Translate this page into:
Prevalence of Hyponatremia in Palliative Care Patients
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Hyponatremia is an undertreated finding in clinical practice. It is the most common electrolyte abnormality. Hyponatremia can be asymptomatic or can cause symptoms ranging from nausea and lethargy to convulsions and coma. Palliative care patients have a multitude of symptoms and there are several contributing factors towards this. Hyponatremia could be one of the contributing factors. Looking at the prevalence of hyponatremia would highlight the magnitude of the problem and would prompt healthcare professionals to investigate and treat hyponatremia in palliative care patients, which in turn might reduce symptoms such as fatigue and nausea. This could improve the quality of life in palliative care patients.
Aim:
To assess the prevalence of hyponatremia among patients referred for palliative care in a tertiary care hospital.
Methodology:
This is a descriptive study, with retrospective analysis of consecutive patient charts for 5 years. The sodium levels at the time of referral for palliative care, was reviewed. Inferential statistics for the result was calculated using the Z-test.
Results:
Of the 2666 consecutive patient charts that were reviewed, sodium values were recorded in 796 charts. Among the recorded charts, 28.8 % of patients showed hyponatremia at the time of referral which was significant with a P value of 0.000 (<0.05). Of these, 61.1 % had malignancy as their diagnosis and the rest had nonmalignant diseases, ranging from trauma to chronic obstructive pulmonary disease.
Conclusions:
Prevalence of hyponatremia is significant in palliative care patients. A prospective study looking at the causes and clinical outcomes associated with hyponatremia in palliative care patients is needed.
Keywords
Hyponatremia
Palliative care
Prevalence
INTRODUCTION
Hyponatremia is the most common electrolyte abnormality seen in patients.[1] It can be defined as sodium levels below 135 mEq/L. Hyponatremia can be asymptomatic or can cause a variety of symptoms such as nausea, vomiting, malaise, lethargy, confusion, headache, decreased level of consciousness, seizures, and coma, depending on its severity. In their study on hyponatremia in hospitalized cancer patients and its impact on clinical outcomes, Doshi et al. concluded that hyponatremia in a patient with cancer is associated with longer hospital stay and higher mortality.[2] Patients referred for palliative care have multiple symptoms and tiredness or fatigue is one of the most frequent symptoms in palliative care.[3] Hyponatremia can be counted as one of the many contributing factors for fatigue in these patients.
Hyponatremia can be classified, according to volume status, as - hypovolemic hyponatremia: Decrease in total body water with greater decrease in total body sodium, euvolemic hyponatremia: Normal body sodium with increase in total body water, hypervolemic hyponatremia: Increase in total body sodium with greater increase in total body water. Hyponatremia can be further sub-classified according to effective osmolality as hypotonic hyponatremia, isotonic hyponatremia, and hypertonic hyponatremia.
Hypovolemic causes of hyponatremia include acute corticosteroid withdrawal, cerebral salt wasting, diuretic use, gastrointestinal loss, iatrogenic (insufficient volume, use of hypotonic solutions), and skin loss. Normovolemic causes include adrenal insufficiency, drug-induced: Selective serotonin reuptake inhibitors, opioids, and oxytocin. Opioids are a group of drugs that are regularly prescribed for palliative care patients. Hypothyroidism and syndrome of inappropriate secretion of antidiuretic hormone (SIADH) are other important causes of normovolemic hyponatremia. Hypervolemic causes of hyponatremia include acute renal failure, cirrhosis, and congestive heart failure. In cancer patients, which form a majority of palliative care patients, hyponatremia is caused mainly by SIADH and salt wasting. Cancers of the lung, breast, head and neck are the ones commonly associated with hyponatremia caused mostly by SIADH. Among these, lung cancer has the worst prognosis which can be compounded by the increase in mortality caused by hyponatremia.[4]
Establishing the cause of hyponatremia in palliative care patients is often not undertaken as they have multiple co-morbidities and there could be several factors involved. In a developing country like India, financial implication is a major factor that contributes to physician's reluctance in ordering multitude of tests required to establish the exact cause of hyponatremia such as serum osmolality, urine osmolality, and imaging studies. Clinical judgment in requesting appropriate investigations is tested in such circumstances. Correction of hyponatremia becomes difficult when there are multiple causes. A literature search reveals that hyponatremia is prevalent in patients and often is an incidental finding which is undertreated.[5]
METHODOLOGY
A retrospective manual analysis of charts of consecutive patients, who were referred to the Department of Pain and Palliative Medicine, St. John's Medical College Hospital, Bengaluru for a total of 5 years, was carried out. All patients whose sodium levels were below 135 mEq/L were included in the analysis. Inferential statistics for the result was calculated using the Z-test. Statistical package SPSS 16 (IBM SPSS statistics) was used for analysis of data.
RESULTS
Demographics
A total of 2666 charts were analyzed. Sodium levels were documented in 796 charts [Figure 1a]. Hyponatremia was recorded in 222 which is 28.8 % of the patients whose sodium levels were documented. Patients’ age varied from 3 to 94 years, and 125 men and 97 women demonstrated hyponatremia [Figure 1b].
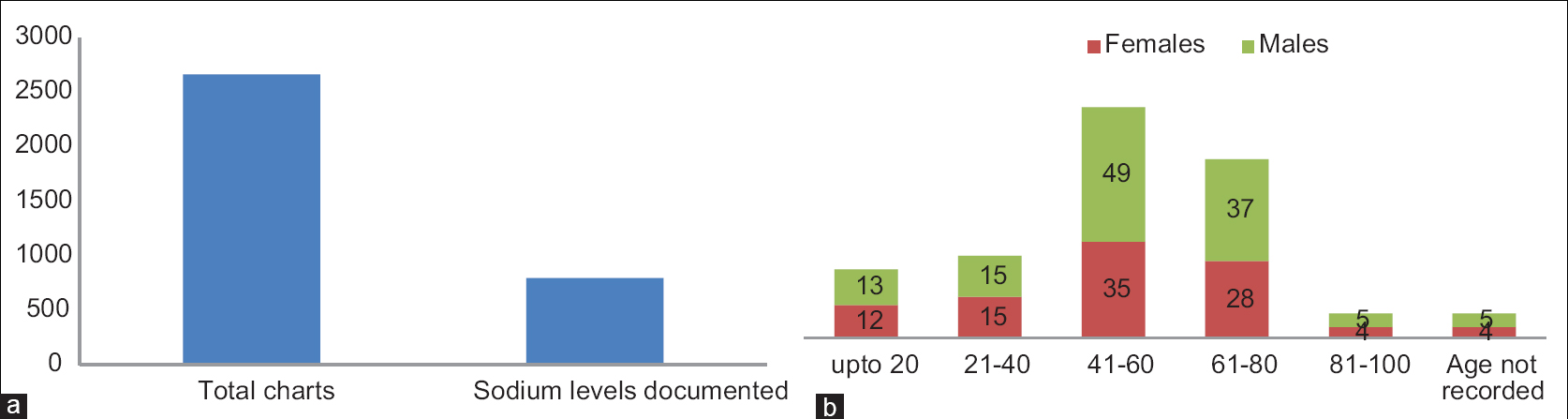
- (a) Documentation of sodium levels, (b) demographics
Prevalence of hyponatremia
Of the 28.8% of patients, who had documented hyponatremia, 61.1 % had malignant disease compared to 39.9 % with nonmalignant disease [Figure 2]. Inferential statistics done with Z-test was statistically significant with a “P” value of 0.000.

- Prevalence of hyponatremia in malignant and nonmalignant diseases
Types of cancers with hyponatremia
In the malignant group, gastrointestinal cancers showed the highest percentage (36.7%), followed by hematological cancers (16.1%), genitourinary cancers (14.7%), lung cancers (12.5%), head and neck cancers (8.8%), breast cancers (5.1%), and endocrine, renal and soft tissue cancers (5.7%) forming the remaining group [Figure 3].

- Types of cancers with hyponatremia
The nonmalignant group of patients had different diseases such as fractures, amputations, stroke, peripheral vascular disease, renal failure, cardiac failure, and chronic obstructive pulmonary disease.
Percentage of patients in different grades of hyponatremia
Of the 222 patients, who had hyponatremia, 117 (52.7%) had mild hyponatremia with a sodium of 130–134 mEq/L, 65 (29.2%) had moderate hyponatremia with a sodium of 125–129 mEq/L, and 40 (19.1%) had severe hyponatremia with a sodium value of 124 mEq/L and less [Figure 4a].

- (a) Grades of hyponatremia, (b) percentage of malignant and nonmalignant diseases in different grades of hyponatremia
Malignant patients formed 88.8% in the mild hyponatremia group, 75.4% in the moderate group, and 82.5 % in the severe hyponatremia group. The nonmalignant patients formed 11.2%, 24.6%, and 17.5 5% in the mild, moderate, and severe hyponatremia group, respectively [Figure 4b].
DISCUSSION
True occurrence of hyponatremia in various clinical settings is difficult to determine. A literature search (Cochrane database and EMBASE) for the prevalence of hyponatremia in palliative care patients did not yield any result. There are several studies that connect hyponatremia to increased hospital stay and increased mortality. This is true, especially with elderly patients.[6] In their study looking at predictors of inpatient mortality in an acute palliative care unit, Elsayem et al. states that hyponatremia is a significant risk factor among others.[7] Correlation of hyponatremia to patient mortality was not done in the present study.
In their study on prevalence, incidence, and etiology of hyponatremia in elderly patients with fragility fractures, Cumming et al., found that hyponatremia was seen in 26% of patients and was highly prevalent. They found that dehydration and prescription of thiazide diuretics and proton pump inhibitors were the potential causative factors and not SIADH.[8] In the present study too, the prevalence of hyponatremia was significant at 28.8% with a P value of 0.000. In another study, Shapiro et al. found that the prevalence of severe hyponatremia in elderly hospitalized person was significant with a P < 0.001. They found that it was more frequent in women and multifactorial in etiology in 50% of the cases. In their group of patients, they found that it is most commonly caused by SIADH.[9] In the present study, more men (125) were found to have hyponatremia compared to women (97). Mohan et al. states that hyponatremia is a predictor of mortality in the general population independently of age, gender, and co-morbid conditions.[10] A study on ambulatory patients with mild hyponatremia followed up over a period of 8 years, found that the prevalence was 6.9% and was significantly associated with age, black ethnicity, presence of cirrhosis, cardiac failure or cancer and use of antiepileptic drugs and serotonin reuptake inhibitors.[11] In the present study, 61.10% of patients with malignant diseases and 39.9% of patients with nonmalignant diseases were found to have hyponatremia. In a study that looked at hyponatremia in acute medical admissions, the authors found that the prevalence of hyponatremia was high.[12] This could indicate that hyponatremia might be a cause of acute admissions.
In another study that looked at diagnostic codification of hyponatremia on patients admitted under Internal Medicine, the authors found that there was a low prevalence of hyponatremia codification and stated that hyponatremia was underreported and undertreated in spite of numerous studies showing devastating effects of hyponatremia.[13] Cancer patients form the majority of palliative care patients and cancer in itself and its different manifestations cause hyponatremia. An aging population also has more prevalence of cancer, thereby increasingly seeking palliative care. Hyponatremia can be found associated with SIADH in 10–15% of patients with small cell lung cancer.[141516] In their article on tumor related hyponatremia, Onitilo et al. states that hyponatremia is a serious comorbidity in cancer patients and require special attention.[17] Hyponatremia may be detected by routine laboratory testing or by the manifestation of neurological symptoms in cancer patients. Appropriate diagnosis is important as treatment differs.[18] Hospitalized cancer patients are prone to have a higher rate of hyponatremia when compared to hospitalized noncancer patients with the outcome in the cancer patients being poor.[19] In a study result from the International Metastatic Renal Cell Cancer Database Consortium, hyponatremia was found to be independently associated with a worse outcome in metastatic renal cell cancer patients.[20] Most of the patients referred for palliative care in the present study population were cancer patients.
Worldwide, cancer patients still form the majority of palliative care patients. With an already bad prognosis, it is tough for patients to bear the added burden of hyponatremia and its complications. It is time that we recognized and treated hyponatremia diligently so that the patients and their relatives suffer less from the added burden. Even today the disorder largely remains underdiagnosed.[21] Substantial amount of work needs to be done to assess the causes and management outcomes of hyponatremia in palliative care patients.
CONCLUSION
Prevalence of hyponatremia is significant in palliative care patients. Although this study showed that hyponatremia is more in cancer patients, it cannot be generalized, as the number of cancer patients included in the study was proportionately more than noncancer patients. The causes and clinical outcomes associated with hyponatremia in palliative care patients warrant analysis of a prospective cohort.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hyponatremia in hospitalized cancer patients and its impact on clinical outcomes. Am J Kidney Dis. 2012;59:222-8.
- [Google Scholar]
- Fatigue in palliative care patients – An EAPC approach. Palliat Med. 2008;22:13-32.
- [Google Scholar]
- Hyponatremia of non-small cell lung cancer: Indian experience. Indian J Med Paediatr Oncol. 2011;32:139-42.
- [Google Scholar]
- Recurrent hospitalizations with moderate to severe hyponatremia in older adults and its associated mortality. Eur J Intern Med. 2014;25:624-8.
- [Google Scholar]
- Predictors of inpatient mortality in an acute palliative care unit at a comprehensive cancer center. Support Care Cancer. 2010;18:67-76.
- [Google Scholar]
- Prevalence, incidence and etiology of hyponatremia in elderly patients with fragility fractures. PLoS One. 2014;9:e88272.
- [Google Scholar]
- Severe hyponatraemia in elderly hospitalized patients: Prevalence, aetiology and outcome. Intern Med J. 2010;40:574-80.
- [Google Scholar]
- Prevalence of hyponatremia and association with mortality: Results from NHANES. Am J Med. 2013;126:1127-37.
- [Google Scholar]
- Mild hyponatremia is associated with an increased risk of death in an ambulatory setting. Kidney Int. 2013;83:700-6.
- [Google Scholar]
- Prevalence of hyponatremia in acute medical admissions in tropical Asia Pacific Australia. Asian Pac J Trop Med. 2014;7:40-3.
- [Google Scholar]
- Low prevalence of hyponatremia codification in Departments of Internal Medicine and its prognostic implications. Curr Med Res Opin. 2013;29:1757-62.
- [Google Scholar]
- Is hyponatremia a prognostic marker of survival for lung cancer? Pneumologie. 2011;65:565-71.
- [Google Scholar]
- The occurrence of hyponatremia in SCLC and the influence on prognosis: A retrospective study of 453 patients treated in a single institution in a 10-year period. Lung Cancer. 2010;68:111-4.
- [Google Scholar]
- High sensitivity to tolvaptan in paraneoplastic syndrome of inappropriate ADH secretion (SIADH) Ann Oncol. 2011;22:2696.
- [Google Scholar]
- Diagnosis and management of hyponatremia in cancer patients. Oncologist. 2012;17:756-65.
- [Google Scholar]
- Tolvaptan in hospitalized cancer patients with hyponatremia: A double-blind, randomized, placebo-controlled clinical trial on efficacy and safety. Cancer. 2014;120:744-51.
- [Google Scholar]
- The impact of low serum sodium on treatment outcome of targeted therapy in metastatic renal cell carcinoma: Results from the International Metastatic Renal Cell Cancer Database Consortium. Eur Urol. 2014;65:723-30.
- [Google Scholar]






