Translate this page into:
Symptoms experienced by cancer patients and barriers to symptom management
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
People living with cancer experience wide variety of symptoms. If symptoms are not managed well, it may hamper an individual's ability to continue his or her activities of daily life. Treatment of symptoms relieves suffering and improves the rate of recovery as well as the quality of life.
Objectives:
To assess the symptoms of suffering among cancer patients and to identify the perceived barriers to their symptom management.
Materials and Methods:
A cross-sectional study was carried out among 768 cancer patients selected by stratified sampling with a proportionate selection from each stratum. Data were collected from cancer patients by interview technique using structured validated questionnaire.
Results:
Majority of the samples (30.2%) belonged to the age group of 51–60 years, most of them were diagnosed with head and neck cancer (40.1%) and 57.7% had stage III disease. The majority of the patients studied had pain (77%), tiredness (96.5%), disturbed sleep (96.4%), weight loss (63.3%), and irritability (85.7%). Most of the patients had lack of appetite (89.4%), feeling of sadness (96.6%), worry (94.5%), and feeling of nervousness (82.8%). Majority of the patients had some misconception regarding symptoms, that is, increasing pain signifies disease progression (92.7%), medicine to control pain may weaken the immune system (89.9%) and pain is inevitable for cancer patients (78.5%). Seventy-seven percent of samples reported that the anxiety or depression is expected after the diagnosis of cancer.
Conclusion:
This study provides an overview of symptoms among cancer patients and barriers experienced by them.
Keywords
Barriers
Cancer patients
Symptoms
INTRODUCTION
People living with cancer experience a variety of symptoms-such as pain, worry, depression, diarrhea, cough, shortness of breath, nausea, weakness, fatigue, fever, and confusion. Lack of care results in untreated symptoms that hamper an individual's ability to continue his or her activities of daily living. Treatment of symptoms relieves suffering and often improves the rate of recovery and quality of life. Ward and Gatwood(US) identified barriers like fear of addiction, beliefs that “good” patients do not complain about pain, and concerns about side effects[1] Borneman et al. (UK) classified barriers into three categories: Patient, professional, and system barriers.[2] Pnina has reported three types of barriers to manage pain; those were an addiction to medication, saving pain medicine to use when the pain gets worse, and pain is a sign that the disease was getting worse.[3] Yeom and Heidrich(2009, USA) identified three possible barriers to symptom management; they were: Negative beliefs about managing symptoms, perceived negative attitudes of healthcare providers, and difficulties in communicating about symptoms. Barriers to symptom management may lead to poorer self-care of symptoms that can result in lower levels of psychosocial quality of life.[4]
Objectives of the study
Objectives of the study were to:
-
Assess the symptoms among cancer patients
-
Identify the perceived barriers to symptom management among cancer patients
-
Find the association between perceived barriers and study variables of client such as age, education, income, type of cancer, stage of cancer, duration of illness, and treatment.
Sample size estimation
One of the main objectives was to estimate the barriers perceived by the cancer patients. The sample size for this study was calculated based on the pilot study result. For 95% confidence limits, the allowable error of 1.5% and a design effect of 2 for cluster sampling, a sample size of 768 would be sufficient to estimate the rate at 5% level of significance.
Formula used for the calculation of sample size was:

N = Sample size
Zα = 95%
σ = 7.8 (Barrier score)
d = 1.5%
Total = 384. 384 × 2 = 768
MATERIALS AND METHODS
An exploratory survey was done among 768 cancer inpatients aged above 30 years and diagnosed to be in third or above stages of cancer of breast/cervix/head and neck/gastro intestinal tract/lung/colorectal cancer and have undergone radiotherapy or chemotherapy or surgery or combination of them in selected reputed cancer hospitals of Karnataka. Patients unable to perform activities and with psychiatric problems were excluded from the study. Reputed cancer hospitals all over Karnataka were selected by purposive sampling, and each hospital was considered as a stratum. Then proportionate sample from each stratum was selected for the study. Data were collected from cancer patients of various hospitals using pre-tested structured interview technique after obtaining permission from the respective hospital administrators. Cancer patients those who have given their consent only were interviewed for the study.
Ethical issues
Reputed cancer hospitals were selected, and permission was obtained from the respective administrators. The hospitals who granted permission to do the study only were included. The objective and study protocol were explained to the study participants, and written consent was taken.
Analysis of data
The obtained data were entered in SPSS version 16.0. Data analysis was performed by using descriptive and inferential statistics.
RESULTS
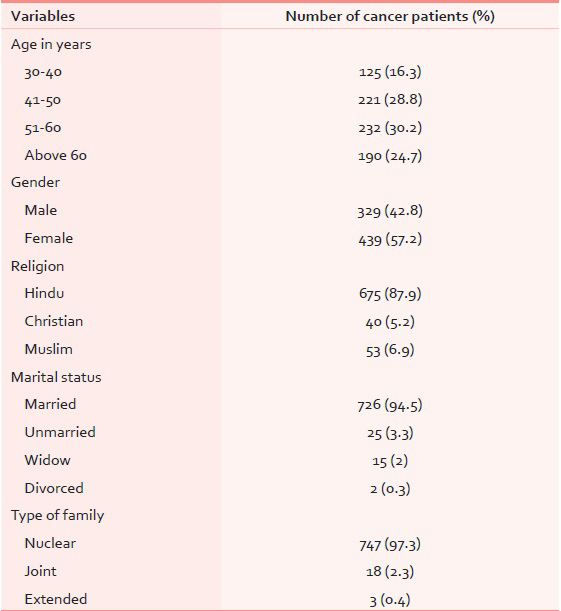
The data from 768 samples were collected and analyzed based on the objectives of the study. Out of 768, majority of the cancer patients (30.2%) belonged to the age group of 51–60 years, most of them were females (57.2%), belonged to Hindu religion (87.9%) and 94.5% were married [Table 1]. The majority of the cancer patients (39.2%) were primary educated [Figure 1]. Most of the affected patients were housewives (49%), their monthly income was between Rs. 2501 and 5000 (51.3%), and 33.1% of the patients had taken combination therapy [Table 2]. Most of them availed modern medical treatment from the hospital after final diagnosis (80.3%) and 57.7% of the samples were in the third stage of cancer [Table 3]. Around 40% of the patients suffered with head and neck cancer and most (76.2%) of the patients were suffering from the illness for <6 months [Figures 2 and 3].

- Educational status of cancer patients



- Types of cancers. GIT: Gastro intestinal tract

- Duration of illness among cancer patients
Self-reported symptoms of suffering
During survey, patients reported various symptoms. Major symptoms are depicted in Figure 4. Majority of the patients (96.5%) had tiredness, 96.4% had disturbed sleep, 94.5% had worry, 90.4% of the patients reported that they lost their appetite after diagnosis, 85.7% patients felt irritable, 83% of patients had feeling of nervousness, 77% had pain and 63.3% of the patients lost their weight after diagnosis, 60.7% had anxiety and 57.6% had depression.

- Self-reported symptoms
Perceived barriers to symptom management among cancer patients
The barriers were categorized into: Communication, personal, professional, financial and misconceptional barriers. The response for all items are graded on a four-point scale (4 = “very much,” 3 = “quite a bit,” 2 = somewhat, 1 = “a little,” and 0 = “not at all“). Major barriers only are shown in the Tables 4–6. Majority of the patients (36.1%) did not know how to express symptoms since the majority had only primary education, they were facing language problems while communicating with the health care personnel (45.8%). 71.4% had worry about side-effects, and 23.1% had fear about addiction. 90.6% had a fear of consequences of treatment, and 96.9% had fear about disease progression. Most (58.8%) of the patients had a fear of further hospitalization, and there were no professional barriers identified except overcrowding in the cancer clinic (50%) [Table 4]. About 89.3% had lack of resources in the family, 99% of the samples expressed that the treatment is very expensive, 72% of samples were not able to afford nutritional supplements, 82.6% of them reported inability to afford the cost of medicine and to pay for health care services (83.1%) [Table 5]. Majority of the samples had some misconception that is, increasing pain signifies disease in progress (92.7%), medicine to control pain may weaken the immune system (89.9%), pain is inevitable for cancer patients (78.5%), and 77.1% of samples reported that the anxiety or depression are expected after diagnosis of cancer [Table 6].



Data further showed that for total barriers score among cancer patients from all categories, the mean was 44.86 and standard deviation 19.38 [Table 7]. Median and interquartile range of each type of barriers identified among cancer patients are presented in Table 8. Financial barriers were affecting symptom management the most among the cancer patients. Central 50% of the samples have a value of 12–24.


Association between mean score of barriers and study variables
One-way ANOVA test was used to test the association between the mean score of barriers perceived by the cancer patients and study variables such as age, gender, education, income, type and duration of illness. Result showed that as education and income increases, barriers score decreases, which is found to be statistically significant (education: F = 13.556, P= 0.001 and income: F = 16.338, P= 0.001) [Table 9].

DISCUSSION
The study findings were in conformity with a study done by Naveh et al.[3] who reported that 66% of the patients had severe pain and Iyer et al. who found that more than 90% of the patients expressed pain, fatigue and loss of appetite. Fatigue, loss of appetite, shortness of breath and pain have a significant negative impact on patient reported disease specific health related quality of life in advanced non-small-cell lung cancer patients.[5] Nilmana et al.[6] and Harding et al.[7] reported in their study that most of the cancer patients had pain (87.5%), lack of energy (77.7%), feeling sad (75.9%), feeling of drowsiness (72.3%) and worry (69.6%). Yates et al.[8] reported some of the symptoms experienced by patients in their study: 48% of cancer patients had pain within the previous 24 h and they were depressed (41.8%), worried (38.2%), frightened (30.9%) and angry (18.2%) due to disease-related symptoms.
The present study showed that barriers to symptoms management were: Worry about side effect (71.4%), fear of addiction (23.1%) and pain medication harm the immune system (89.0%). Similar findings on barriers were observed by Nilmana et al.,[6] Edrington et al.[9] and Ward et al.[10] in their studies; which were: Concern about medication and its side-effects, fear of addiction and beliefs that “good” patients do not complain about pain and disease progression. Gunnarsdottir et al.[11] found that pain medications harm the immune system and Yates et al. reported that almost 71% believed it is easy to become addicted to pain relieving medication.[8]
Limitations
-
Since this study was confined to a single state, the findings cannot be generalized to nationwide
-
Cancer patients who gave consent for participation only were interviewed
-
Permitted hospitals only were selected for the study.
CONCLUSION
This study revealed that cancer patients experience many symptoms and barriers to symptom management. The management of cancer pain is a critical issue in the care of patients with cancer. All health professionals must ensure that patients receive timely and appropriate education and care. There is a need to develop measures for effective management of symptoms and to reduce the barriers.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Concerns about reporting pain and using analgesics. A comparison of persons with and without cancer. Cancer Nurs. 1994;17:200-6.
- [Google Scholar]
- Reducing patient barriers to pain and fatigue management. J Pain Symptom Manage. 2010;39:486-501.
- [Google Scholar]
- Pain severity, satisfaction with pain management, and patient-related barriers to pain management in patients with cancer in Israel. Oncol Nurs Forum. 2011;38:E305-13.
- [Google Scholar]
- Effect of perceived barriers to symptom management on quality of life in older breast cancer survivors. Cancer Nurs. 2009;32:309-16.
- [Google Scholar]
- Symptom burden and quality of life in advanced non-small cell lung cancer patients in France and Germany. Lung Cancer. 2013;81:288-93.
- [Google Scholar]
- Symptom management and its barriers among patients with terminal advanced cancer in Thailand. BMJ Support Palliat Care (Suppl 1) A49 doi:10.1136/bmjspcare-2012-000196.142
- [Google Scholar]
- The prevalence and burden of symptoms amongst cancer patients attending palliative care in two African countries. Eur J Cancer. 2011;47:51-6.
- [Google Scholar]
- Barriers to effective cancer pain management: A survey of hospitalized cancer patients in Australia. J Pain Symptom Manage. 2002;23:393-405.
- [Google Scholar]
- Barriers to pain management in a community sample of Chinese American patients with cancer. J Pain Symptom Manage. 2009;37:665-75.
- [Google Scholar]
- Patient-related barriers to pain management: The Barriers Questionnaire II (BQ-II) Pain. 2002;99:385-96.
- [Google Scholar]






