Translate this page into:
The Prevalence of Severe Pain, its Etiopathological Characteristics and Treatment Profile of Patients Referred to A Tertiary Cancer Care Pain Clinic
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pain is the most feared symptom in cancer. About 52–77% patients suffer pain despite World Health Organization (WHO) recommendations. Out of total, one-third patients suffer moderate to severe pain. This study was undertaken to determine the prevalence, etiopathogenesis and characteristics of severe pain and treatment response among pain clinic referrals in a busy tertiary care cancer center. This study found a high prevalence (31.5%) of severe pain. A total of 251 patients who had complete pain data were analyzed for etiopathological characteristics and treatment response. Head and neck cancer contributed the highest prevalence among all regions. Oncologists prescribed non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol with or without mild opioids to 14% patients and pain clinic physicians prescribed opioids and overall 63.7% patients had a better response after pain clinic referral, even then, morphine was not prescribed to many deserving patients. Doctors need pain education about opioids to remove any fear of prescribing opioids in presence of severe pain.
Keywords
Cancer pain
Prevalence of pain
Severe pain
INTRODUCTION
An estimated 6.6 million people worldwide die from cancer every year and the number is escalating. The World Health Organization (WHO) estimated that of the 9 million new cancer cases, more than half are found in developing countries. Unrelieved cancer pain continues to be a major issue despite WHO ladder (1986) recommendations. About 53% patients suffer pain at all stages of the disease. According to a systematic review of cancer pain prevalence, 59% patients suffer pain during active therapy phase and 65% suffer during advanced disease.[1]
In an advanced stage of the disease, 70% to 80% patients suffer from moderate to severe pain. The consequences of unrelieved cancer pain are devastating and can include functional impairment, immobility, and social isolation, emotional and spiritual distress with a significant negative impact on the patient. As the pan-European cancer pain prevalence study (2009) comprising 5,084 patients’ survey reported that 56% suffered moderate to severe pain at least monthly, and treatment of cancer was overall suboptimal.[23]
Many international bodies have reported that cancer pain can be controlled in almost 90% patients successfully using available knowledge from published literature including the WHO guidelines. Yet, pain is the most feared symptom despite great strides in the understanding of pain pathophysiology, discovery of newer analgesics, and advanced cancer therapies worldwide. The disease may be incurable, but even relief from pain seems to be a distant dream for most patients. Overall, 33% patients suffer pain of moderate to severe pain intensity. Such patients are known to express greater fear of pain and suffering than death itself.[4] Severe pain that affects one's performance of activities of daily living and enjoyment of life, has been found to be a predictor of anxiety and depression.[5] The objective of this study was to determine the prevalence, etiopathogenesis, and characteristics of severe pain and treatment response in cancer patients presenting to the pain clinic.
MATERIALS AND METHODS
This retrospective observational study was carried out after obtaining a formal approval from the Institutional Review Board. Adult patients who presented with severe pain (pain score of ≥7 on the numerical rating scale: 0–10) to the pain clinic during 1-year study period (January–December 2010) were included in the study. Details of disease extent, administered cancer therapy, temporal patterns of pain (site, type, intensity, and duration of pain, exacerbation/relieving factors) as described by the patient, inferred cancer pain syndromes, ongoing analgesics with response prior to first pain clinic visit to analgesics prescribed at the pain clinic, and follow-up data were collected from case record forms completed by the treating pain physician at the time of first assessment visit and at the time of follow-up which was usually after a week.
Data was analyzed using the statistical software Statistical Package for the Social Sciences (SPSS) 18. All the variables are presented as percentages.
RESULTS
A total of 2,200 new patients were referred to the pain clinic during two years period. Severe pain was noted in total 701 patients, out of which a complete pain record was found of 251 (11.40%). Of the 251 patients analyzed, 64.1% were male and rest female. Mean age was 52.5 years (45 – 60 years).
Service-wise distribution
Out of total 251 patients, 29.9% had head and neck cancers, 20.7% had gastrointestinal tract-related cancers, 15.1% thoracic cancers, while breast, bone, and soft tissue cancers had 10.4% each [Figure 1].
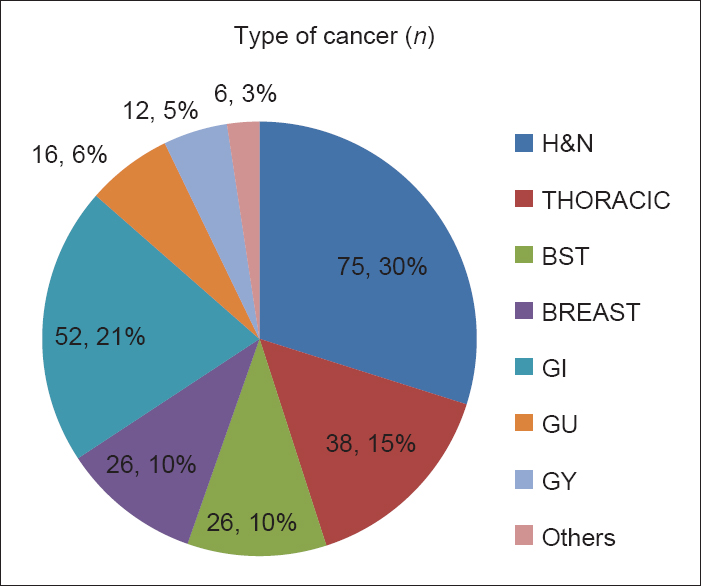
- Service-wise distribution (n = 251)
Characteristics of pain
Of the 251 patients, localized pain was found in 83.7%, dull aching pain (32.3%), stabbing pain (20.7%), pricking (12%), and had shooting (10.8%) type of pain. Episodes of breakthrough pain were noted in 49.8%. Pain was attributed to due to tumor in 83.3% [Figure 2].
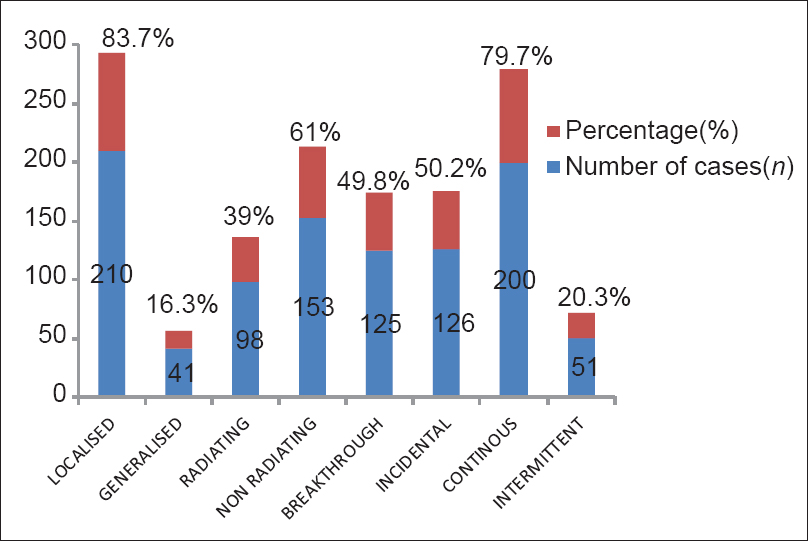
- Characteristics of pain
Various pain syndromes were identified: Visceral pain syndrome (26.7%), head and neck pain syndrome (23.5%), skeletal metastasis pain syndrome (20%), and rest others had brachial plexopathy, Soft tissue sarcoma (STS), and pelvic pain [Figure 3].
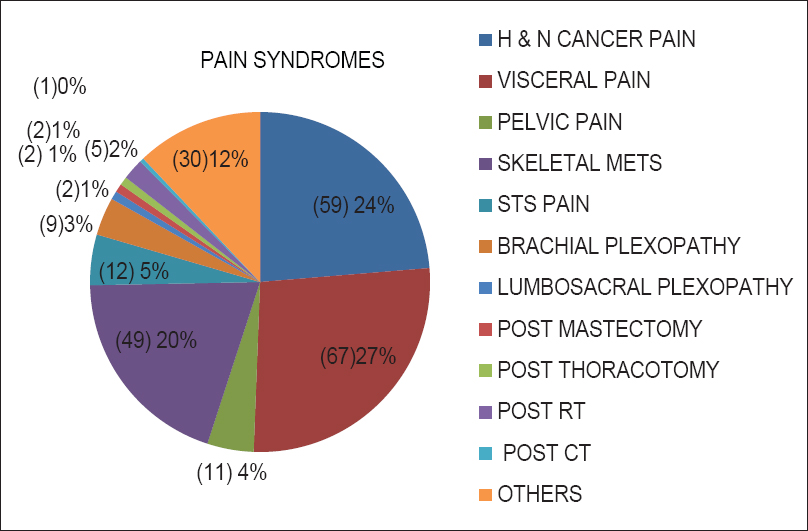
- Inferred cancer pain syndromes
Pharmacological treatment
At the time of the presentation to the pain clinic, all patients were receiving analgesics prescribed by referring unit. Around 25.1% were receiving paracetamol, 55.5% NSAIDs, 14.4% were receiving weak opioids (tramadol or codeine with NSAIDs combinations), and only 2% on oral morphine. Prescription by pain clinic physicians included paracetamol (61.8%), NSAIDs (42.6%), and opioids (52.6%) including oral morphine (31.5%) in modest starting doses. Anti-depressants and anti-convulsants were prescribed in 72% patients. None of the patients received any neurolytic nerve blocks. At thefirst follow-up with the pain clinic, 63.7% of the patients were found to have a pain score of 3/10 or less on Numerical rating scale (NRS) 0–10 scale.
DISCUSSION
This retrospective study found a 31.5% prevalence of severe pain among chronic pain patients referred to the pain clinic of a tertiary care cancer hospital. The study shows that often inappropriate medication prescribed (not by the WHO ladder) and/or fixed schedule dosing was not used (not by the clock). Oral morphine was prescribed to fewer patients even in severe pain, pointing possibly to the lack of education about opioids and existence of opiophobia among doctors.
Majority of the referred patients with severe pain at the first visit to the pain clinic (n = 251) were found opioid naïve (85%) and were treated only with NSAIDs or paracetamol by primary oncological services. Most patients (83.7%) had pain due to tumor while only <10% patients had pain pertaining to cancer therapy (surgery, radiotherapy, or chemotherapy) and only fewer had non-cancer pain. More than 70% patients had advanced disease and head and neck cancer was the most common diagnosis. About 63.7% patients responded well after initiation of opioids and adjuvants consequent the referral.
Overall, literature shows that 53% patients suffer pain during all stages of the disease. About 64% patients with advanced disease complain of unrelieved pain with more than one-third grading their pain as moderate or severe.[123] A Taiwanese study (n = 296) reported a high prevalence of severe pain among newly diagnosed cancer patients.[6] About 65% patients suffered significant worst or 31% significant average (>5.0) pain and 69% never received any analgesics at the time of first diagnosis of cancer. Most of these patients either had distant metastasis or not been prescribed appropriate analgesics (not by the ladder) or appropriate analgesic not at the fixed scheduled dosing (not by the clock). Most of these patients had inoperable lesion and not taking analgesic as per fixed schedule. Our results are similar as reported by the systematic review (2007) and the Taiwanese study.[16]
There could be many reasons for occurrence of severe pain. Either the patient had not been treated as per the WHO guidelines due to lack of knowledge or fear of prescribing strong opioids and its side effects or patient is having opioid resistant pain. This study found that only 14.4% patients with severe pain (n = 251) were treated with opioids (only 2% patients received morphine) by primary oncology unit doctors. Subsequent to pain clinic referral, 52.6% patients were prescribed opioids out of that only 32.2% patients had been prescribed oral morphine.
Patients started on strong opioids as a first-line analgesic require significantly fewer changes in therapy and are known to have better pain relief.[78] Anti-depressants and anti-convulsants were also prescribed contributing to a higher success of analgesic regime. Many of these patients were treated by anesthesiology resident doctors who may not have sufficient education or training in treating chronic pain patients.
The WHO ladder (1986) is a simplistic approach recommended initially to treat cancer pain globally across all levels of care using oral analgesics in a clock regulated manner. It can successfully relieve pain in about 75% patient.[9] However, it has many limitations. It does not take into account the disease extent, administered cancer therapy, mechanism of pain, type of pain, opioid responsiveness, psychological issues, and lastly the role of pain interventions. A questionnaire survey reported that 80% patients can be treated successfully using morphine in hospice but only 39% in hospital setting.[10] If morphine is prescribed by an oncologist at an early stage, then patient may perceive it as therapeutic failure. Some patients feel that morphine may hasten death. However, there is no evidence to confirm this fear.
Pain is a biopsychosocial issue and its successful treatment requires multi-dimensional assessment and multi-disciplinary treatment. National Cancer Control Network (NCCN) guidelines refers to an alternative acceptable approach that each patient is evaluated based on his or her stage of disease, response to treatments, and multiple therapies can be employed in a flexible manner simultaneously. Mechanism based approach should be adopted rather than disease or pain intensity-based approach for the successful treatment of cancer pain, especially in bone metastasis or neuropathic pain wherein opioids may be unresponsive.
This study found that main etiopathological factors responsible for severe pain were: Breakthrough pain (49.8%), bone metastatic pain (20%), and brachial plexopathy (12%) [Figure 3]. The prevalence of breakthrough pain has been reported to be 19–95% among various groups of patients.[11] Breakthrough pain appears to be more common in patients with advanced disease, poor performance status, vertebral metastasis, or plexopathies.
Patient education is the key to successful management of severe pain. Explanation of the cause of pain and giving hope to the patient goes a long way in treating pain. The various options available to control pain should be discussed. The right approach is to control background pain first, then to control breakthrough pain using appropriate drug by appropriate route. When oral analgesics fail to provide even 50% pain relief and cause untoward side effects limiting their efficacy, nerve blocks may be used as adjuvant therapy, wherever applicable. About 10% of patients may require interventional techniques (peripheral nerve blocks, autonomic nervous system blocks, radiofrequency lesions, and neurosurgical procedures) as part of a multi-modal, multi-disciplinary approach to pain control.
The limitations of this study are same as inherent in any retrospective observational study. It may not show a true prevalence of severe pain in a tertiary care cancer centre since all patients with severe pain are not referred to pain clinic and patients with incomplete pain records were not included in the study. Patients do not stay at tertiary care centre for their adequate pain control, once declared palliative, as many have advanced disease. Therefore, the proper response of the prescribed pain treatment could not be evaluated. Complete pain data including details of administered cancer therapy and actual analgesics prescribed, issued and taken by the patients could not be ascertained in many patients. A true picture of treatment responses may be possible only in a prospective controlled study.
In conclusion, the study shows a high prevalence of severe pain in a tertiary care cancer pain clinic. Severe pain was not treated with strong opioids either due to lack of knowledge or opioiphobia fearing side effects.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Ann Oncol. 2007;18:1437-49.
- [Google Scholar]
- Cancer-related pain: A pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20:1420-33.
- [Google Scholar]
- An international survey of cancer pain characteristics and syndromes. IASP Task Force on Cancer Pain. International Association for the Study of Pain. Pain. 1999;82:263-74.
- [Google Scholar]
- Suffering in the advanced cancer patient: A definition and taxonomy. J Palliat Care. 1994;10:57-70.
- [Google Scholar]
- Psychological distress of patients with advanced cancer: Influence and contribution of pain severity and pain interference. Cancer Nurs. 2006;29:400-5.
- [Google Scholar]
- The prevalence and severity of cancer pain: A study of newly-diagnosed cancer patients in Taiwan. J Pain Symptom Manage. 1998;15:285-93.
- [Google Scholar]
- World Health Organization guidelines for cancer pain: A reappraisal. Ann Oncol. 2005;16:132-5.
- [Google Scholar]
- Morphine is not the only analgesic in palliative care: Literature review. J Adv Nurs. 2004;45:527-32.
- [Google Scholar]
- Validation of the World Health Organization Guidelines for cancer pain relief: A 10-year prospective study. Pain. 1995;63:65-76.
- [Google Scholar]
- A comparison of the quality of care provided to cancer patients in the UK in the last three months of life in in-patient hospices compared with hospitals, from the perspective of bereaved relatives: Results from a survey using the VOICES questionnaire. Palliat Med. 2009;23:190-7.
- [Google Scholar]
- Working Group of an IASP Task Force on Cancer Pain. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med. 2004;18:177-83.
- [Google Scholar]






