Translate this page into:
Relationship of Quality of Life with Disability Grade in Obsessive Compulsive Disorder and Dysthymic Disorder
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
There is paucity of information on the relationship of quality of life (QOL) in obsessive compulsive disorder (OCD) and dysthymic disorder (DD) with disability grade in India.
Aim:
To assess the relation of QOL with disability level in OCD and DD.
Materials and Methods:
This hospital based study was conducted in a medical institution in Davanagere, Karnataka, India. Data was collected by using Diagnostic and Statistical Manual IV Text Revision (DSM IV TR) criteria, WHO QOL BREF and IDEAS. Relationship between disability grade and QOL was assessed by independent sample t test.
Results:
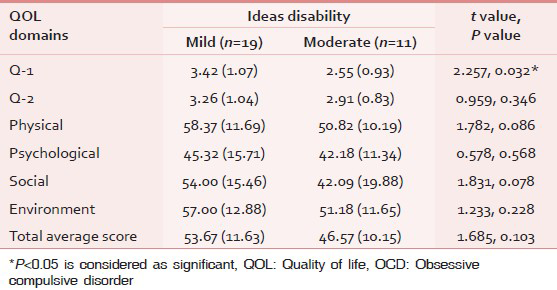
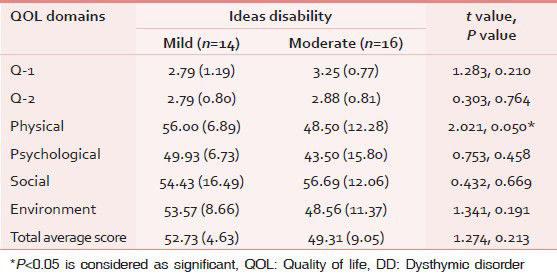
Mild disabled OCD patients had a significantly better QOL in the Q1 domain i.e. perception on quality of life as compared to moderately disabled patients (P < 0.05), while in other domains of QOL, there was no statistically significant difference (P > 0.05). But, QOL score in physical domain showed significant difference across disability grades (56.00, SD = 6.89; 48.50, SD = 12.28) in DD, but not in other domains.
Conclusion:
Perception of QOL is better in those with mild disability in OCD, but in DD, physical domain of QOL score is more in mild disability compared to moderate disability.
Keywords
Disability
Dysthymic disorder
Obsessive compulsive disorder
Quality of life
Relationship
INTRODUCTION
Psychiatric illnesses have psychosocial consequences like disability and impaired quality of life (QOL). As disability and QOL are interrelated, severe psychiatric illnesses like schizophrenia, bipolar affective disorder (BPAD), and dementia can cause severe disability and impair QOL due to their symptomatology and chronic course. Non-psychotic disorders such as obsessive compulsive disorder (OCD) and dysthymic disorder (DD) also run a chronic course and can cause disability and impair QOL. According to DSM-IV-TR criterion, obsession is recurrent and persistent thoughts, impulses or images that are experienced, at some time during the disturbance, as intrusive and inappropriate and that cause marked anxiety or distress. Compulsion is the repetitive behaviour such as hand washing, ordering, checking or mental acts like praying, counting, repeating words silently that the person feels driven to perform in response to an obsession, or according to rules that must be applied rigidly. Dysthymia refers to depressed mood for most of the day, for more days than not, as indicated either by subjective account or observation by others, for at least 2 years.[1]
Mental disability has demonstrable connection to an underlying mental disorder.[1] It is reported that OCD result in significant disability.[2] But, disability is comparatively more in schizophrenia and affects all areas of functioning.[2] Also, disease symptom severity was associated with QOL score in schizophrenia which was assessed by WHO QOL-BREF.[3] QOL is also impaired in various mental disorders.[4] In OCD, severity of obsessions and comorbid depression predict poor QOL.[5] However, there is paucity of Indian literature in the assessment of relation of disability with QOL in non-psychotic illnesses.[67] Hence, the present study assessed the relation of QOL and disability in OCD and compared it with another non-psychotic illness, DD.
MATERIALS AND METHODS
This cross-sectional hospital based study was conducted in a medical institution in Davanagere, Karnataka, India, from October 2009 to September 2011. This information is a part of main study and here we presented the relationship of QOL and disability in OCD and DD. We included 30 subjects each diagnosed with OCD and DD. DSM-IV-TR criterion was used for diagnosis of OCD and DD.
We used WHOQOL-BREF to assess the QOL in OCD and DD.[8] This instrument was used to assess the QOL in other mental disorders like schizophrenia and it was tested and validated.[3] WHO QOL BREF has four domain scores and two question items about overall perception of QOL and perception of their health. Domain scores are scaled in a positive direction. The mean score of items within each domain is used to calculate the domain score. Then the raw scores are converted into transformed scores. The first transformation method converts scores to range of 4-20 and the second transformation method converts domain scores to a final score of 0-100 scale.
Indian Disability Evaluation Assessment Scale was used to assess the disability level of the subject.[9] Disability was assessed based on the scores obtained for four areas of functioning which include self-care, inter personal activities, communication and understanding, and work along with the duration of illness of the individual. Disability was classified as no disability (0%), mild disability (<40%), moderate disability (40%-70%), severe disability (71%-99%) and profound disability (100%) based on the scores obtained.
Statistical analysis
Data was entered in Statistical Package for Social Sciences (SPSS) version 16 and analyzed by calculating mean score and independent sample t test. The findings were expressed in proportion and a P value less than 0.05 is considered as significant.
RESULTS
The mean age was found to be greater in the DD group (32.33 years, SD = 9.97) compared to the OCD group (27.33 years, 7.49). Males represented less both in the OCD group (14/30) and the DD group (12/30). Education level was more for the OCD group (20 had studied >10th standard) compared to DD (8 had studied >10th standard). All the subjects in both the groups had disease duration of 2 to 5 years preceding the study period. All of them were taking the drugs belonging to selective serotonin reuptake inhibitors regularly as prescribed in the medical college hospital.
Mildly disabled OCD patients had a significantly better QOL in the Q1 domain i.e. perception on QOL as compared to moderately disabled patients. In the domains of Q2 (perception on quality of health), physical, psychological, social and environment, there was no statistically significant difference between the mild and moderately disabled OCD patients. The OCD subjects with mild disability had greater total average QOL score and hence had a better overall QOL when compared with the moderately disabled group [Table 1]. In DD subjects, QOL score in physical domain showed statistical difference across disability grades, but not in other domains [Table 2].
DISCUSSION
This study highlights the relationship of QOL with disability level in non-psychotic disorders that include OCD and DD and found that overall QOL score is marginally more in those with mild disability compared to moderate disability in OCD and DD, but there was no statistical significance difference in QOL score. A previous study showed that severe OCD is associated with significant disability and poor QOL.[6] Another study showed that OCD with occupational disability was associated with greater functional impairment in completing household duties, social functioning, and QOL.[10] A recent review article highlighted the fact that OCD is associated with a wide range of functional impairments, and the condition has significant social and occupational liabilities.[11] The difference in the results of various other studies and this study may be due to the different methodologies adopted like instruments used for the assessment and data collection methods adopted.
But, physical domain in DD showed significant difference may be because of somatic preoccupation in DD where the subjects perceives the somatic symptoms as physical in origin and it interferes with leading and experiencing a normal life. Affective disorders comorbid with medical, somatic illnesses have a major impact on QOL and disability with more pronounced effects in DD than in major depressive disorder.[12] QOL was also significantly related to severity of anxiety, depression and measures of disability and adjustment.[13] In view of the above finding, it is important to look into the physical dimension of QOL with disability in subjects with DD.
Hospital-based cross-sectional study nature and other factors influencing the relation of disability with QOL in OCD and DD were not analyzed. It is concluded that there is marginally improved QOL in mild disability compared to moderate disability in OCD, while in DD this difference was even lesser. There is comparatively more QOL score in mild disability in OCD with respect to perception of quality of life, while in DD physical domain of QOL score is comparatively more in those with mild disability. There is a need to explore further the role of physical dimension of QOL with disability in DD.
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- Lexicon of Psychiatric and Mental Health Terms. (2nd ed). Geneva: WHO; 1994. p. :38. 71
- [Google Scholar]
- Subjective quality of life in patients with chronic schizophrenia: Relationships between psychosocial and clinical characteristics. Compr Psychiatry. 2011;52:171-80.
- [Google Scholar]
- Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA. 1995;274:1511-7.
- [Google Scholar]
- Quality of life in OCD: Differential impact of obssessions, compulsions, and depression comorbidity. Can J Psychiatry. 2003;48:72-7.
- [Google Scholar]
- Family burden, quality of life and disability in obsessive compulsive disorder: An Indian perspective. J Postgrad Med. 2008;54:91-7.
- [Google Scholar]
- Relationship of depression, disability, and quality of life in Parkinson's disease: A hospital-based case-control study. Neurol India. 2011;59:185-9.
- [Google Scholar]
- WHO QoL BREF- Field Trial Version. 1996. Available from: http://www.who.int/mental_health/media/en/76.pdf
- [Google Scholar]
- Indian Disability Evaluation and Assessment Scale (IDEAS). Ministry of Social, Justice and Empowerment Notification. 2002.
- [Google Scholar]
- Correlates of occupational disability in a clinical sample of obsessive-compulsive disorder. Compr Psychiatry. 2008;49:43-50.
- [Google Scholar]
- Multiple pathways to functional impairment in obsessive-compulsive disorder. ClinPsychol Rev. 2010;30:78-88.
- [Google Scholar]
- The effects of dysthymic disorder on health-related quality of life and disability days in persons with comorbid medical conditions in the general population. Psychother Psychosom. 2009;78:161-6.
- [Google Scholar]
- Quality of life in anxiety disorders: Its relation to work and social functioning and dysfunctional cognitions: An exploratory study from India. Asian J Psychiatr. 2012;5:309-14.
- [Google Scholar]






