Year: 2013, Volume: 19, Issue: 3, Sep-Dec
Review Article
Ken Russell Coelho
p.131-138
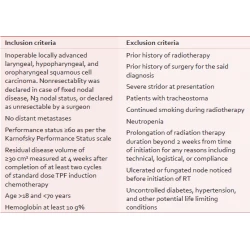
Original Article
Kailash Chandra Pandey, Swaroop Revannasiddaiah, Nirdosh Kumar Pant, Vipul Nautiyal, Madhup Rastogi, Manoj Kumar Gupta
p.139-145
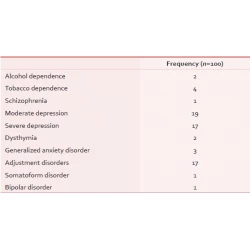
Original Article
V Rajmohan, Suresh K Kumar
p.146-151
Letters to Editor
Senthil P Kumar, Krishna Prasad, Kamalaksha Shenoy, Mariella D’souza, Vijaya K Kumar
p.198-199