Translate this page into:
Analysis of Patterns of Palliative Radiotherapy in North West India: A Regional Cancer Center Experience
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Palliative radiotherapy (PRT) is the eventual requirement in 30-50% of all cancer patients. PRT is primarily aimed to relieve pain and prevent/treat collapse or fracture in case of bone metastasis, to reduce edema in patients with cranial metastasis, and to control distressing symptoms of rapid primary growth. An audit of PRT planned in a busy cancer center can help in the characterization of the requirements of the patients and the formulation of institutional policies.
Materials and Methods:
In total, 516 patients who received PRT in our regional cancer center from January 2012 to December 2012 and whose complete records were available for analysis were selected for this retrospective study. Medical records and radiotherapy files were analyzed to obtain data such as sociodemographic parameters, prescription of PRT, and follow up. Descriptive statistics were evaluated in terms of frequencies and percentages to allow comparisons.
Results:
Of the 516 patients, 73% patients were male; the median age of the patients receiving PRT was 62 years (range 13-83 years). About 48% (n = 248) patients received PRT at the primary site while rest (52%) were given PRT at the metastatic site. The most common indication of PRT was pain (56.8% cases), followed by cytostatic PRT (19.8%) and raised ICT (12.4%). The median dose prescribed was 30 Gy (range 8-36 Gy) delivered in 1-12 fractions over the duration of 1-18 days. The overall response rate was about 43% at 2 weeks of completion of PRT; the median follow-up of the patients was 154 days (range 9-256 days). The long-term symptom relief at median follow up was 8%.
Conclusions:
Good clinical judgment and expertise is required in prescribing correct fractionation schedule to achieve effective symptom palliation with lowest possible cost and inconvenience to the patients and relatives. Hypofractionated radiotherapy is a feasible treatment option in patients with advanced incurable disease to achieve effective palliation.
Keywords
North West India
Palliative radiotherapy
Regional cancer center
Sociodemographic parameters
INTRODUCTION
Despite various developments in the field of cancer diagnosis and treatment, many patients develop incurable disease. These patients, though incurable, should be offered appropriate treatment to maximize their quality of life. Palliative care, as defined by world health organization (WHO), is “the active total care of patient whose disease is not responsive to curative treatment”.[1] A patient with advanced incurable disease may tolerate the anti-neoplastic treatment poorly and may become further disabled. Thus, an oncologist should try to maintain an intricate balance between expected symptom relief and the possible toxicities of the treatment. Palliative radiotherapy (PRT) is required in 30-50% of all cancer patients, and the primary aim of PRT is to provide adequate pain and symptom relief. Hypofractionated radiotherapy provides efficient palliation of symptoms. There might be complex issues pertaining to pain, physical symptoms, and psychosocial aspects coexisting during PRT, which needs to be adequately addressed by a palliative care unit.[2] Besides providing pain relief, PRT is useful to prevent/treat collapse or fracture in case of bone metastasis, to reduce headache and edema in patients with cranial metastasis, and to control distressing symptoms of rapid primary growth, e.g. PRT in cases of recurrent breast cancer. In this article, we present a review of the medical records of the patients who received PRT in our institute. Such a review is required for the characterization of the requirements of the patients and the formulation of institutional policies.
MATERIALS AND METHODS
In total, 516 patients, who received PRT at our institute from January 2012 to December 2012 and whose complete records were available for analysis, were selected for this retrospective study. Our institute is a Regional Cancer Center with separate palliative care facilities, thus providing comprehensive palliative management of patients with advanced incurable disease. The treatment goal in such patients is to achieve the best possible quality of life. Patients who underwent PRT were included in this study, irrespective of age, sex, primary disease, site of radiotherapy, or site of metastasis, the only selection criteria being availability of sufficient treatment details and records of sociodemographic parameters. The following data were retrieved from the medical records and radiotherapy files: Age, sex, symptoms, site of primary, site of metastasis (if any), response to PRT, and last follow up. The descriptive statistics of the PRT data were evaluated in terms of frequencies and percentages to allow comparisons. The PRT dose ranged from 8 Gy to 30 Gy given in the fractionation of 3-8 Gy per fraction. For bone metastasis, two fractionation schedules were primarily used: 8 Gy in single fraction or 30 Gy in 10 fractions. The latter was also used for cranial metastasis, superior vena caval (SVC) syndrome, and achieving hemostasis. The allocation to the fractionation schedule was based on the discretion of radiation oncologist and based on the patient's general condition. All patients were treated on a telecobalt machine with two-dimensional radiation planning. Lead fiducial markers were used to obtain portal film and confirm the dose delivery. The response to cranial radiotherapy was assessed by improvement in performance status and resolution of symptoms, such as headache and vomiting. The response to PRT for SVC was assessed by relief from dyspnea and resolution of symptoms of vein engorgement and pain. All responses were recorded as one of the four categories: Complete relief, partial relief, stable, and progressive status. The second line PRT schedule for patients with bone metastasis used was 600 cGy in single fraction in all the patients in whom pain or weakness of the lower limbs reappeared. This second line PRT was used after a minimum interval of 4 weeks. In patients with advanced gynecologic malignancies, two schedules were used: 5 fractions of 300 cGy or 3 fractions of 400 cGy. The fractionation used for patients with advanced bladder carcinoma was 300 cGy five fractions followed by conventional fractionation in patients with better life expectancy. In patients with fungating lesions and large neck nodes, two PRT schedules have been used in our institute with a fractionation of 600 cGy given weekly for 5 weeks and 300 cGy 14 fractions given 5 days a week. In patients with fungating lesions and large neck nodes due to head and neck cancer, two PRT schedules have been used in our institute with a fractionation of 600 cGy given weekly for 5 weeks and 300 cGy 14 fractions given five days a week. Conventional fractionation was employed to complete the curative dose in those achieving good response and good life expectancy.
RESULTS
Characteristics of patients
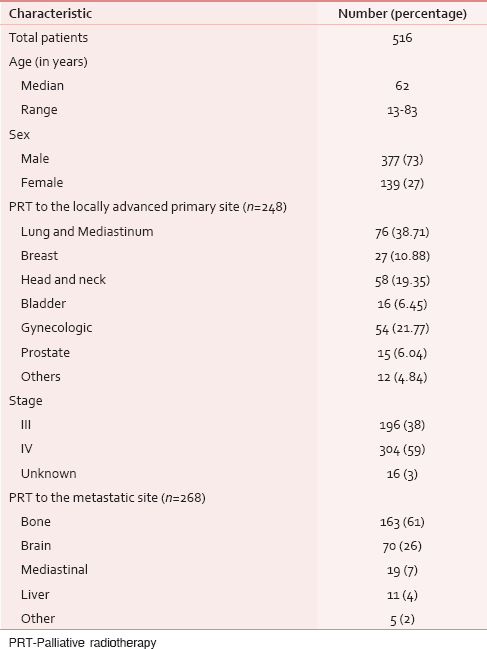
Out of 516 patients analyzed in this study, 73% patients were male; the median age of the patients receiving PRT was 62 years (range 13-83). About 48% (n = 248) patients received PRT at the primary site. The primary site of the disease was lung in 38.7% of the patients followed by head and neck (19.4%) and breast (10.8%). Patients with gynecologic malignancies and prostate cancer accounted for 21.8% and 6.1% of the cases, respectively. About 59% patients were stage IV at the time of prescription of PRT while 38% belonged to stage III. Distant metastasis was identified in 52% of the patients, with the most common site being bones (64%) followed by brain (26%) [Table 1]. About 26% of the patients had received chemotherapy before starting PRT while concurrent chemoradiotherapy was given to 8% of the patients. The median dose prescribed was 30 Gy (range 8-36 Gy) delivered in 1-12 fractions over the duration of 1-18 days. Upfront PRT was prescribed to 64% of the patients due to metastatic presentation or poor performance status of the patients. The most common indication of PRT was pain (56.8% of the cases), followed by cytostatic PRT (19.8%) and raised ICT (12.4%) [Table 2]. Cytostatic PRT was aimed to control bleeding, to relieve pressure symptoms, and to control excess discharge or pain arising from ulceration.

Results of PRT
About 6% patients had complete relief for all symptoms for which PRT was indicated, while 37% patients got partial relief; thus, the overall response was about 43%. About 28% had stable symptoms while 12% developed progression of the symptoms. About 5% patients died within 2 weeks of completion of PRT while 11% were lost to follow up [Table 3]. The median follow-up of the patients receiving PRT was 22 weeks (range 9-256 days). Table 4 depicts the median and range of palliative radiotherapy dose, fractions and follow up duration. Further radiotherapy was prescribed to 23% of the patients. The median duration of response of bone metastasis to PRT was about 36 days after completion of PRT. The overall response rate was 54%; the retreatment rate was 16%. In patients who received palliative cranial radiotherapy, the overall response rate was 53%. The overall median survival was 2.6 months and survival at one year was 8.57%. In patients receiving PRT for SVC syndrome, the response was obtained in median 6 days in about 73% of the patients. Hydronephrosis was relieved in 54% patients receiving PRT for advanced gynecologic malignancies. Hematuria was resolved in 84% patients receiving PRT for advanced bladder carcinoma. The response to PRT for head and neck cancer was about 46% with 20% patients proceeding to receive the curative dose.


DISCUSSION
Palliative treatment is aimed to provide symptomatic relief and the best achievable quality of life in patients suffering from incurable diseases. There is an important misconception among the physicians who still refer to palliative medicine to be a branch completely focused on the care of terminally ill patients.[3] Thus, there is an urgent need to spread awareness of the importance of palliative medicine. PRT is an important tool for an oncologist to provide effective pain relief, to reduce the intracranial tension, to relieve compressive symptoms and dyspnea, to enable regression of fungating mass, and to achieve hemostasis in the appropriate settings. Most of the schedules used for PRT are hypofractionated based on the shorter life expectancy and problems of protracted treatment with conventional fractionation.
Bone metastasis
PRT is an effective tool to provide relief from painful bone metastases. The standard treatment for palliation of bone metastases has been daily treatment for 2-3 weeks with doses of 30-35 Gy in 10-14 treatments. In our patients with skeletal metastasis, the fractionation schedule mostly used were 8 Gy in single fraction or 30 Gy in 10 fractions depending upon the patients general condition and choice of the consultant. This is in accordance with the result of multiple randomized, prospective trials in the last 30 years, which have concluded that single-dose treatment of 8 Gy provides pain relief similar to longer treatment regimens.[456] In most of these studies, there were no differences reported in pain relief or pain medication requirements between the treatment regimens. Hoskin et al. reported that pain responds to PRT in about 60% of the patients.[7] The overall response rate in our study was 54% while the retreatment rate was 21% after single fraction and 4% after multiple fractions. This is in accordance with previous studies in which the need for retreatment ranged from 11% to 29% after single-fraction therapy, compared with 0-24% after multiple-fraction treatment.[8910]
Brain metastasis
Whole brain radiotherapy (WBRT) is an effective measure to control symptoms of raised intracranial tension in patients with multiple cranial metastases. Solitary brain metastasis with controlled primary disease should be considered for surgical resection.[11] Stereotactic radio surgical treatment is another attractive option for patients with isolated cranial metastasis. We referred patients of isolated cranial metastasis with controlled extracranial primary for neurosurgery. WBRT was delivered in 24% patients, with majority of patients having primary of lung (54%) and breast (28%). The most common fractionation schedule used for cranial radiotherapy in our study patients was 300 cGy in 10 fractions delivered over two weeks. Brain metastasis is a common unfortunate event in many advanced malignancies. The treatment of such patients typically starts with dexamethasone. Mehta et al. reported it to improve edema and neurological deficits in about 70% of the patients.[12] In our patients, injectable dexamethasone was started by admitting the patients immediately after diagnosis of brain metastasis along with an injection of mannitol. The median survival with steroids alone is estimated to be only about 2 months. Murray et al. reported that the median survival could be increased to approximately 4-6 months in such patients by addition of WBRT.[13] Radiation therapy oncology group trials have reported about 60% cumulative response rates.[14] The response rate attained in our patient cohort was about 53%. This may be ascribed to delayed presentation of our patients with multiple cranial metastases with poor overall general condition.
Lung and mediastinal PRT
Thoracic symptoms including SVC syndrome are effectively palliated with hypofractionated radiotherapy. In our study, 6.9% patients had features of SVC syndrome. Other thoracic symptoms for where PRT was used included dyspnea, chest pain, and hemoptysis. PRT is described as the primary treatment modality in such patients. Various studies have reported employing either 16 Gy or 17 Gy in 2 fractions or 20 Gy in 5 fractions for PRT of non-small cell lung cancer.[151617] Few severe side effects were noted, and symptom response was consistent between the studies. In patients with acute, life-threatening symptoms, emergency radiotherapy can be started even without histological diagnosis.[18] In our study, relief of symptoms (dyspnea and venous engorgement) was obtained in median 6 days in about 73% of the patients. Knopp et al. reported that 85-90% of the patients attained symptomatic relief within three weeks.[19]
Gynecologic malignancies
Locally advanced pelvic malignancies may cause distressing symptoms, including pain, discharge, bleeding, and hydronephrosis leading to obstructive uropathy. In a Phase II RTOG trial, patients with advanced gynecologic and genitourinary malignancies were treated with a total dose of 44.4 Gy in 12 fractions.[20] The dose was given as 3.7-Gy fractions twice daily for 2 days with 3-6-week breaks after 14.8 Gy and 29.6 Gy. The patients had acceptable acute and long-term side-effect rates, with an overall response rate of about 40%. In our patients, two schedules were used: 5 fractions of 300 cGy or 3 fractions of 400 cGy. Hydronephrosis was relieved in 54% patients, and they were given conventional fractionation to complete the dose.
Genitourinary malignancies
In patients of locally advanced prostate cancer presenting with lower urinary tract symptoms or hematuria, PRT led to response in 78% of the patients. This is in accordance with the study by Kynaston et al., in which they observed a response of 88% by employing 35 Gy in 15 fractions or 24 Gy in 3 weekly fractions.[21] In a randomized trial by Duchesne et al., similar palliation rate of about 70% along with similar side effects and survival rates were obtained by using either 35 Gy in 10 fractions or 21 Gy in 3 fractions for patients with locally advanced, inoperable bladder carcinoma.[22] The fractionation used in our study was 300 cGy five fractions followed by conventional fractionation in patients with good life expectancy. Our patients had 84% response rate in terms of resolution of hematuria.
Head and neck cancer
In developing countries, patients of head and neck cancer usually present with locoregionally advanced disease. In patients with fungating lesions and large neck nodes, two PRT schedules have been used in our institute with a fractionation of 600 cGy given weekly for 5 weeks and 300 cGy 14 fractions given five days a week. Conventional fractionation is employed to complete the curative dose in those achieving good response and good life expectancy. The response to both the schedules is about 46% with no major differences in acute toxicities. About 20% patients proceeded to receive the curative dose. The median survival was 7.6 months (2.5-11 months). In a study by Mohanti et al. employing 20 Gy in 5 fractions, symptom relief for pain, dysphagia, hoarseness, cough, and otalgia was obtained in 47-59% of the patients following PRT.[23] In a regimen entitled the Quad Shot, consisting of 14 Gy in 4 fractions given twice per day for 2 consecutive days, the median survival was 5.7 months.[24] The regimen was repeated at 4-week intervals for an additional 2 courses if there was no tumor progression.
Many patients who receive treatment near the end of life require an intense effort to achieve transportation out of the home; thus, the optimal intervention for this group is 1 visit that includes consultation, dose planning, and delivery of a single-fraction treatment–a series of tasks that may be completed within 2 hours at most radiotherapy centers.[25] The toxicity profile of radiotherapy has a clear advantage over systemic therapy as the deleterious effects are usually limited to the anatomic site of treatment and for a shorter time, whereas systemic therapy often cause functional deficits in several organ systems.
Limitations of the study
The precise information about the quality of life was not available in the records; hence, it could not be quoted in the study. However, there was qualitative improvement of the patients as mentioned in the data was included in the study. In addition, there was limited use of standard pain assessment scales in the records making the comparisons difficult.
CONCLUSIONS
Shorter courses of hypofractionated PRT exemplify common sense end-of-life care and palliation, especially because most patients who are treated for symptom palliation will not survive to face the increased risk of long-term side effects associated with hypofractionated regimens. Good clinical judgment and expertise is required to prescribe the correct fractionation schedule for achieving effective symptom palliation with lowest possible cost and inconvenience to the patients and relatives. Hypofractionated radiotherapy is a feasible treatment option in patients with advanced incurable disease to achieve effective palliation.
ACKNOWLEDGEMENTS
The authors would like to thank the consultants in the department of Oncology Dr. Ajay Sharma, Dr. N Sharma, Dr. Surender Beniwal and Dr. S L Jakhar. Also, they express gratitude to PG Students of the department: Dr. Sitaram, Dr. Daleep, Dr. Guman, Dr. Murali, Dr. Tanya, Dr. Rajesh, and Dr. Ramesh Purohit
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Pattern of palliative care, pain management and referral trends in patient receiving radiotherapy at a tertiary cancer center. Indian J Palliat Care. 2009;15:148-54.
- [Google Scholar]
- Disclosing gaps between supportive and palliative care: The past 20 years. Support Care Cancer. 2008;16:109-11.
- [Google Scholar]
- Palliative radiotherapy for painful bone metastases: Short-course or long-course? Ann Palliat Med. 2012;1:78-80.
- [Google Scholar]
- The effect of a single fraction compared to multiple fractions on painful bone metastases: A global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52:101-9.
- [Google Scholar]
- Single versus multiple fractions of palliative radiotherapy for bone metastases: A randomized clinical trial in Iranian patients. Curr Oncol. 2008;15:151.
- [Google Scholar]
- Oncology for palliative medicine. New York: Oxford University Press; Bone metastases; 2003. p. :271-89.
- [Google Scholar]
- Prospective randomized trial of single and multifraction radiotherapy schedules in the treatment of painful bony metastases. Radiother Oncol. 1986;6:247-55.
- [Google Scholar]
- A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bony metastases. Clin Oncol (R Coll Radiol). 1989;1:59-62.
- [Google Scholar]
- A prospective randomized trial of 4 Gy or 8 Gy single doses in the treatment of metastatic bone pain. Radiother Oncol. 1992;23:74-8.
- [Google Scholar]
- Management of single brain metastasis: A practice guideline. Curr Oncol. 2007;14:131-43.
- [Google Scholar]
- The dandelion effect: Treat the whole lawn or weed selectively? J Clin Oncol. 2011;29:121-4.
- [Google Scholar]
- A randomized phase III study of accelerated hyperfractionation versus standard in patients with unresected brain metastases: A report of the Radiation Therapy Oncology Group (RTOG) 9104. Int J Radiat Oncol Biol Phys. 1997;39:571-4.
- [Google Scholar]
- Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997;37:745-51.
- [Google Scholar]
- Palliative treatment of advanced non small cell lung cancer with weekly fraction radiotherapy. Indian J Cancer. 2000;37:148-52.
- [Google Scholar]
- Short-course palliative radiotherapy in non-small-cell lung cancer: Results of a prospective study. Am J Clin Oncol. 2000;23:83-93.
- [Google Scholar]
- Prospective study of palliative hypofractionated radiotherapy (8.5 Gy×2) for patients with symptomatic non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004;58:1098-105.
- [Google Scholar]
- Radiotherapy for palliation of symptoms in incurable cancer. Curr Probl Cancer. 1997;21:129-83.
- [Google Scholar]
- Lung cancer. In: Dow K, Buchottz J, Iwamoto R, Fieler V, Hilderley L, eds. Nursing Care in Radiation Oncology (2nd ed). Philadelphia: Saunders; 1997. p. :293-315.
- [Google Scholar]
- Phase II study of multiple daily fractionations in the palliation of advanced pelvic malignancies: Preliminary report of RTOG 8502. Int J Radiat Oncol Biol Phys. 1989;17:659-61.
- [Google Scholar]
- Radiotherapy for palliation of locally advanced carcinoma. Br J Urol. 1990;66:515-7.
- [Google Scholar]
- A randomized trial of hypofractionated schedules of palliative radiotherapy in the management of bladder carcinoma: Results of a Medical Research Council trial BA09. Int J Radiat Oncol Biol Phys. 2000;47:379-88.
- [Google Scholar]
- Short course palliative radiotherapy of 20 Gy in 5 fractions for advanced and incurable head and neck cancer: AIIMS study. Radiother Oncol. 2004;71:275-80.
- [Google Scholar]
- The ‘QUAD SHOT’--a phase II study of palliative radiotherapy for incurable head and neck cancer. Radiother Oncol. 2005;77:137-42.
- [Google Scholar]






