. p. :734-55.
- [Google Scholar]
- Myofascial Pain and Dysfunction. The Trigger Point Manual. (2nd ed). Lippincott: Williams and Wilkins; 1999. p. :31-5.
- [Google Scholar]
- Functional organization of the nociceptive withdrawal reflexes. I. Activation of hindlimb muscles in the rat. Exp Brain Res. 1990;83:67-78.
- [Google Scholar]
- Long-term follow-up of trigger point injections for abdominal wall pain. Can J Gastroenterol. 2005;19:561-5.
- [Google Scholar]
- Trigger point therapy for myofascial pain in cancer patients (second report) analysis results of special use-results surveillance by neovitacain® injection. Gan To Kagaku Ryoho. 2012;39:605-11.
- [Google Scholar]
- Cancer patients’ perceptions regarding the value of the physical examination: A survey study. Cancer. 2014;120:2215-21.
- [Google Scholar]






