Translate this page into:
Metastatic Adenocarcinoma of Prostate in a 28-Year-Old Male: The outcome is poor in young patients?
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Prostate cancer is common in older patients. Rarity in younger population limits the study of natural history and prognosis in this population. Most of the published data has reported poor outcome in younger patients with metastatic prostate cancer. Here, we report a case of prostate cancer in 28-year-old male who presented with bone metastasis. After bilateral inguinal orchidectomy, he was started on anti-androgen therapy and received palliative radiotherapy for bone metastasis. There was only a slight decrease in prostate-specific antigen (PSA) level and pelvic disease post treatment. Subsequently, he was started on opioid analgesics (by World Health Organization, WHO, step ladder) in view of persistent pain. The index case is being presented for its rarity and probable poor outcome in young patients and to stress on the fact that the possibility of primary prostatic adenocarcinoma should be investigated in a male presenting with bone metastasis irrespective of the age.
Keywords
Biological behavior
Carcinoma prostate
Outcome
Young age
INTRODUCTION
Prostate cancer is rare in young adults. Its incidence is 0.8–1.1% in patients younger than 50 years.[1] Causes associated with the onset of the disease in young patients remains elusive. However, genetic factors contribute in around 8–10% of the cases. Other factors which may be associated prostate cancer in young males are abnormality on hereditary prostate cancer 1 (HPC1) gene, race (more common in African American), smoking, fat rich diet, obesity and family history of prostate cancer. [2] It has been reported by Carter et al., that 43% patients of prostate cancer under 55 years of age are hereditary.[3]
Age is an important prognostic factors and biological behavior is thought to be aggressive in younger patients. The Surveillance, Epidemiology, and End Results (SEER) database in 1989–2003 has shown that the prognosis of young men with prostate cancer is worse than that of elderly men as most young patients present with distant metastases and have poorly differentiated or undifferentiated histology.[2] We, here, are reporting a case of prostate cancer in a 28-year-old male who presented with bone metastases.
CASE REPORT
A 28-year-old male presented with complaints of dysuria and backache from past 6 months. Patient had a good general condition and his eastern cooperative oncology group (ECOG) performance status was one. Digital rectal examination revealed large and asymmetrical prostate along with a separate hard nodule. His serum prostate-specific antigen (PSA) level was 5.85 ng/ml (range 0–4 ng/ml). Contrast enhanced magnetic resonance imaging (CEMRI) of pelvis was revealing multi-lobulated enlarged prostate and a large tumor with extra-capsular extension to bilateral seminal vesicles and bladder neck along with multiple enlarged pelvic lymph nodes. Biopsy of the tumor was suggestive of a poorly differentiated prostatic adenocarcinoma with a gleasons score of 4 + 5 = 9. The tumor cells were immunopositive for pancytokeratin, PSA and focally positive for alpha-methylacyl-CoA racemase (AMACR) and synaptophysin while immunonegative for CK 7 and 20, TTF-1, MIC-2, myogenin, and chromogranin. [Figure 1 (a-d) Poorly differentiated adenocarcinoma of prostate with neuroendocrine differentiation. Sections show a malignant tumor arranged in sheets and in vague glandular pattern along with perineural invasion (Figure A; 200×). Immunostains for pancytokeratin (Figure B; 200×), synaptophysin (Figure C; 200×), and PSA (Figure D; 200×) are positive. Whole body Technitium-99 bone scan was suggestive of metastases to skull, right 6th rib, scapula, 11th and 12th thoracic, and 2nd lumbar vertebrae. He was planned for palliative treatment in view of metastatic disease. He underwent bilateral inguinal orchidectomy and started on oral anti-androgen therapy (ADT). Subsequently, he received palliative radiotherapy to painful bone metastasis. He was started on opioid analgesics (by World Health Organization, WHO, step ladder) in view of persistant pain. His serum PSA level was 4.11 ng/ml after 1 year and persistent pelvic disease was seen on CEMRI of pelvis which was repeated after 1 year of treatment.
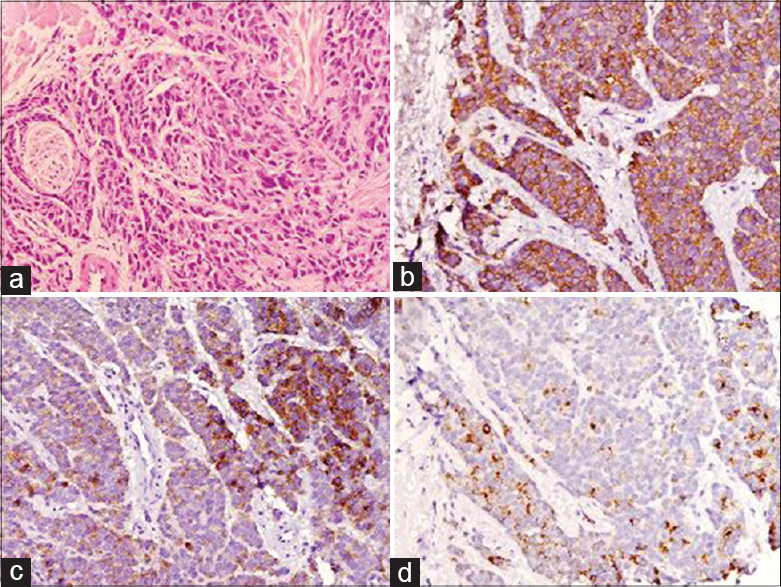
- Poorly differentiated adenocarcinoma of prostate with neuroendocrine differentiation. Sections show a malignant tumor arranged in sheets and in vague glandular pattern along with perineural invasion (Figure A; 200×). Immunostains for Pancytokeratin (Figure B; 200×), Synaptophysin (Figure C; 200×) and Prostate specific antigen (Figure D; 200×) are positive]
DISCUSSION
Biological behavior of prostate cancer is difficult to interpret in young patients because most of these cases are either reported as case reports or are included in the case series of older men. Because of its rarity, there is no standard guideline for management of prostate cancer in young patients and thus it is treated in the same way as in older patients. Number of studies have reported that age is an independent prognostic factor for metatstic prostate cancer and young age is associated with poor outcome. Many of these have been reported in the pre-serum PSA era, so patients used to present in more advanced stage and thus poorer outcome.[4] Although most of the studies have reported poor outcome in younger population, many have suggested equal or even better outcome in this group of patients.
Silber and McGavran observed favorable survival rates in men younger than 50 years.[5] Similar findings have been observed by Bechis et al., that older men are more likely to have high risk prostate cancer and low overall survival because older patients more likely to be treated with primary ADT rather than potentially curative local therapy.[6] A retrospective review of 151 patients under 50 years has shown that young patients have similar morphology and outcome as older patients. Patients received different modes of treatment as surgery, radiotherapy, and endocrine therapy depending upon the stage of disease and availability of treatment at that time. It was suggested that young patients with prostate cancer present with similar symptomatology, histological grade, stage, and prognosis as the older population.[7]
In contrast, several authors have reported poor prognosis in young patients with prostate cancer. In 1980, Hiroyuki shimada et al., reported prostate cancer in a young boy of 11 years age and summarized the clinico-pathologic characteristics of prostatic carcinoma in infant and adolescents. It was thought that aggressive behavior of prostate cancer in young individuals can be because of undifferentiated histology.[8] In another retrospective analysis by Astigueta et al., 41 patients of prostate cancer under 50 year of age were identified from 1952–2005.[2] All patients had bone metastasis. In addition, 20 patients had retroperitoneal metastasis, 3 patients had mediastinal lymph node metastasis, 4 had liver, 3 had lung, and 1 patient had testicular metastasis. All prostatic biopsies were reported as poorly differentiated or undifferentiated and according to current classification, predominant gleason score was 9. Patients received different kind of palliative treatment like bilateral orchidectomy and adrenalectomy in 1970s and oral or parentral ADT in recent years. Additionally patients received palliative radiotherapy and other symptomatic treatment. Median survival was 16.1 month and all patients died of progressive disease.
A recent study by Kimura et al., has also reported poorer outcome in young patients.[9] In this study, 3,006 patients with metastatic prostate cancer received primary ADT. It was seen that age was an independent prognostic factor for metastatic cancer patients and 5 year overall survival was poorer in young patients, at just 22% in patients under 50 years.
To conclude, prostate cancer is rare in young males. The index case explains that in a young male presenting with bone metastasis, possibility of prostate cancer cannot be ruled out. It has been observed from available published data that undifferentiated or poorly differentiated adenocarcinoma is the most common histology in younger age-group and a large percentage of patients present with metastatic disease at the outset. Although many authors have reported poor outcome in young patients, there is still conflicting data regarding its biological behavior and treatment outcome. Future research is required to know the biological behavior and outcome in young patients with prostate cancer.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Atypical case of metastatic undifferentiated prostate carcinoma in a 36 years old man: Clinical report and literature review. Clin Ter. 2000;151:371-4.
- [Google Scholar]
- Characteristics of metastatic prostate cancer occurring in patients under 50 years of age. Actas Urol Esp. 2010;34:327-32.
- [Google Scholar]
- Mendelian inheritance of familial prostate cancer. Proc Natl Acad Sci U S A. 1992;89:3367-71.
- [Google Scholar]
- Adenocarcinoma of the prostate in men less than 56 years old: A study of 65 cases. J Urol. 1971;105:283-5.
- [Google Scholar]
- Impact of age at diagnosis on prostate cancer treatment and survival. J Clin Oncol. 2011;29:235-41.
- [Google Scholar]
- Prostate adenocarcinoma in men younger than 50 years. A retrospective review of 151 patients. Cancer. 1994;74:1768-77.
- [Google Scholar]
- Carcinoma of the prostate in childhood and adolescence: Report of a case and review of the literature. Cancer. 1980;46:2534-42.
- [Google Scholar]
- Prognostic impact of young age on stage IV prostate cancer treated with primary androgen deprivation therapy. Int J Urol. 2014;21:578-83.
- [Google Scholar]






