Translate this page into:
Availability, Current issues, and Anticipation Training for Clinician-Patient Communication in Palliative Care: Learning and Doing or Learning by Doing?
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Following up on the previously published letter to editor[1] emphasizing “interpersonal communication skills in palliative care,” we intend to throw light on a recently evolving training methodology that aims to improve clinician-patient communication, namely the “availability, current issues, and anticipation (ACA)” model.
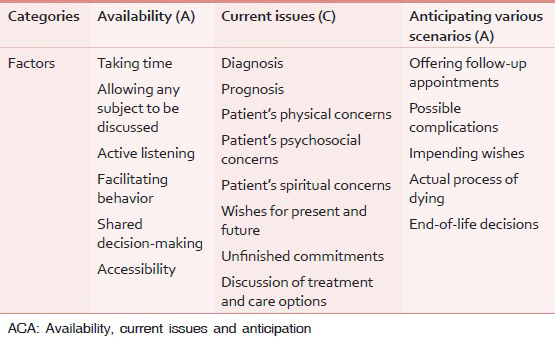
Slort et al.[2] developed the novel ACA training program on general physician (GP)-patient communication in palliative care, which focused on the following three categories [Table 1]: Availability of the GP for the patient, Current issues that should be raised by the GP, and Anticipating various scenarios. It subsequently described category-specific factors: Six factors for Availability (taking time, allowing any subject to be discussed, active listening, facilitating behavior, shared decision-making, and accessibility), eight factors for Current issues (diagnosis, prognosis, patient's physical concerns, patient's psychosocial concerns, patient's spiritual concerns, wishes for present and future, unfinished commitments, and discussion of treatment and care options), and five factors for Anticipating (offering follow-up appointments, possible complications, impending wishes, actual process of dying, and end-of-life decisions).
Two studies were reported by Slort et al.[34] The first one studied 126 GPs of whom 64 received ACA training and 64 were controls and compared the content analysis scores of Roter Interaction Analysis System (RIAS) for a videotaped 15-min consultation of each GP with a simulated palliative care patient between both groups. The second one was on 116 GP trainees of whom 54 received ACA training and 64 acted as controls. Both studies did not find any effect of ACA training on the RIAS scores, either on the number of issues discussed or on the quality of GP or GP trainees’ communicative behavior.
Although the ACA approach was developed and studied by same group of authors, and was surprisingly shown to be ineffective, it is yet to be content validated and cross-culturally adapted to suit the scenario in developing countries. The ACA model appears to be comprehensive and patient-focused, but the studies on its effectiveness did not measure patient-focused outcomes, or were not on real patient population, or on interdisciplinary training, which are scope for future research in this area.
The major concerns in using this model in the palliative care settings of developing countries include the level of knowledge and practical skills in the application of ACA model, perceived professional/provider attitudes, and patient/caregiver preferences and their experiences, which are to be taken into consideration prior to its use in the palliative care settings of developing countries.
REFERENCES
- Interpersonal communication skills and palliative care: “Finding the story behind the story”. Indian J Palliat Care. 2014;20:62-4.
- [Google Scholar]
- The ACA training programme to improve communication between general practitioners and their palliative care patients: Development and applicability. BMC Palliat Care. 2012;11:9.
- [Google Scholar]
- Effectiveness of the ACA (Availability, Current issues and Anticipation) training programme on GP-patient communication in palliative care; a controlled trial. BMC Fam Pract. 2013;14:93.
- [Google Scholar]
- Effectiveness of the ‘availability, current issues and anticipation’ (ACA) training programme for general practice trainees on communication with palliative care patients: A controlled trial. Patient Educ Couns. 2014;95:83-90.
- [Google Scholar]





