Translate this page into:
Impact of Medical Intervention on Stress and Quality of Life in Patients with Cancer
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Many studies have explored stress and quality of life in (QOL) patients with cancer, under several phases of disease and treatment. However, the impact of medical intervention on psychological parameters, such as stress and quality of life focusing on psychological intervention has been sparsely studied.
Aims:
The main aim of the study was to examine the impact of medical intervention on the level of stress and quality of life of patients with lung, breast, and head and neck cancers.
Settings and Design:
The study was carried out in hospital settings by following a one-group pre-test-post-test pre-experimental design.
Statistical analysis used:
The quantitative data were analysed by means of descriptive statistics, paired t-tests, Cohen's d, and bar graphs accordingly.
Results:
The effect of medical intervention was medium in case of reduction of overall stress in participants. So far as the components are concerned, the effect was high in case of psychosomatic complaints, medium in case of fear and information deficit, and low in case of everyday life restrictions. The effect of medical intervention in respect of the quality of life was found to be high in case of symptom scale (pain) and additional symptoms (constipation); medium in case of functional scale (emotional functioning, cognitive functioning) and symptoms scale (nausea, vomiting). In additional symptoms scale the effect of medical intervention was found to be medium in dyspnoea and appetite loss.
Conclusions:
The findings revealed that though the medical intervention reduced stress and improved the quality of life, it was not instrumental in bringing down the stress to minimal level and enhancing the quality of life to optimum level. Therefore, the findings point to the need of inclusion of psychological intervention along with the medical intervention for minimizing stress and optimizing the quality of life of patients with cancer.
Keywords
Cancer
Medical intervention
Quality of life
Stress
INTRODUCTION
Cancer is a chronic illness that can result in major lifestyle changes which may cause severe disruptions to a person's normal functioning in life, starting from illness to severe financial crises. People who live with cancer have a greater risk of developing various psychological problems. Studies show that cancer patients suffer not only from physical symptoms but also from the psychological and social stress associated with both diagnosis and treatment of their disease.[1] There is evidence that patients experience psychological distress at different points during the course of cancer. Unfortunately, psychological distress may remain unrecognized in certain cancer patients. Patients either do not communicate their feelings or they may be unaware of their distress.[2] The disease, its effects and treatment may show impact on several aspects of life, adding to their distress. Studies show that apart from the fear of dying, patients feel threatened by interventions, like chemo- or radio-therapy, and they worry about losing their bodily integrity, independence, and social roles.[3]
Quality of life is a broad, subjective, and multidimensional concept that includes physical health and symptoms, functional status and activities of daily living. Here quality of life (QOL) is a descriptive term that refers to “people's emotional, social and physical wellbeing and their ability to function in the ordinary tasks of living”.[4] It is seen that in the day to day practice, often owing to several limitations beyond their control, many medical practitioners focus more often upon the physical aspects of cancer-related outcomes. Thus studies show that assessment of quality of life of a cancer sufferer remains a neglected area.[5] Over recent decades cancer treatments have become more complex and intense. While these resulted in increasing survival rates, invasive therapies have also led to adverse psychological impact.
While studies as above show the impact of the disease as well as the treatment on the psychological variables like level of stress as well as QOL, there needs to be an integrative psychological intervention that handles the psychological aspects alongside the necessary medical treatment that deals with the disease. Research indicates a definite positive impact on treatment outcomes when an integrative approach that focuses on stress, symptom control and quality of life is provided along with the standard therapeutic regimens.[6]
Findings suggest that lung cancer is more prevalent in men, breast cancer is more prevalent in women,[7] and head and neck cancer is prevalent across the genders in India.[8] Hence, our study was designed to measure the effect of medical intervention on stress and QOL of patients with lung cancer, breast cancer and head and neck cancer. It was hypothesized that there would be an effect of medical intervention in reducing the level of stress and enhancing the QOL of these patients.
SUBJECTS AND METHODS
This intervention study involved a one-group pre-test-post-test pre-experimental design. The time gap between pre and post intervention psychological assessment was 6 weeks during which the participants were under three types of combined medical intervention, such as chemotherapy, radiation-hormonal therapy, and surgery.
Participants
Participants of the study consisted of 105 patients (50 male, 55 female) with three types of cancer viz. lung cancer, breast cancer and head and neck cancer selected by means of purposive sampling method from cancer hospitals from twin-cities of Hyderabad and Secunderabad in the state of Telangana of India. The sample comprised of 35 female patients with breast cancer, 35 (female 8, male 27) patients with lung cancer and 35 patients (female 12, male 23) with head and neck cancer. Their age group was between 28-65 years of age with mean age of 52 years.
Written informed consent forms were given to the patients with cancer and their consent was obtained. Only those patients who were willing to participate for the whole period of 6 weeks of study were included. Inclusion criteria also included newly diagnosed male and female patients with lung cancer, breast cancer, head and neck cancer between the age of 25–65 years, having no psychiatric illness irrespective of their occupation, place of living and socio economic status. Patients below the age of 25 years and above 65 years, and those having psychiatric illnesses and other physical illness were excluded from the study.
Research tools
(i) The Questionnaire on Stress in Cancer Patients-Revised Version (QSC-R23) was used to assess psychological stress in cancer patients.[9] It consists of 23 items that described potential everyday stress and in everyday language. There are five domains of QSC-R23, such as psychosomatic complaints, fears, information deficits, everyday life restrictions, and social strains. Scoring was done based on the instruction manual, which indicated that higher the scores higher was the stress.
(ii) European Organization for the Treatment and Research of Cancer Quality of Life Questionnaire, version 3.0. (EORTC QLQ-C30 version 3.0) was used for assessing health related quality of life for cancer patients (Aaronson et al.).[10] The questionnaire was organized into five functional scales (physical, role, emotional, cognitive and social), three symptoms scales (fatigue, nausea/vomiting and pain), a Global Health Status and quality of life (GHS/QoL) scale, and a number of single items assessing additional symptoms (dyspnoea, insomnia, appetite loss, constipation and diarrhoea) and perceived financial difficulties. Each item has a 4-point response scale (1 = not at all, 2 = a little, 3 = quite a bit, and 4 = very much) with the exception of the two items measuring Global Health Status/Quality of Life, which have 7-point response scales (1 = very poor to 7 = excellent). The scoring was done as per the procedure standard.[11] For the functional and global health and quality of life scales, a higher score indicated better functioning whereas for the symptoms-oriented scales and items, a higher score corresponded to a higher level of symptomatology.
Procedure
For conducting the study three cancer hospitals were identified and permission was taken to conduct the study. Initially senior consultants and doctors were approached to identify the patients newly diagnosed with three types of cancer under study. Such patients were included in the study after due permissions from the respective hospitals. Each identified patient was individually contacted and explained about the study. Those who consented to participate in the study were finally selected for the psychological assessment. Each of the selected participants was administered the research tools individually prior to the starting of medical intervention. During this psychological assessment, the doubts raised by the participants were clarified. However, three versions of the research tools—English, Hindi, and Telugu—were used as per the requirement of the participants. The QSC-R23 was translated into Hindi and Telugu with the help of two experts, who were proficient with the respective languages as well as English. The translated versions were again re-translated into English following the same procedure with another two experts, and matched with the original English version to check the item construction and validity of each of the items. The psychometric properties had been verified through pilot study. Since the Hindi and Telugu standard versions of the EORTC QLQ C30 were available, the same were used. After the initial assessment, individually tailored medical intervention was followed under the supervision of a senior medical oncologist. Reassessment with the above research tools was done after the completion of 6-week period of medical intervention. After the post assessment the participants were debriefed individually. An observation record was used for procedures used during medical intervention for a period of 6 weeks.
RESULTS
The obtained quantitative data were analysed by means of descriptive statistics, paired t-tests and Cohen's d by using IBM SPSS Statistics, ver. 20.0 and bar graphs were plotted accordingly. Table 1 shows the M, SD, t values, and effect sizes of the level of overall stress and its five dimensions, such as psychosomatic complaints, fears, information deficits, everyday life restrictions, and social strains in the total sample (N = 105) consisting of patients of three types of cancer such as lung cancer, breast cancer, and head and neck cancer.
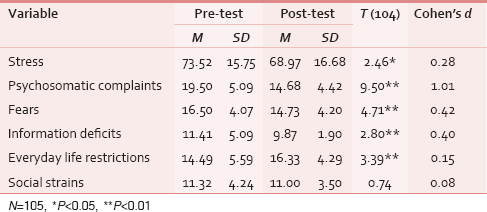
It is observed from Table 1 that there was a significant difference between pre and post medical intervention stress (overall) score, t (104) =2.46, P < 0.05 with medium effect size (Cohen's d =0.28). This indicated that overall stress score of the participants was significantly reduced after medical intervention (M = 68.97, SD = 16.68) compared to the stress score observed prior to medical intervention (M = 73.52, SD = 15.75). So far as the dimensions of stress are concerned, significant difference was found between the pre- and post-medical intervention scores of cancer patients in respects of psychosomatic complaints scores (t = 9.50, P < 0.01), reduction of fear scores (t = 4.71, P < 0.01), information deficit score (t = 2.80, P < 0.01), and everyday life restrictions scores (t = 2.80, P < 0.01), whereas no significant difference was observed in case of pre- and post-medical intervention social strains scores.
Moreover, the effect of medical intervention was found to be high in case of psychosomatic complaints (Cohen's d = 1.01), medium in case of reduction of fear (Cohen's d = 0.42) and information deficit (Cohen's d = 0.40), and low in case of everyday life restrictions (Cohen's d = 0.15). From Table 1, it is evident that the psychosomatic complaints scores, fears scores and information deficit scores of the patients significantly decreased after medical intervention whereas the reverse trend was noticed in case of life restrictions scores. The significant mean differences are shown in the form of bar graph in Figure 1.

- Mean stress scores during pre- and post-medical intervention MIA: Medical Intervention Assessment Stress: Overall Stress, psC: Psychosomatic complaints, FR: fears, ID: Information deficits, ELR: Everyday life restrictions, SS: Social strains
Table 2 shows M, SD, t values and effect sizes of the EORTC-QLQ-30 and its sub scales (GHS/QoL, functional and symptoms scales) in patients with cancer during pre- and post-medical intervention. So far as the functional scale of quality of life is concerned, significant difference was found between the pre- and post-medical intervention scores of cancer patients in respect of emotional functioning (t = 4.50, P < 0.01) and cognitive functioning (t = 2.63, P < 0.05). Among the symptoms scale of quality of life, significant differences were found between the pre- and post-medical intervention scores of cancer patients in nausea and vomiting (t = 3.23, P < 0.01) and pain (t = 5.85, P < 0.01) scores. In additional symptoms significant differences were found between the pre- and post-medical intervention scores of cancer patients in dyspnoea (t = 3.47, P < 0.01), appetite loss (t = 3.47, P < 0.01), and constipation (t = 6.24, P < 0.01).

The effect of medical intervention was found to be high in case of symptom scale (pain) and additional symptoms (constipation); medium in case of functional scale (emotional functioning, cognitive functioning) and symptoms scale (nausea, vomiting). In additional symptoms scale the effect of medical intervention was found to be medium in dyspnoea and appetite loss.
From Table 2, it is evident that the nausea and vomiting, pain, dyspnoea and appetite loss decreased after medical intervention and a reverse trend was noticed in case of emotional functioning, cognitive functioning, sleeping and constipation. The significant mean differences are shown in bar graph in Figure 2.

- Means of the dimensions of the quality of life scores during pre- and post-medical intervention. GHS/QoL: Global Health Status/ Quality of Life, PF2: Physical Functioning, RF2: Role Functioning, EF: Emotional Functioning, CF: Cognitive Functioning, SF: Social Functioning, FA: Fatigue, NV: Nausea / Vomiting, PA: Pain, DY: Dyspnoea, SL: Sleeping, AP: Appetite, CO: Constipation, DI: Diarrhea, FI: Financial difficulties
However, medical intervention did not have any impact on physical, role and social functioning scores under functional scale, fatigue score under symptoms scale, insomnia and diarrhoea scores under additional symptoms scale, was financial difficulties scores.
DISCUSSION
The results indicate that there is a medium effect of medical intervention on stress scores of patients with lung cancer, breast cancer, and head and neck cancer. Accepting the hypothesis, it is noticed that even though the stress decreased after intervention, the stress was in the same level of above average as per the scoring criteria. The finding is supported by a study which states that distress is very common in cancer patients across diagnoses and across the disease trajectory.[12] The same trend is also noticed for the individual dimension of stress, such as psychosomatic complaints, fears, information deficit and everyday life restrictions. The findings, thus, point out that though medical intervention is instrumental in reducing stress, it is not effective enough to manage it to minimal level. The findings to some extent contradict the findings of previous studies which state that during the course of treatment most of the patients with cancer were restricted to stay at home or are bed ridden and this leads to disturbance in their daily routine and their functional activities.[13]
Results indicate that there are no significant differences between pre- and post- medical intervention assessment scores of symptoms scale such as fatigue, insomnia, followed by single item scale like diarrhea and financial difficulties of the patients with cancer, and these symptoms were reported to be at moderate level. Similar findings were found a study[14] which shows that cancer patients suffer from multiple physical symptoms such as fatigue and pain and also from psychological changes such as fear of death and fear of progression or recurrence of disease, and changes in the quality of life. Previous studies have also shown that sleep disturbances are extremely troublesome to the patient and decrease the overall quality of life.[15]
It is seen that in functional scales, there is a significant difference between pre- and post- medical intervention scores of emotional functioning and cognitive functioning. It is also observed that emotional and cognitive functioning among patients with cancer is found to be better during post-medical intervention in comparison to pre-medical intervention assessment. These results are consistent partially with the findings of a previous study,[16] which reported high levels of physical functioning and emotional functioning in a sample of 558 breast cancer patients one month after the last component of primary treatment, that is surgery, radiation therapy (RT) or chemotherapy (CT). The same instrument (EORTC-QLQ-C30) used in the present study was used in another study for comparing the situation at the beginning of chemotherapy and at the end of inpatient treatment.[17] Their analyses showed that physical, emotional, and social functioning improved significantly from beginning of chemotherapy to the end of inpatient treatment. Yet another study found small but statistically significant improvements in cognition, as measured by the Mini Mental State Examination (MMSE), after 12 weeks of combined chemotherapy.[18]
On symptoms scale, it is observed that significant differences between pre- and post-medical intervention scores of nausea and vomiting, pain, dyspnoea and appetite loss. These symptoms are reduced during post-medical intervention in comparison to pre-medical intervention. Similar findings were reported by a study which reports decreased fatigue, nausea, loss of appetite and sleep disturbance in acute myeloid leukaemia of 28 patients.[18] On the other hand a significant difference is seen between pre- and post-medical intervention scores of constipation of the patients with cancer. The results also indicate that the constipation among patients with cancer increases during post-medical intervention in comparison to pre-medical intervention and the effect of medical intervention is found to be high. This may be attributed to the narcotic effect as reported by previous studies. One such study reports that about 50% of cancer patients experience constipation, other side effects can occur from this condition such as decreased appetite and nausea.[19] Another study reports that some chemotherapy and anti-sickness drugs can cause constipation.[20] However, to make the findings more relevant and useful, other significant factors, like gender, age, and types of cancer and medical procedure need to be considered. To understand the in-depth experience of the participants, future research should focus on mixed-method paradigm.
CONCLUSION
The change in the level of stress as well as the quality of life may be attributed to the resurgence of courage that the ongoing medical treatment may have provided. Thus, the findings reveal that though the medical intervention reduces stress and improves the quality of life, it is not instrumental in bringing down the stress to minimal level and enhancing the quality of life to optimum level. Therefore, the findings point to the need of inclusion of psychological intervention along with the medical intervention for minimizing stress and optimizing the quality of life of patients with cancer. The intervention should be designed aiming to help the patients overcome stress and cope better with the situation, cognitively reorient them positively so as to use a more realistic appraisal of their situation, such as psycho-education (educating the patients about the realities of the disease, treatment and recovery as well as helpful methods of coping), training (focusing on stress management techniques), and counselling (using cognitive restructuring to minimize stress and enhance quality of life in patients with cancer.
ACKNOWLEDGEMENT
The authors are grateful to the hospitals, doctors and patients who have participated in this study and contributed to the findings. The care givers of the patients need a special thanks for being supportive althrough. We are also thankful to C. Vanlalhruaii and Tia Mongla for assisting us in editing the manuscript.
Source of Support: No.
Conflict of Interest: None declared.
REFERENCES
- Emotional distress: The sixth vital sign-future directions in cancer care. Psychooncology. 2006;15:93-5.
- [Google Scholar]
- Assessment of psychosocial distress and resources in oncology - a literature reviews about screening measures and current developments. Psychother Psychosom Med Psychol. 2006;56:462-79.
- [Google Scholar]
- Emotional distress and needs for psychosocial support among breast cancer patients at start of radiotherapy. Psychother Psychosom Med Psychol. 2003;53:229-35.
- [Google Scholar]
- Elderly person's experience of living with venous leg ulcer: Living in a dialectal relationship between freedom and imprisonment. Scand J Caring Sci. 2001;15:235-43.
- [Google Scholar]
- Incorporating person centred care principles into an ongoing comprehensive cancer management program: An experiential account. Indian J Palliat Care. 2001;17:S61-7.
- [Google Scholar]
- Biennial Report (1988-1989) of National Cancer Registry Programme. New Delhi: Indian Council of Medical Research; 1992.
- [Google Scholar]
- Psychological problems of cancer patients: A cancer distress screening with a cancer-specific questionnaire. Br J Cancer. 2004;91:504-11.
- [Google Scholar]
- The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-76.
- [Google Scholar]
- on behalf of the EORTC Quality of Life Group. EORTC QLQ-C30 Scoring Manual. (3rd edn). Brussels: EORTC; 2001. p. :86.
- [Google Scholar]
- Efficacy and medical cost offset of psychosocial interventions in cancer care: Making the case for economic analyses. Psychooncology. 2004;13:837-49.
- [Google Scholar]
- Patterns of objective physical functioning and perception of mood and fatigue in post treatment breast cancer patients and healthy controls: An ambulatory psychophysiological investigation. Psychosom Med. 2008;70:819-28.
- [Google Scholar]
- Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: A cluster analysis. Oncol Nurs Forum. 2006;33:E79-89.
- [Google Scholar]
- Impact of surgery and chemotherapy on the quality of life of younger women with breast carcinoma: A prospective study. Cancer. 2001;92:1288-98.
- [Google Scholar]
- Quality of life in adult patients with acute myeloid leukemia receiving intensive and prolonged chemotherapy - a longitudinal study. Leukemia. 1998;12:586-92.
- [Google Scholar]
- Emotional distress in cancer patients at the beginning of chemotherapy and its relation to quality of life. J BUON. 2008;13:217-22.
- [Google Scholar]
- Mesothlioma. Chemotherapy Side Effects: Constipation. Available from: http://www.treatmentsformesothelioma.org/neuropathy.htm
- [Google Scholar]
- Macmillan. org [internet]. United Kingdom: Possible side effects of some chemotherapy drugs, Macmillan Cancer Support Online Resource, Inc., 2011-12. Available from: http://www.macmillan.org.uk/Cancerinformation/Cancertreatment/Treatmenttypes/Chemotherapy/Sideeffects/Possibleside-effects.aspx
- [Google Scholar]






